1. Introduction
Vaginal bleeding in pre-pubertal girls is a major concern among pediatric urologists and gynecologists, because it may represent important underlying conditions such as tumors. Sexual abuse and foreign bodies are the other reasons of vaginal bleeding. Vaginal bleeding in children may have various etiologies such as sexual abuse, trauma, vulvovaginitis, endocrine abnormalities, lichen sclerosis, urethral prolapse, blood dyscrasia, haemangioma, tumors and foreign bodies. Foreign bodies in the vagina lead to severe inflammation and result in vaginal bleeding or blood-stained and foul-smelling discharge.
In this case report we present a three years-old girl, who was referred to our center, with abnormal vaginal bleeding.
2. Case Presentation
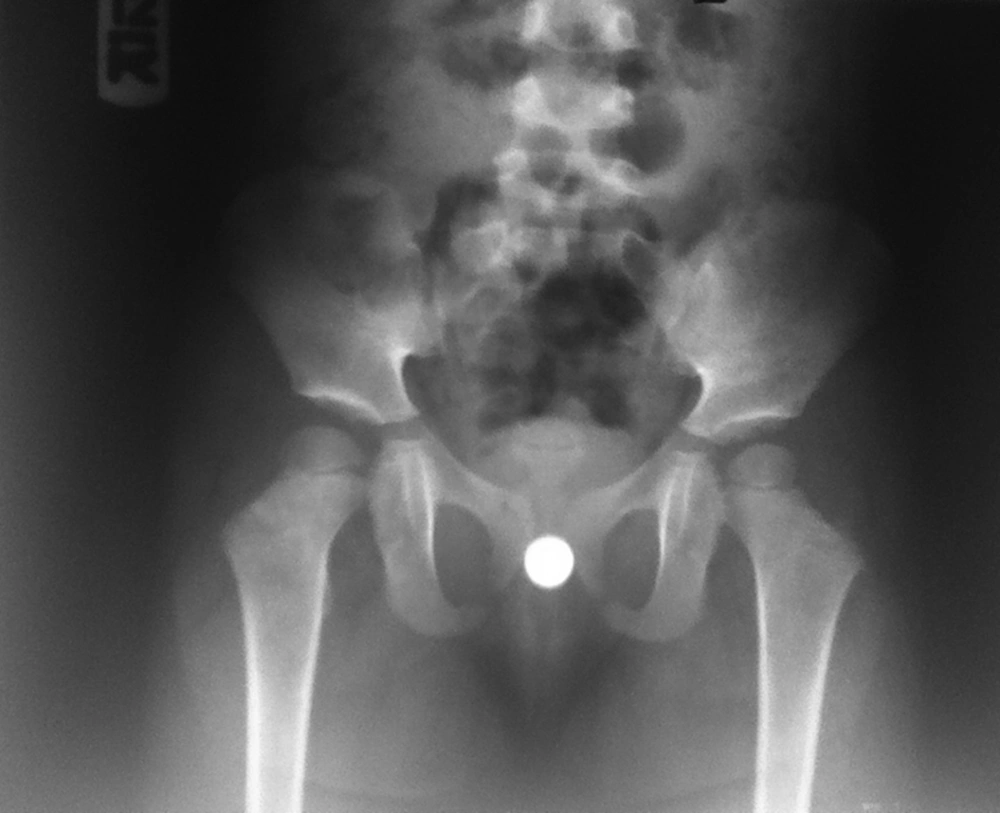
A three-year-old girl was referred to our pediatric urology clinic with chief complain of bloody discharge which increased by defecation, for more than one week. Her mother denied a history of any foreign body insertion or sexual abuse. She did not have any pruritis or voiding dysfunction. She did not take any medication. Also, her past medical and surgical histories were unremarkable. Vital signs were stable and she was afebrile at the time of admission. Chest and cardiovascular system examinations were normal. She had normal female external genitalia with no sign of erythema, skin inflammation or excoriation. Pelvic and urinary system sonography excluded any underlying pathologies such as malignancy. Pelvic X-ray revealed a round radio-opaque object in her pelvic cavity which was compatible with a button battery (Figure 1).
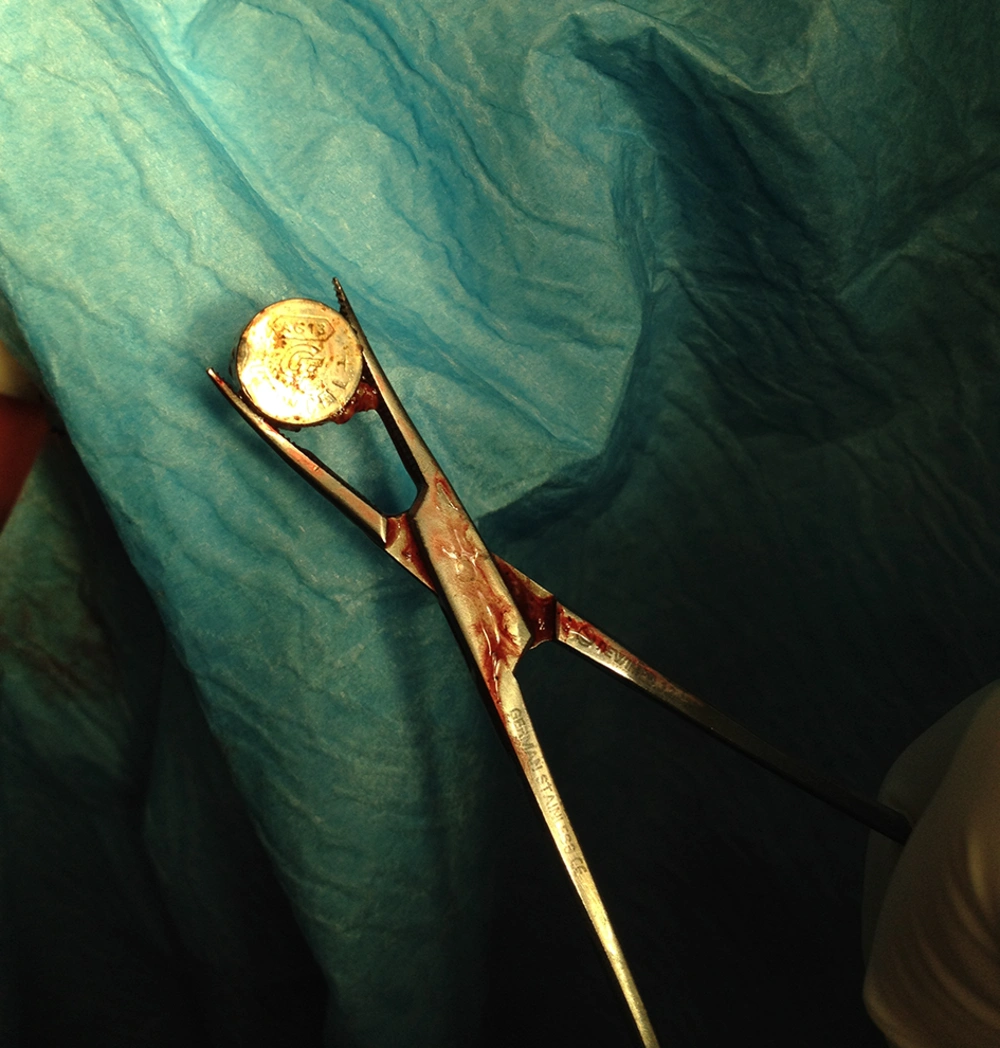
The patient was admitted for examination under general anesthesia. First we performed cystoscopy by a 6 Fr. cystoscope, but we did not find any bladder abnormalities. Furthermore, the vaginoscopy confirmed a round metal object embedded to the posterior fornix covered with necrotic tissue and surrounded by sever vaginal burn. Following vaginal irrigation by normal saline through the cystoscope the button battery was visible and the battery was pushed and fixed upward by a digital rectal maneuver in order to be grasped by Mosquito forceps and removed following installation of 5 mL of sterile lubricant gel by gentle traction (Figure 2). The object was a discolored 1 cm diameter battery. Repeated gentle vaginoscopy confirmed a type III coin shaped burn with no fistula to the rectum. The hymen was elastic and intact following removal of the foreign body. We finished the procedure following vaginal irrigation with diluted povidone-iodine solution and installation of gentamycin eye ointment into the vagina. Besides, we prescribed laxative (milk of magnesia) in order to facilitate a soft stool rectal passage. During her post-operative days she did not have fever or any systemic signs.
Finally, she was discharged on the third post-operative day with no vaginal bleeding and good general condition. She was examined as an outpatient after two weeks. On examinations, there were no signs or symptoms of rectovaginal fistula (e.g. passage of gas, stool or pus from the vagina, malodorous vaginal discharge, vaginal or urinary tract infections, irritation or pain in vulva, vagina or perineum), vaginal discharge either bloody or non-bloody, voiding difficulties, etc. Our follow up revealed complete healing after two weeks.
3. Discussion
When vaginal bleeding occurs in children, complete examination is required. An appropriate inspection of the perineum region could be achieved in a child with a frog-leg position. If further examinations are needed, or if the upper vagina must be examined to exclude important underlying conditions (e.g. trauma or tumors), examination should be performed under general anesthesia. Small diameter vaginoscopy allows adequate endoscopic examination of the vaginal canal and cervix (1).
Vaginal bleeding in children may have various etiologies such as sexual abuse, trauma, vulvovaginitis, endocrine abnormalities, lichen sclerosis, urethral prolapse, blood dyscrasia, haemangioma, tumors and foreign bodies (2). Foreign bodies in the vagina lead to severe inflammation and result in vaginal bleeding or blood-stained and foul-smelling discharge (3).
In another report, McAllister and Gudson reported an intravaginal foreign body in an eleven-year-old girl with foul smelling discharge and vaginal bleeding. By incision of the fibrotic zone after dilation, a flash light bulb was removed (4). Also, Wu et al. reported a case of an eight-year-old girl who presented bloody and stench vaginal discharge for more than four years. Multiple imaging modalities (e.g. pelvic x-ray, ultrasound abdomen and MRI of the pelvis) failed to find any evidence; yet vaginography revealed an intravaginal filling defect by incision through the scarred zone; two foreign bodies, a round plastic tube and a cap were removed (5).
According to the studies performed by Di Meglio et al. Paradise et al. and Deligeoroglou et al. 4% - 5% of all outpatient pre-pubertal girls with gynecological complaints had complications resulting from vaginal foreign bodies (6-8). In another study, Capraro et al. concluded that the incidence of vaginal foreign bodies among pre-pubertal girls with vaginal bleeding or bloody discharge is about 10% (9). However, Stricker et al. reported that 50% of the girls with vaginal foreign bodies presented either vaginal bleeding or blood stained vaginal discharge (10). In the study performed by Di Meglio et al. 93% of patients who had vaginal foreign bodies presented with spotting, bleeding, or blood-tinged discharge, and 82% of patients with vaginal bleeding had vaginal foreign bodies. Additionally, non-bloody (greenish) discharge is much less common (6).
Paradise et al. used Bayes' theory to assess the probability of vaginal foreign bodies in girls with genitourinary complaints. Bayes' theory acknowledges that, about 18% of pre-pubertal girls with vaginal bleeding, either with discharge or otherwise, and 50% of those with bleeding but no discharge will affirm to have vaginal foreign bodies. They reviewed 17 premenarcheal girls who had foreign bodies and they reported that patients with foreign bodies presented vaginal bleeding more frequently than discharge (7).
According to the study of Smith et al. foreign bodies were the cause of persistent vaginal discharge in about 10% of girls who had referred to the clinic. They noticed that vaginal irrigation was very beneficial especially in older children, because it was more feasible in this age group. However, all of the foreign bodies were removed by irrigation only after they were visually identified. Such identification was achieved through examination under anesthesia and vaginoscopy (11).
Previous studies reported rolled pieces of toilet tissue as the most common foreign body found in pre-adolescent vaginas. However, hard objects such as lead pencils, pen caps, bottle caps, small plastic toys, safety pins, wax crayons, coins and stones were documented as other important causes of vaginal bleeding (2, 3). Distal vagina-located foreign bodies (e.g. vaginal introitus) can be removed or washed out. Diagnosis and removal of foreign objects, which are located proximal to the vagina or embedded in the vaginal wall, usually require vaginoscopy. Usually, a single irrigation of the vagina with povidone-iodine is recommended after removal. In this regard, Baldwin and Landa noticed that viscous lidocaine, followed by the insertion of a 10-12 Fr. Foley catheter, then irrigation with povidone-iodine solution in order to wash out the foreign body, was the treatment of choice (12). Previous authors indicated that in most patients, the problem is resolved without additional treatment (e.g. sitz baths and local estrogen cream application) (13).
The consequences of a long remained intravaginal foreign body may include infection, vaginal stenosis and traumatic laceration. Additionally, late sequels may result pelvic inflammatory disease, intrauterine synechiae, pelvic adhesions and infertility. In this case, the late consequence may perhaps be intense inflammation, fibrosis and recto-vaginal fistula due to battery reactions with the vaginal wall (10, 14).
We conclude that in girls who present vaginal discharge and bleeding, the probability of retained foreign body or malignancy should be strongly considered.