1. Background
Stroke, including ischemic and hemorrhagic types, is the second leading cause of death globally and the third leading cause of death and disability (1), and it is one of the most important healthcare issues worldwide (2). Stroke is the second main cause of dementia (3). It is a neurological disorder caused by a blockage in the blood vessels. Clots form in the brain, disrupting blood flow, which can clog arteries or cause blood vessels to break, leading to bleeding. When the arteries supplying the brain rupture during a stroke, it results in the sudden death of brain cells due to a lack of oxygen (4). Neurological symptoms arise from the involvement of the central nervous system and disturbances in cerebral blood flow.
Several factors increase the risk of stroke, including hypertension, heart disease, diabetes, smoking, and high blood lipid levels. Other contributing factors, such as systemic diseases that lead to increased blood coagulability and the use of oral contraceptive pill (OCP), play a lesser role. The most significant risk factor for stroke is either systolic or diastolic hypertension. Strokes can generally be categorized into two main types: Ischemic and hemorrhagic. Statistics indicate that 85% of strokes are due to cerebral ischemia (5).
The effects of stroke can vary, with about one-third of patients dying, another third recovering with minor issues, and the remaining third experiencing moderate to severe problems such as motor, sensory, cognitive, and speech impairment. Most patients also experience personality changes and emotional adjustments (6, 7).
China has the highest stroke burden in the world, with an age-standardized prevalence rate of 1115, an incidence rate of 247, and a mortality rate of 115 per 100,000 person-years (8). The data indicate that the prevalence of stroke in China is relatively low compared to that in high-income countries. However, China still has one of the highest incidence and mortality rates for stroke worldwide. While the incidence of stroke is declining in high-income countries, including the United States, the situation in China remains concerning (4, 8, 9).
In the United States, approximately 795,000 strokes occur annually, with around 610,000 being first-time strokes and 185,000 recurrent strokes (10). The southeastern United States, known as the "stroke belt", has higher rates of stroke incidence, prevalence, and mortality than the rest of the country (11-14).
In 2019, Iran recorded a total of 963,512 prevalent stroke cases, with 102,778 new cases and 40,912 deaths attributed to strokes (15). Of these, 88.1% were ischemic strokes, 12% were intracerebral hemorrhages, and 4.7% were subarachnoid hemorrhages. Stroke incidents rose from 48,274 in 1990 to 102,778 in 2019, a 2.1-fold increase. All provinces, except Ilam, which had a 0.4% increase, experienced a decline in stroke incidence rates for both males and females (15).
To reduce the population’s stroke burden, it is essential to identify modifiable risk factors and prove the effectiveness of risk reduction strategies. Stroke risk factors include both modifiable (e.g., diet, comorbid conditions) and non-modifiable factors (e.g., age, race) (16). Given the increasing number of patients exhibiting stroke symptoms, including decreased levels of consciousness, severe headaches, changes in pupil size, and drooping of the face, this study seeks to assess the relative frequency of stroke risk factors in Yasuj. Furthermore, a similar study has not been conducted in the province before (17-20).
2. Methods
This descriptive cross-sectional study was conducted on patients referred to Shahid Beheshti Hospital, Yasuj city, Kohgiluyeh and Boyer Ahmad provinces, Iran, in 2022 - 2023 with stroke confirmed by a neurologist. After the University Research Committee approved the plan and the code of ethics was received from the ethics committee (IR.YUMS.REC.1399.077), the relevant hospital was approached. The questionnaire and related questions were completed after explaining the study and obtaining informed consent from the patients.
All patients referred to Shahid Beheshti Hospital with a stroke diagnosis were evaluated by a specialist neurologist who determined the stroke type and cerebral circulation involved based on the patient's CT scan. Information was gathered by administering a questionnaire to patients and subsequently extracting data from their clinical records or the hospital information system, thus completing the required information for the research.
The inclusion criteria included patients at least 25 years of age and confirmation of stroke by a neurologist. Exclusion criteria included pregnant women, lack of consent to participate in the study, and a change of mind by the patient during the study, which were necessary to continue participation. The required number of samples was 58, and the sampling method was consecutive. Patient information — including age, gender, medical history of blood pressure and diabetes, and clinical symptoms — was recorded in a dedicated questionnaire. A neurologist noted the type of stroke, the involved blood circulation, and the affected nerves. The collected data were analyzed and reported using SPSS 18 software and descriptive statistics.
- In this study, a low-fat diet is defined as a diet that restricts the intake of calories from fat. This approach may offer some advantages over other methods for helping people lose weight. However, there are generally few, if any, additional health benefits associated with low-fat diets (21).
- A healthy sodium level in a diet is less than 2.3 grams (2,300 milligrams), which is about the amount of sodium found in one teaspoon per day. Consuming less than this amount is considered a low-salt diet (22).
3. Results
The present study was conducted to investigate the relative frequency of stroke risk factors in patients referred to Shahid Beheshti Yasuj Hospital in 2022 - 2023. This included 58 patients whose stroke was confirmed by brain CT scan and neurologist's opinion. In this study, 28 cases (48.3%) were male and 30 cases (51.7%) were female. The mean age of the patients was 65.46 years, with a standard deviation of 14.72 years. The ages ranged from a minimum of 29 years to a maximum of 92 years. The largest group of patients, accounting for 37.9%, was between the ages of 55 and 70. Additionally, 58.6% of the participants did not have a formal education background. Most of the patients (91.4%) were unemployed, and 79.3% were married (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 28 (48.3) |
| Female | 30 (51.7) |
| Age | |
| 25 - 40 | 2 (3.4) |
| 40 - 55 | 13 (22.4) |
| 55 - 70 | 22 (37.9) |
| 70 - 85 | 15 (25.9) |
| 85 - 100 | 6 (10.4) |
| Education | |
| None | 34 (58.6) |
| Elementary school | 13 (22.4) |
| Secondary education | 2 (3.5) |
| Diploma | 7 (12.1) |
| Advanced diploma | 1 (1.7) |
| Master | 1 (1.7) |
| Occupation | |
| Employed | 5 (8.6) |
| Unemployed | 53 (91.4) |
| Marital status | |
| Married | 46 (79.3) |
| Widowed | 11 (19) |
| Single | 1 (1.7) |
Prevalence of Stroke by Gender, Age, Education, Occupation, and Marital Status
Among the patients surveyed, 82.8% were non-smokers, while those who smoked had an average smoking history of 28.6 pack-years. Additionally, a significant majority (98.3%) did not consume alcohol, with only one individual drinking occasionally. Moreover, a large portion of the patients (44.8%) reported frequently or always following a low-salt diet, and 36.2% of stroke patients often adhered to a low-fat diet (Table 2).
| Variables | No. (%) |
|---|---|
| Number of cigarette consumption (pack/y) | |
| 0 | 48 (82.8) |
| 1 - 10 | 2 (3.5) |
| 11 - 20 | 1 (1.7) |
| 21 - 30 | 4 (6.9) |
| 31 - 40 | 1 (1.7) |
| 41 - 50 | 1 (1.7) |
| 51 - 60 | 1 (1.7) |
| Opium consumption | |
| Yes | 3 (5.2) |
| No | 55 (94.8) |
| Alcohol consumption | |
| Yes | 1 (1.7) |
| No | 57 (98.3) |
| Salt consumption | |
| Never | 37 (63.8) |
| Rarely | 5 (8.6) |
| Occasionally | 10 (17.25) |
| Often | 6 (10.35) |
| Always | 0 (0) |
| Low-fat diet | |
| Never | 10 (17.25) |
| Rarely | 18 (31.03) |
| Occasionally | 0 (0) |
| Often | 21 (36.2) |
| Always | 9 (15.52) |
Prevalence of Stroke by Smoking Habits, Alcohol Consumption and Dietary Habits
In this study, a majority of stroke patients (63.8%) were found to have high blood pressure. Additionally, 25.9% of the stroke patients had diabetes, while 31% had a history of hyperlipidemia. Furthermore, 37.9% of patients reported a history of vascular diseases, and 41.4% had a history of heart disease. Among those with heart disease, 79.2% had experienced structural heart problems, whereas 20.8% had a history of arrhythmias. Notably, most stroke patients (84.5%) did not have a history of migraines. Lastly, over half of the participants (51.7%) were classified as overweight, with a Body Mass Index (BMI) between 25 and 30 (Table 3).
| Variables | No. (%) |
|---|---|
| High blood pressure | |
| Yes | 37 (63.8) |
| No | 21 (36.2) |
| Diabetes | |
| Yes | 15 (25.9) |
| No | 43 (74.1) |
| Hyperlipidemia | |
| Yes | 18 (31) |
| No | 37 (63.8) |
| Undiagnosed | 3 (5.2) |
| Vascular disease | |
| Yes | 22 (37.9) |
| No | 36 (62.1) |
| BMI | |
| 18 - 24.9 | 15 (25.9) |
| 25 - 29.9 | 30 (51.7) |
| 30 - 35 | 12 (20.7) |
| 35 < | 1 (1.7) |
| Migraine disease | |
| Yes | 9 (15.5) |
| No | 49 (84.5) |
| History of heart disease | |
| Yes | 24 (41.4) |
| No | 34 (58.6) |
| Type of heart disease in people who had heart disease | |
| Arrhythmias | 5 (20.8) |
| Structural | 19 (79.2) |
Prevalence of Stroke by Clinical and Medical History
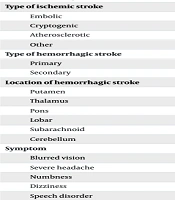
In terms of type of stroke, 77.6% of cases were ischemic and 22.4% were hemorrhagic. Of the ischemic stroke cases, 57.8% were cryptogenic. The type of hemorrhagic stroke in patients was only of the primary type. The frequency of hemorrhagic stroke in the thalamus area was 46.2%, which was the most prevalent. The most common symptom of stroke patients upon hospital admission was paresis (43.1%), while dizziness accounted for the least (1.7%) cases (Table 4). Most (93.8%) female patients with stroke had no history of OCP use.
| Variables | No. (%) |
|---|---|
| Type of stroke | |
| Ischemic | 45 (77.6) |
| Hemorrhagic | 13 (22.4) |
| Type of ischemic stroke | |
| Embolic | 9 (20) |
| Cryptogenic | 26 (57.8) |
| Atherosclerotic | 5 (11.1) |
| Other | 5 (11.1) |
| Type of hemorrhagic stroke | |
| Primary | 13 (100) |
| Secondary | 0 (0) |
| Location of hemorrhagic stroke | |
| Putamen | 1 (7.7) |
| Thalamus | 6 (46.1) |
| Pons | 1 (7.7) |
| Lobar | 1 (7.7) |
| Subarachnoid | 2 (15.4) |
| Cerebellum | 2 (15.4) |
| Symptom | |
| Blurred vision | 2 (3.5) |
| Severe headache | 9 (15.5) |
| Numbness | 8 (13.8) |
| Dizziness | 1 (1.7) |
| Speech disorder | 5 (8.6) |
| Impaired level of consciousness | 4 (6.9) |
| Paresis | 25 (43.1) |
| Ataxia | 4 (6.9) |
Prevalence of Stroke by Stroke Characteristics and Symptoms
4. Discussion
The study aimed to investigate the prevalence of stroke risk factors in patients referred to Shahid Beheshti Yasuj Hospital from 2022 to 2023. Research by Potter et al. reveals that cryptogenic strokes in young people often have variable and unclear causes. The incidence of strokes varies by gender and age: Women are more affected before age 35, while men show a higher incidence after age 45. This trend aligns with the increase in traditional vascular risk factors, implying that physiological differences between the genders may play a role in the heightened risk (1).
In Lotfi et al.’s study (23), the mean age of the patients was 68 years with a standard deviation of 16.56 years, while in Mojarrab et al.’s study (24), the mean age was 70 years with a standard deviation of 13 years, which is almost similar to the present study. In terms of gender, the mean age for men was 66.60 years with a standard deviation of 12.81 years, and for women, it was 64.40 years with a standard deviation of 16.45 years. In Mazaheri et al.’s study (25), the average age for men was 64.18 years and for women was 67.83 years, while in our study, contrary to Mazaheri et al.’s findings, men had a higher average age than women.
In a study conducted by Ebrahimi-Rad et al. on those aged 61 - 80 (26), and Mazaheri et al. on individuals aged 60 - 69 (25), it was found that the prevalence of stroke was highest in these age groups, consistent with the findings of the present study. Similar to other research, it can be inferred that advancing age is a significant risk factor for stroke, with the risk increasing as age advances. Therefore, the study suggests that the risk of stroke is highest in the seventh decade of life.
In Lotfi et al.’s study (23) and Mazaheri et al.’s study (25), the percentage of smokers among patients was higher compared to the smoking rate in this study. Blomstrand et al. (27), Owolabi et al. (28), and Wang et al. (29) have linked smoking to an increased risk of stroke. Substances like opium, cigarettes, and other drugs, apart from leading to dependence, which itself is a major social, personal, and cultural problem, can have various effects on the body’s physiology, immune system, and coagulation system, including plasma fibrinogen, and may potentially impact the incidence of strokes.
In this study, a small percentage of people reported drinking alcohol. However, in Ahangar et al.’s study, 28.1% of patients were found to consume alcohol (30). Additionally, case-control studies conducted in 2007 (31) and 2016 (32) identified alcohol consumption as a significant risk factor for stroke. It was also noted that high alcohol consumption increases the level of certain fats (triglycerides) in the blood. This variation may be attributed to the religious beliefs of Islamic society, which prohibits alcohol consumption.
In Lotfi et al.’s study, 74% of stroke cases were ischemic, while 26% were hemorrhagic (23). In Ahangar et al.’s study, 93.8% of cases were ischemic, and 6.2% were hemorrhagic strokes (30). Additionally, in Mazaheri et al.’s study, 80% of cases were ischemic, and 20% were hemorrhagic (25). These findings are consistent with the present study, which also found a higher frequency of ischemic stroke compared to hemorrhagic stroke. In Ahangar et al.’s study, most cases of ischemic stroke were of embolic type (30), which is different from the present study. The anterior circulation system of the brain accounted for the most involved cases, and all the cases of hemorrhagic stroke were of the primary type. The most frequently involved site among hemorrhagic stroke cases was the thalamus, with other involved sites including putamen, pons, lobar, subarachnoid, cerebellum, and caudate.
In patients with stroke, high blood pressure and old age are common. It’s recommended for these individuals to have a low-fat, low-salt diet. Salt consumption is linked to high blood pressure, a significant risk factor for stroke. The daily recommended salt intake is 2.4 grams. For those over 50, individuals with high blood pressure, or heart failure, the recommended intake is 1.5 - 2 grams. In a study conducted by Owolabi et al., it was found that 31.1% of strokes were linked to regular consumption of red meat. Additionally, research has shown that high consumption of red meat is associated with increased risk of high blood pressure and hyperlipidemia, both of which are proven stroke risk factors (28).
The following statistics were reported in various studies: Ebrahimi-Rad et al. found that 73% of patients had high blood pressure (26), Lotfi et al. found 56.75% (23), Ahangar et al. found 35.4% (30), Mazaheri et al. found 54.24% (25), Mojarrab et al. found 71% (24), and Madsen et al. found 70.1% (33). Owolabi et al.’s study showed that 90.8% of strokes are related to high blood pressure (28), and Wang et al.’s study identified high blood pressure as the strongest independent risk factor for stroke (29). These findings underscore the importance of controlling and preventing high blood pressure in reducing the incidence of stroke, which can be achieved in part through screenings and national health programs.
In Lotfi et al.’s research, 64.86% of patients had a history of diabetes (23). Ebrahimi-Rad et al. found that 31% of patients had a history of diabetes (26), Ahangar et al. reported 20% (30), and Mazaheri et al. reported 19.01% (25). Owolabi et al. found that 22.1% of strokes were associated with diabetes (28), and Blomstrand et al. associated a history of diabetes with an increased risk of stroke (27). Despite the different frequencies of diabetes in different studies, having a history of diabetes is known to be an important risk factor for stroke.
The research findings show that hyperlipidemia prevails at a rate of 13.51% in Lotfi et al.’s study (23), 54% in Ebrahimi-Rad et al.’s study (26), 23.1% in Ahangar et al.’s study (30), and 18.42% in Mazaheri et al.’s study (25), which aligns with the findings of the present study. Owolabi et al. have associated a 35.8% occurrence of stroke with hyperlipidemia (28), and other studies also identify dyslipidemia as a risk factor for stroke.
The studies by Mazaheri et al. (25) and Ebrahimi-Rad et al. (26) found that one-third of stroke patients had a history of heart diseases such as ischemic heart diseases, arrhythmia, valve stenosis, etc. However, Owolabi et al.’s study (28) minimized the relationship between stroke and heart disease. Nevertheless, these results collectively suggest that a history of heart disease is a risk factor for stroke. Additionally, Blomstrand et al. and Madsen et al.’s studies (27, 33) demonstrated that atrial fibrillation is a moderate risk factor for stroke.
Carrying excess weight not only increases the likelihood of high blood pressure and diabetes but also significantly raises the risk of stroke. According to Blomstrand et al.’s study, a high BMI is strongly associated with an elevated risk of stroke (27).
4.1. Conclusions
Awareness of risk factors can play a significant role in the prevention of both the primary and secondary levels of the disease. In this study, a large number of individuals had more than one risk factor, highlighting the multifactorial nature of stroke and the need for detailed diagnostic examinations and evaluations to identify underlying risk factors. Given the high prevalence of stroke among the elderly, along with its complications and significant economic and social costs, it is essential for medical professionals and health system planners to familiarize themselves with these related risk factors to effectively control and mitigate the risk.