1. Background
Rhinitis is a chronic symptomatic nasal mucosal inflammation. This is one of the most prevalent reasons for referring to otorhinolaryngologists, involving approximately 10-30% of adults (1, 2). The symptoms are cyclical, seasonal or permanent (3, 4); they are annoying and in many cases serious and debilitating. According to the literature, hyperemia and nasal obstruction are the most annoying chronic symptoms of this disease, which have led to lowering the quality of life (1, 5, 6).
Nasal breathing plays a crucial role in maintaining the physiology of the upper and lower respiratory systems. Nose has a significant role in moisturizing, warming and filtering the incoming airstream. One of the most common causes of nose hyperemia is hypertrophy of inferior nasal turbinate (7). Inferior turbinate hypertrophy (ITH) is a cause of nasal obstruction, which might be due to inflammation, infection, or medical reasons (8). Nasal obstruction due to ITH leads to irreversible obstruction and may interfere with normal function of the nose (1, 6). The cases with ITH that are resistant to medical intervention are the main problems among these patients (6).
Most cases with ITH get treated with local treatments and oral antihistamine (7, 9-11). But in cases that are resistant to medical intervention inferior turbinate surgery is suggested (12). There are different techniques for this procedure such as turbinectomy, turbinoplasty, extra and submucosal electrocautery, radiofrequency, resection with laser, and cryosurgery (11, 12). Although none of the aforementioned techniques have been established as the optimal treatment for inferior turbinate hypertrophy surgery, radiofrequency have recently gained momentum since it can be easily repeated with only local anesthetics needless of packing the nose (11). The heat generated during radiofrequency makes it possible to reduce the volume without harming the lining mucus, ending in less nasal obstruction (13, 14). Although complications from radiofrequency can create post-operative inconveniences such as edema for patients, using this technique increases the chance to recover from nasal obstruction due to inferior nasal turbinate (15). Using radiofrequency can be productive in reducing the obstruction and hyperemia caused by inferior nasal turbinate as well as other rhinitis symptoms and improving the quality of life (15-17).
2. Objectives
Worldwide, a few studies have compared radiofrequency and medical approaches. Therefore, the present study was designed to assess the effects of radiofrequency and to compare them with those of nasal corticosteroid spray during a 6-month follow-up, to complement the existing studies and determine the preferred treatment.
3. Patients and Methods
This randomized clinical trial was approved by Baqiyatallah University of Medical Sciences (BMSU) Ethics Committee (No. 34-15 at meeting 2014-01-05) and Iranian Registry of Clinical Trials (IRCT2014042417413N1). Patients with ITH due to allergic rhinitis, referred to BMSU allergy clinic, were enrolled in the study. Allergic rhinitis was approved by clinical examination (ITH and pale mucus), patients' history (rhinorrhea, nasal obstruction and family history), and diagnostic tests such as rhinomanometry. Patients with other obstructive lesions (e.g. polyp and tumor), severe septal deviation, asthma, cigarette smoking, chronic rhinosinusitis, history of other medical therapies, and history of sinus and nasal surgeries, were excluded. Written informed consents were obtained from all patients. Patients were randomly assigned to radiofrequency (RF) and intranasal corticosteroid (INS) groups by a computer-generated list.
Radiofrequency was performed under local anesthesia with 10% lidocaine in three point of the inferior turbinate (the first point was in front of inferior turbinate and parallel to septum, the second point parallel to palmistry, and the third point 2 cm posterior to other two points), two punctures in each point. The total dose of RF was 1500 ± 200 Joules (300-359 Joules in each step), and all the procedures were performed by one specialist. After the procedure, patients were discharged immediately without any limitation in daily activities and a nasal decongestant was prescribed for three days. For the INS group, fluticasone 125 µg intranasal spray was prescribed twice a day and every time one puff in each side of the nose. Patients were evaluated by rhinoscopy, nasal obstruction severity score (0-10 VAS score), and rhinomanometry tests, at first, third and sixth months after the intervention. Rhinomanometry was accomplished for nasal airflow and obstruction severity. Its score, reported by each person, predicted the nasal airflow percentage.
3.1. Statistical Analysis
Data were analyzed by statistical package for social sciences (SPSS) version 21 (SPSS Inc. Chicago, IL) for windows. Normal distribution variables were approved by one-sample Kolmogorov–Smirnov (KS) test. Normal variables were compared using independent sample t-test between the groups and paired sample t-test within the groups. Nonparametric tests (Mann-Whitney U test between the groups and Wilcoxon test within the groups) were used for non-normal distribution variables. Qualitative variable were compared by chi square and Fisher’s exact tests in the two groups. P values less than 5% were considered significant.
4. Results
Sixty patients with mean age of 36.52 ± 8.86 years old were included (30 patients in each group). Among them, 20 were male and 34 were female with the mean body mass index (BMI) of 22.97 ± 3.12 kg/m2. There were no significant differences in demographic data between the two groups, as shown in Table 1 (P > 0.05).
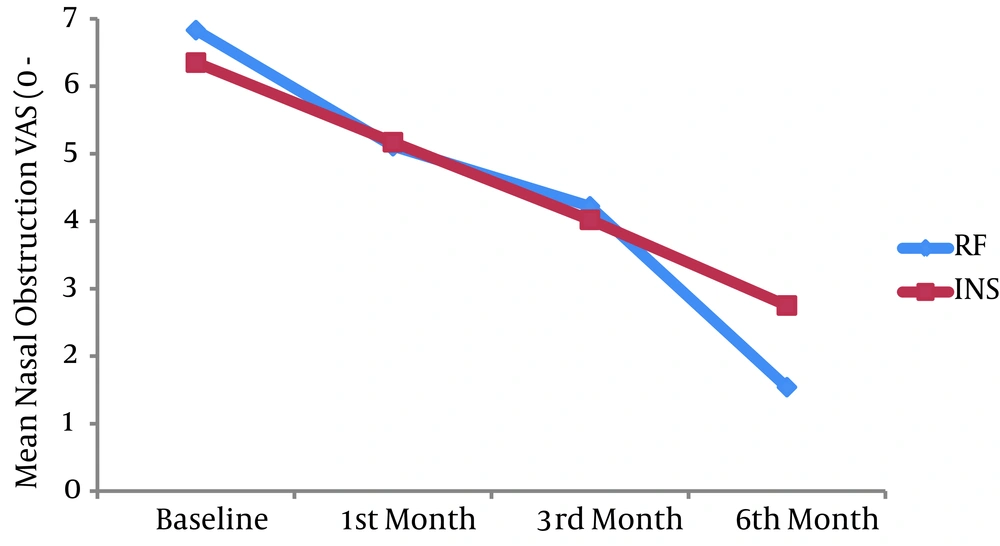
The mean nasal obstruction visual analogue scale (VAS) score was 6.83 ± 0.52 in the RF group and 6.35 ± 1.19 in the INS group (P = 0.045). The mean of the score changes was 1.72 ± 0.83 in the RF group and 1.17 ± 0.77 in the INS group at the first month follow-up after the intervention (P = 0.009). At the third month of follow-up, the mean VAS scores decreased 2.62 ± 0.66 and 2.33 ± 0.75 in the RF and INS groups, respectively (P = 0.127). The mean reduction amount of the baseline VAS scores at the sixth month of follow-up was 5.28 ± 0.798 and 3.6 ± 1.21 in the RF and INS groups, respectively (Table 2, Figure 1) (P = 0.000).
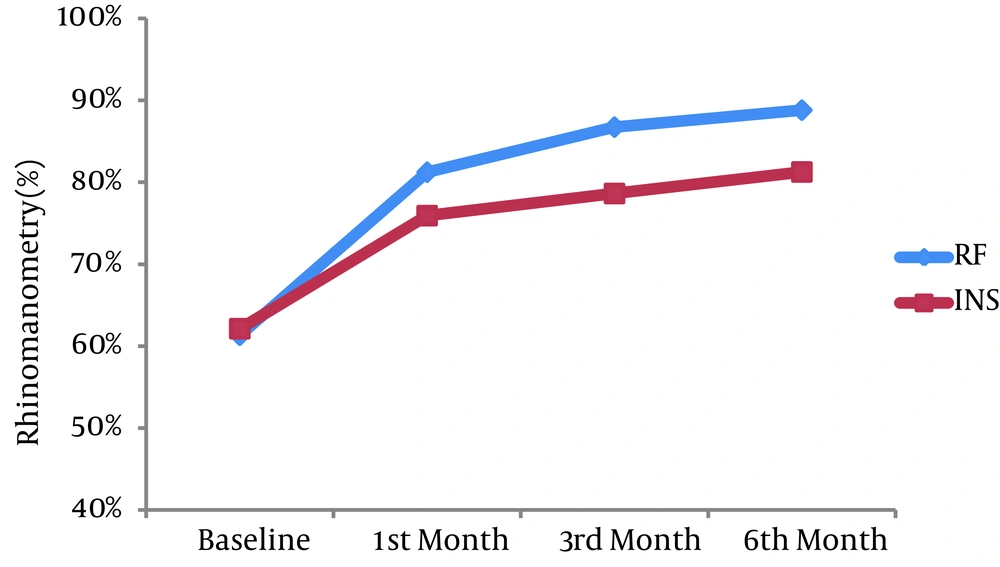
There was no significant difference in the baseline rhinomanometry score (P = 0.752). At all after intervention visits, the mean rhinomanometry score was significantly more in the RF group than the INS group (P < 0.05). At the first month after intervention, the mean rhinomanometry predicted percentage increased 19.9% ± 10.11% in the RF and 13.8% ± 5.09% in the INS group (P = 0.005). This increase from the baseline amount was 25.4% ± 9.56% in the RF and 16.5% ± 5.12% in the INS group, at the third month after the intervention (P = 0.000). After six months, this percentage increased 27.64% ± 7.49% in the RF and 19.13% ± 5.39% in the INS group (Table 3, Figure 2) (P = 0.000).
| Radiofrequency Group (n = 30) | Intranasal Steroid Group (n = 30) | P Value | |
|---|---|---|---|
| Age, Mean ± SD, y | 35.5 ± 8.56 | 37.53 ± 9.18 | 0.379 |
| Male, No. (%) | 12 (40) | 14 (46.7) | 0.397 |
| BMI, Mean ± SD, kg/m2 | 22.53 ± 3.11 | 23.42 ± 3.12 | 0.276 |
Comparison of Patients' Characteristics in Radiofrequency and Intranasal Steroid Groups a
| Visual Analogue Scale (0-10) | Baseline | 1st Month | 3rd Month | 6th Month |
|---|---|---|---|---|
| Radiofrequency group | 6.83 ± 0.57 | 5.11 ± 0.636 | 4.22 ± 0.696 | 1.54 ± 0.885 |
| Intranasal steroid group | 6.35 ± 1.19 | 5.17 ± 0.934 | 4.01 ± 0.784 | 2.75 ± 0.644 |
| P value | 0.045 | 0.754 | 0.293 | 0.000 |
Comparison of the Mean Nasal Obstruction Scores in the Two Groups (Mean ± SD)
| Rhinomanometry (Prediction Percentage) | Baseline | 1st Month | 3rd Month | 6th Month |
|---|---|---|---|---|
| Radiofrequency group | 61.33 ± 10.84 | 81.23 ± 8.06 | 86.73 ± 4.96 | 88.8 ± 5.73 |
| Intranasal steroid group | 62.13 ± 8.56 | 75.93 ± 7.09 | 78.63 ± 7.69 | 81.27 ± 6.97 |
| P value | 0.752 | 0.009 | 0.000 | 0.000 |
Comparison of the Mean Percentage Predicted of Rhinomanometry in the Two Groups (Mean ± SD)
5. Discussion
According to the symptoms severity score and results of rhinomanometry, radiofrequency of inferior turbinate was more effective than intranasal steroids in reducing nasal obstruction severity in patients with ITH due to allergic rhinitis. The current study was in concordance with Gunhan et al. restudy regarding the results of rhinomanometry and reduction of symptoms, with the exception that the latter study covered a 12-month follow-up with no frequent visits after the intervention (1).
The reduction of the severity of symptoms in the third month in this study was confirmed by Sozen et al. with the exception that they analyzed the cases in the third month after the intervention and did not consider quality of life and rhinomanometry of patients (18). The present study was in agreement with Celiker et al. study in reducing the severity of nasal hyperemia (19). The current study agreed with that of Kaymakci et al. in the extent of radiofrequency effectiveness for symptoms of patients with allergic rhinitis, but Kaymakci et al. considered lateral displacement radiofrequency superior to radiofrequency with a four-week follow-up and no assessment of patients' rhinomanometry (11).
This study was confirmed by Kojima et al. in reduction of nasal hyperemia in patients with ITH due to allergic rhinitis, but Kojima et al. conducted a retrospective study which did not compare radiofrequency with other treatments throughout a two-year follow-up. Indeed, Kojima et al. reported a degree of increase in symptoms; but overall, they reported over 75% effectiveness in the second year for this approach (13).
The present study was in strong agreement with Parida et al. study in reducing the indices of nasal hyperemia symptoms and the downward trend of symptoms severity up to the sixth month (14). Kumar et al. did not compare this method with others and did not consider the rhinomanometry of patients (20).
The current study was parallel with that of Lin et al. regarding the reduction of symptoms in radiofrequency in the sixth month with the difference that in the latter study the patients were examined only once in the whole six months of follow-up with no rhinomanometry being performed and no consideration of cases with allergic rhinitis resistant to medical intervention. Of course, Lin et al. assessed the patients in the fifth year and reported a slight rise in symptoms (6).
Radiofrequency approach has also been compared with turbinoplasty via microdebrider (introduced as nasal hyperemia reducer as well as quality of life and rhinomanometry improver in Huang et al. study) (21). Kumar et al. investigated the results of two approaches of turbinoplasty with microdebrider and radiofrequency throughout a six-month period. This study, just as the present one, found radiofrequency to be effective in reducing symptoms in the first and sixth months, while observing the same results for microdebrider; but, three cases of recurrence were reported in the sixth month in the radiofrequency approach, which was the reason for preferring microdebrider to radiofrequency (20). In the study by Cingi et al. which investigated 268 cases with ITH and nasal hyperemia, turbinoplasty with microdebrider was more effective than radiofrequency in reducing the symptoms during three months (22).
The current study was in agreement with Banhiran et al. study in the degree of effectiveness of radiofrequency in reducing the symptoms, with the difference that Banhiran et al. followed patients for eight weeks; their experimental group included cases with chronic rhinitis resistant to treatment, regardless of rhinomanometry (23). A retrospective study by Safiruddin et al. also investigated patients treated with radiofrequency four years after the treatment, and just like the present study, a reduction of symptoms in comparison with the before operation state was reported; however, approximately 30% had recurrences in the fourth year (24). In the survey by Incandela et al. long-term effects of turbinoplasty by radiofrequency was investigated and although in the second year of follow-up only slight increase in symptoms was reported, there were significant reductions compared with the first year (25). Deenadayal et al. investigated 200 cases with allergic and nonallergic rhinitis during a two-year period and found a significantly downward trend in symptoms in comparison to the past, with no recurrent episodes in two years (26). In Garzaro et al. study, not only there was no evidence of recurrence after two years following radiofrequency, they also reported better nasal airflow, symptoms, and olfactory in the second year, compared with the second month (27). The study by Assanasen et al. just as the present study, found radiofrequency to boost nasal airflow in rhinomanometry and reduce symptoms in the tenth week after the intervention. This study also suggested that the patients' olfactory sensitivity significantly improved in the tenth week (28). The results of the current study, in addition to asserting the previous findings, revealed that radiofrequency was more effective than nasal corticosteroid spray in controlling the symptoms of patients with ITH due to allergic rhinitis. It is suggested that in cases with seasonal or mild permanent allergic episodes, radiofrequency should be applied instead of the corticosteroid spray. In addition, results of the present study showed that if the patient is unable to perform radiofrequency for any reason, corticosteroid spray can yield acceptable outcomes in treating the disease and reducing the symptoms severity. Yet, determining the long-term effects and the degree of recurrence of these two approaches demand studies with much longer follow-ups. It is suggested that future studies investigate these two treatments prospectively with randomization and longer follow-ups (2-4 years with frequent visits) to determine the degree of recurrence and levels of symptoms in long term. It is also suggested to compare the long-term effects of radiofrequency with other surgical procedures on ITH in future studies.
Future studies can be designed double-blinded so that each group would be prescribed with a spray (corticosteroid or placebo) and a procedure (radiofrequency or pseudo-radiofrequency) to eliminate the destructive effects of existing mentalities on the researcher and patient’s part. This was almost completely ignored in the previous studies.