1. Background
Cerebral venous sinus thrombosis (CVST) is a rare cerebrovascular disorder (1, 2), with an annual prevalence of 3 - 4 cases per million worldwide (3). The annual incidence varies from 1.16 to 2.02 per 100,000, with significant continental disparities (4). In Iran, located in Western and Central Asia, the incidence of CVST is 12.3 cases per million (5). Cerebral venous sinus thrombosis is diagnosed based on clinical grounds and confirmed by imaging findings (1), with early diagnosis playing a crucial role in disease improvement (1). Thoroughly assessing symptoms and potential predisposing factors, as well as utilizing neuroimaging studies, is essential for an early diagnosis (1). Symptoms range from headaches to loss of consciousness (6). While predisposing factors, such as pregnancy or oral contraceptive pills (OCPs), help with the diagnosis in most patients, approximately 15% of CVST cases are considered idiopathic (7). Thus, the evaluation of patients, especially those without apparent risk factors, is challenging and requires further investigation (8). Magnetic resonance imaging (MRI), magnetic resonance angiography (MRA), and magnetic resonance venography (MRV) are appropriate tools for early diagnosis (9).
Anticoagulation remains the primary treatment for patients with CVST, despite being a debatable subject due to the risk of hemorrhagic transformation in cerebral infarcts (10). For individuals with a poor prognosis and extensive thrombosis that worsens despite anticoagulation treatment, systemic or catheter-directed thrombolysis is recommended (10, 11). Cerebral venous sinus thrombosis prognosis varies from full recovery to serious neurologic consequences (12). Delay in diagnosis, especially in developing countries, is the leading cause of high mortality rates (13, 14). However, the available literature predominantly originates from developed countries (1).
2. Objectives
This study evaluated the demographics, climate patterns, clinical manifestations, risk factors, laboratory, and neuroimaging findings, as well as in-hospital mortality of patients with CVST in the Iranian population. Additionally, the mortality rate and outcomes of patients were assessed after a three-month follow-up, and factors associated with poor functional outcomes were examined.
3. Methods
3.1. Study Design and Ethics Statement
This retrospective cohort study was carried out at an academic hospital complex affiliated with Shahid Beheshti University of Medical Sciences, Tehran, Iran, with approval from the institutional review board (IRB) of the university (IR.SBMU.MSP.REC.1399.521). The study adhered to the principles of the Declaration of Helsinki (15), ensuring the protection of patient anonymity and confidentiality. The need for informed consent was waived due to the retrospective nature of the study and the anonymization of the data.
3.2. Study Population
Employing consecutive sampling, all patients meeting the following criteria were considered eligible for inclusion: (a) a confirmed diagnosis of CVST supported by both imaging and clinical symptoms, (b) the diagnosis validated by two independent expert neurologists, and (c) admission to our tertiary care referral center between April 2007 and March 2018. Patients with comorbidities such as congenital hydrocephaly and Chiari malformation were excluded.
3.3. Study Objectives
There are two objectives of this study:
(1) To describe the demographic, clinical, laboratory, and neuroimaging characteristics of patients with CVST, as well as the CVST mortality rate at discharge and after a three-month follow-up.
(2) To evaluate the factors associated with poor functional outcomes at follow-up in patients with CVST.
3.4. Study Measures
Patient data, including medical records and laboratory results, were extracted. The extracted demographic and clinical information included age, sex, time of symptom onset (categorized as acute, subacute, or chronic based on onset < 48 hours, 48 hours to 30 days, and > 30 days, respectively (16)), chief complaint, admission season, risk factors (regular steroids and OCP use for more than two weeks, pregnancy and the postpartum period, recent fasting history [defined as abstaining from food and drink for at least 12 hours within a single day during the last month], and history of thromboembolic events [deep vein thrombosis (DVT), thrombotic cerebrovascular accidents, vasculitis, previous CVST, and pulmonary thromboembolism (PTE)]), and in-hospital mortality. Laboratory measures included protein C, protein S, antithrombin III, antiphospholipid antibody (IgM and IgG), and anticardiolipin antibody (IgM and IgG). Neuroimaging studies, encompassing MRI and MRV, were conducted for all patients, with results cross-verified by a team of radiologists and neurologists who reported the involved sinus and its laterality.
3.5. Follow-up Protocol
According to the hospital guidelines, all patients are scheduled for a 3-month follow-up after their discharge. If patients cannot attend the follow-up visit, telephone interviews with the patient or their next of kin are performed up to two times. To monitor the out-of-hospital functional outcomes of patients, we used the modified Rankin scale (mRS) questionnaire, which was evaluated three months after discharge. The mRS is a validated and reliable tool for assessing the functional outcomes of patients with CVST (16, 17). Patients with an mRS score of ≤ 2 were categorized as having a favorable outcome (no disability to slight disability), while those with an mRS score > 2 were classified as having an unfavorable outcome (moderate disability to death) (16). Table 1 provides an overview of mRS grading.
| mRS | Definition | Meaning |
|---|---|---|
| 0 | No disability | No symptoms at all |
| 1 | No significant disability | Despite symptoms, capable of performing regular duties and activities. |
| 2 | Slight disability | Incapable of engaging in previous activities, but capable of managing personal affairs independently. |
| 3 | Moderate disability | In need of assistance to some extent but capable of walking independently. |
| 4 | Moderately severe disability | Incapable of walking independently and attending to personal bodily needs without assistance. |
| 5 | Severe disability | bedridden, incontinent, and requiring constant nursing care. |
| 6 | Death | N/A |
Modified Rankin Scale (mRS) Grading
3.6. Statistical Analysis
Descriptive statistics were reported as mean ± standard deviation (SD) for normally distributed numerical variables and frequency (percentage) for categorical variables. The normality of numerical variable distributions was assessed using the Kolmogorov–Smirnov test and Q-Q plots. Differences in categorical variables across groups were analyzed using chi-squared or Fisher's exact test, as appropriate. To examine and compare the distribution of numerical variables across different groups, the independent t-test was employed. No imputation was performed for missing data. All analyses were conducted using SPSS software version 18, and statistical significance was considered at a P-value < 0.05.
4. Results
4.1. Patients’ Characteristics and Mortality Rate
Table 2 provides the demographic, clinical, laboratory, and neuroimaging characteristics of patients. A total of 141 consecutive patients with CVST were enrolled, with a mean (SD) age of 38.15 (13.71) years. Most of the patients were female (69.5%). Summer (42.6%) and spring hospital admissions (14.2%) accounted for the highest and lowest hospital admission seasons, respectively.
| Variables (N = 141) | Values |
|---|---|
| Age | 38.15 ± 13.71 |
| Sex | |
| Female | 98 (69.5) |
| Season of hospital admission | |
| Spring | 20 (14.2) |
| Summer | 60 (42.6) |
| Fall | 35 (24.8) |
| Winter | 26 (18.4) |
| Chief complaint | |
| Headache | 93 (66.0) |
| Blurred vision | 5 (3.5) |
| Seizure | 19 (13.5) |
| Loss of consciousness | 7 (5.0) |
| Paresis | 11 (7.8) |
| Vertigo | 3 (2.1) |
| Imbalance | 2 (1.4) |
| Ptosis | 1 (0.7) |
| Onset of symptoms | |
| Acute (< 48 h) | 38 (27.0) |
| Subacute (48 h - 30 d) | 93 (66.0) |
| Chronic (> 30 d) | 10 (7.1) |
| Risk factors | |
| Steroid | 9 (6.4) |
| OCP b | 51 (52.0) |
| Partum/postpartum period b | 22 (22.4) |
| Addiction | 5 (3.5) |
| History of thromboembolic events | 28 (19.9) |
| History of head trauma | 6 (4) |
| Fasting | 32 (22.7) |
| Anticardiolipin IgM (n = 59) | |
| Negative | 56 (94.9) |
| Positive | 3 (5.1) |
| Anticardiolipin IgG (n = 59) | |
| Negative | 56 (94.9) |
| Positive | 3 (5.1) |
| Antiphospholipid IgM (n = 68) | |
| Negative | 67 (98.5) |
| Positive | 1 (1.5) |
| Antiphospholipid IgG (n = 69) | |
| Negative | 66 (95.7) |
| Positive | 3 (4.3) |
| Antithrombin III deficiency (n = 53) | 7 (13.2) |
| Protein C deficiency (n = 63) | 10 (15.9) |
| Protein S deficiency (n = 63) | 9 (14.3) |
| Lesion side | |
| Left | 52 (36.8) |
| Right | 71 (50.3) |
| Bilateral | 18 (12.7) |
| Involved sinus | |
| Superior sagittal | 64 (45.4) |
| Lateral transverse | 87 (61.7) |
| Sigmoid | 5 (3.5) |
| Cavernous | 4 (2.8) |
| Straight | 2 (1.4) |
| Jugular | 10 (7.1) |
| In-hospital mortality | 6 (4.3) |
| Follow-up mortality (n = 75) | 6 (8.0) |
Characteristics of Patients with Cerebral Venous Sinus Thrombosis a
Headache was the most frequent chief complaint (66%), followed by seizure (13.5%), paresis (7.8%), and reduced consciousness (5%). Most of the patients (66.0%) experienced a subacute course of the disease, followed by acute (27.0%) and chronic (7.1%) symptoms onset. More than half of the patients (52.0%) had a history of regular OCP use. Other frequently observed risk factors for developing CVST included fasting (22.7%), pregnancy/post-partum period (22.4%), and previous history of thromboembolic events (19.9%). Thrombophilic abnormalities, including protein C deficiency, protein S deficiency, and antithrombin III deficiency were observed in 15.9%, 14.3%, and 13.2% of individuals, respectively. Positive anticardiolipin IgM and IgG were found in 5.1% and 5.1% of patients, respectively. The corresponding values for antiphospholipid antibodies were 1.5% and 4.3% (Table 2).
Brain MRI was performed for all patients. Sinus involvement was unilateral in the majority (87.2%) of patients. Lateral transverse (61.7%) and superior sagittal sinuses (45.4%) were the most frequently involved sinuses. The in-hospital mortality rate was 4.3% (6/141). Three months after discharge, follow-up data was available for 75 patients. Among them, six patients passed away, indicating a three-month out-of-hospital mortality rate of 8.0%.
4.2. Patients’ Functional Outcomes and Associated Factors After a Three-Month Follow-Up
Follow-up data was available for 75 (53.2%) patients. Table 3 shows demographic, clinical, laboratory, and neuroimaging factors associated with follow-up functional outcomes according to mRS. Sixty-one patients (81.3%) exhibited a favorable prognosis with no or slight disability (mRS ≤ 2), while 14 individuals (18.7%) experienced unfavorable outcomes (mRS > 2) three months after discharge.
| Variables and Level | Favourable outcome (mRS ≤ 2; N = 61) | Unfavorable outcome (mRS > 2; N = 14) | P-Value |
|---|---|---|---|
| Age | 35.95 ± 1.42 | 52.00 ± 5.81 | 0.017 |
| Sex | 1.000 | ||
| Male | 16 (26.3) | 4 (28.6) | |
| Female | 45 (73.7) | 10 (71.4) | |
| Season of admission | 0.020 | ||
| Spring | 9 (14.7) | 2 (14.3) | |
| Summer | 31 (50.8) | 2 (14.3) | |
| Fall | 13 (21.3) | 4 (28.5) | |
| Winter | 8 (13.1) | 6 (42.9) | |
| Chief complaint | 0.028 | ||
| Headache | 44 (72.1) | 6 (42.8) | |
| Blurred vision | 2 (3.27) | 1 (7.14) | |
| Seizure | 8 (13.1) | 2 (14.2) | |
| Loss of consciousness | 1 (1.63) | 3 (21.4) | |
| Paresis | 4 (6.55) | 1 (7.14) | |
| Vertigo | 1 (1.63) | 0 (0) | |
| Imbalance | 1 (1.63) | 0 (0) | |
| Ptosis | 0 (0) | 1 (7.14) | |
| Onset of symptoms | 0.021 | ||
| Acute (< 48h) | 15 (24.6) | 7 (50.0) | |
| Subacute (48h - 30 d) | 44 (72.1) | 5 (35.7) | |
| Chronic (> 30 d) | 2 (3.3) | 2 (14.3) | |
| Risk factors | |||
| Steroid | 4 (6.55) | 2 (14.2) | 0.311 |
| OCP | 26 (42.61) | 4 (28.5) | 0.382 |
| Partum/postpartum | 13 (21.3) | 0 (0) | 0.110 |
| History of thrombosis | 8 (13.1) | 8 (57.1) | 0.001 |
| Addiction | 1 (1.63) | 2 (14.2) | 0.088 |
| Fasting | 18 (29.5) | 3 (21.4) | 0.745 |
| Anticardiolipin IgM | 1.000 | ||
| Negative | 28 (96.5) | 5 (100) | |
| Positive | 1 (3.44) | 0 (0) | |
| Anticardiolipin IgG | 0.269 | ||
| Negative | 29 (96.6) | 4 (80) | |
| Positive | 1 (3.33) | 1 (20) | |
| Antiphospholipid IgM | |||
| Negative | 29 (100) | 7 (100) | |
| Positive | 0 (0) | 0 (0) | NA |
| Antiphospholipid IgG | |||
| Negative | 30 (100) | 5 (71.4) | 0.032 |
| Positive | 0 (0) | 2 (28.5) | |
| Antithrombin III deficiency | 5 (22.7) | 1 (20) | 1.000 |
| Protein C deficiency | 5 (17.8) | 0 (0) | 1.000 |
| Protein S deficiency | 6 (21.4) | 0 (0) | 0.566 |
| Involved sinus | |||
| Superior sagittal | 24 (39.3) | 8 (57.1) | 0.247 |
| Lateral transverse | 40 (65.5) | 6 (42.8) | 0.137 |
| Sigmoid | 1 (1.63) | 1 (7.14) | 0.341 |
| Cavernous | 1 (1.63) | 2 (14.2) | 0.088 |
| Straight | 0 (0) | 0 (0) | N/A |
| Jugular | 5 (8.19) | 0 (0) | 0.577 |
| Lesion side | 0.424 | ||
| Left | 25 (40.9) | 2 (14.3) | |
| Right | 33 (54.1) | 12 (85.7) | |
| Bilateral | 3 (4.91) | 0 (0) |
Demographic, Clinical, Laboratory, and Neuroimaging Factors Associated with Functional Outcomes Three Months After Hospital Discharge a
Patients with an unfavorable outcome were significantly older compared to those with a favorable outcome (52 ± 5.81 vs. 35.95 ± 1.42, P = 0.017). Significant associations were observed between admission season (P = 0.020), chief complaint (P = 0.028), course of the disease (P = 0.021), history of thromboembolic events (P = 0.001), and antiphospholipid IgG (P = 0.032). Among patients with unfavorable three-month follow-up outcomes, 42.9% were admitted in winter, contrasting with 13.1% among those with favorable outcomes (P = 0.020). Furthermore, 21.4% of patients with poor outcomes initially presented with reduced consciousness, in comparison to 1.63% for those with a favorable outcome (P = 0.028). Acute symptom presentation was observed in 24.6% of patients with a good outcome, compared to 50.0% of those with a poor outcome (P = 0.021). Over half (57.1%) of the patients experiencing a poor outcome had a previous history of thromboembolic events, contrasting with 13.1% of patients with a favorable follow-up outcome (P = 0.001). Furthermore, while 28.5% of patients with an unfavorable outcome had a positive antiphospholipid IgG, none of those with a favorable outcome were positive for this antibody (P = 0.032).
5. Discussion
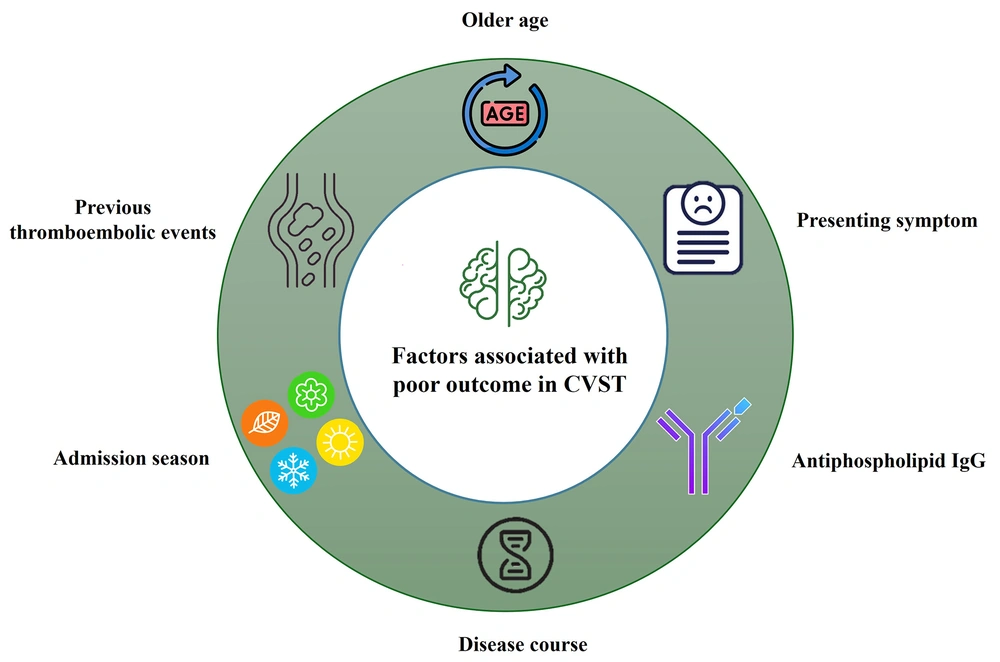
This study outlined the features of patients diagnosed with CVST and evaluated the factors associated with three-month follow-up outcomes. Most patients were admitted to the hospital in the summer. The majority of participants were female, with a female-to-male ratio of 2.28. Cerebral venous sinus thrombosis was commonly manifested in individuals in their late 30s with a subacute course. Headaches and seizures were the most common manifestations. Common clinical risk factors included regular OCP use, fasting, and the pregnancy/postpartum period. Inherited risk factors, such as deficiencies in protein C, protein S, or antithrombin III, were observed in nearly 13 - 16% of patients. The majority of patients exhibited unilateral sinus involvement, with the lateral transverse and superior sagittal sinuses being the most frequently affected. The in-hospital and three-month out-of-hospital mortality rates were 4.3% and 8.0%, respectively. Older age, winter admission, reduced consciousness, acute disease onset, history of thromboembolic events, and positive antiphospholipid IgG were associated with a poorer outcome in patients with CVST (Figure 1).
5.1. Background, Clinical Presentations, Risk Factors, and Mortality
Our findings align with the existing literature on CVST. The condition predominantly affected women (1, 2), particularly those of childbearing age (2, 3). The superior sagittal and transverse sinuses were the most affected sites, consistent with the existing literature (1, 3). Headache was the most frequently reported manifestation, and outcomes tended to be poorer when symptoms other than headaches were present (18). Contraceptive pills consumption emerged as the most common risk factor among females, consistent with numerous studies conducted in Iran (13, 19, 20). Evidence suggests that OCP consumption significantly increases the risk of venous thrombosis, with combined OCPs containing both estrogen and progesterone posing higher hazards. Notably, in individuals with a history of CVST, the use of OCPs elevates the likelihood of recurrence (21).
We observed a seasonal pattern, with an increased incidence of CVST during days with elevated temperatures; 42.6% of our patients were admitted in the summer, followed by 24.8% in the fall. There are diverse global perspectives on the seasonal patterns of this disease. The VANPORT cohort initially proposed the seasonality of CVST, indicating a peak incidence on October (22). A 2003 study by Stolz et al. suggested a bimodal prevalence, peaking in the winter and summer seasons (23). Additionally, Janghorbani et al. and Salehi et al. conducted studies on the most probable seasons for occurring CVST in Iran, identifying autumn and summer—findings that align with ours (5, 24). On the other hand, in their systematic review, Dentali et al. observed a peak incidence of venous thromboembolism, including PTE and DVT, in winter (25-27). While this aligns with numerous investigations on stroke and myocardial infarction, controversies still persist regarding the relationship between thromboembolic events and weather (25, 26).
Antithrombin III antibodies, protein C, and protein S deficiencies were observed in 13 - 16% of patients who developed CVST, aligning with a 2020 study that reported isolated antithrombin deficiency in 11.5% of patients (8). While we did not collect data on the prevalence of factor V Leiden abnormalities in this study, earlier research has suggested that the factor V Leiden mutation is a commonly observed risk factor among patients, with prevalence ranging from 12.6% to 20% (28, 29).
In line with the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT), which reported mortality rates of 4.3% at discharge, our study revealed an in-hospital mortality rate of 4.3% (30). However, we noted a higher three-month mortality rate (8.0%) compared to the mortality rate at the six-month follow-up (6.8%) observed in that study (31).
5.2. Factors Associated with Poor Outcomes
In line with our results, several studies have indicated that elderly patients with CVST have worse outcomes (24). We also observed that the majority of individuals with unfavorable outcomes (almost 71%) were admitted during autumn and winter, in contrast to a lower percentage (34%) for those with a more favorable outcome. These findings align well with W. R. Keating’s observations (24) and further support the concept of increased blood cell and platelet activity in cold weather. This correlation is consistent with the observed linear increase in mortality from coronary and cerebral thrombosis in Britain as air temperature decreased from summer to winter (32). Altered mental status at presentation was also linked to a poorer prognosis, a result consistent with prior studies (33). According to Masuhr et al., the most crucial prognostic factors, aside from the underlying condition, include the clinical presentation upon hospital admission and the findings from neuroimaging investigations (33). Furthermore, we noted a higher incidence of acute presentations in patients with an unfavorable outcome compared to those with a favorable outcome. Studies consistently have indicated that pathophysiological differences between acute and subacute CVST may lead to varying prognoses based on factors such as symptom onset, reversibility, and response to heparin therapy (34). However, there is a lack of evidence specifically comparing the prognosis of these two subtypes, necessitating future endeavors to ascertain whether there exists a notable difference in the prognosis between acute and subacute CVST. Another finding of this study was the association between a history of thromboembolic events and poorer outcomes, which accords with the findings from ISCVT (27). Regarding the observed association between antiphospholipid IgG and patients’ outcomes, while research suggests a link between antiphospholipid antibodies and CVST (35), additional studies are required to fully understand the impact of antiphospholipid IgG on CVST outcomes.
5.3. Limitations and Strengths
Our study has various limitations. Firstly, although we gathered data on patients with CVST during an 11-year period of admission, the small sample size reduces the statistical power of the study. Therefore, the absence of statistical significance in some variables does not necessarily rule out their association with the mRS score. The single-center nature of the study and the unadjusted analyses reduce the generalizability of the study’s findings. Additionally, the retrospective design is susceptible to selection and information bias. To address selection bias, we included “all” eligible patients during the study period consecutively. To mitigate potential information bias, those assessing medical records and patient outcomes were unaware of the specific research question. Lastly, follow-up information was not available for a considerable proportion of patients. Despite these limitations, our findings align with larger cohort studies and contribute to the literature on clinical and laboratory associations with poorer outcomes in CVST patients.
However, the study has its strengths. Considering the rarity of the condition, the inclusion of 141 patients represents a reasonable sample size. Conducting studies with larger samples or employing prospective designs for such a rare condition would be labor- and time-intensive.
5.4. Conclusions
Our study revealed that CVST predominantly manifested during the summer, particularly affecting women in their late 30s with a subacute disease course. Headaches emerged as the most prevalent clinical manifestation. Regular OCP use and fasting were the most frequent clinical risk factors, and inherited thrombophilia was identified in 13 - 16% of patients with CVST. The superior sagittal and lateral transverse sinuses were the most affected locations, and the survival rate at discharge was generally better than previously thought (95.7%). However, there was an 8.0% mortality rate after a three-month follow-up. Factors such as older age, season of hospital admission, presenting symptoms, disease course, history of thromboembolic events, and antiphospholipid IgG were associated with patients’ outcomes.
These findings suggest increased caution for reproductive-age females with headaches, particularly those with a history of OCP use or fasting/dehydration. Additionally, close monitoring is recommended for older patients with reduced consciousness, an acute disease course, and a history of thromboembolic events or positive antiphospholipid IgG to prevent adverse outcomes.