1. Background
Evidence-based medicine (EBM) behooves a definitive approach to medical decision-making by investigating to incorporate the best available evidence with clinical expertise (1). An EBM confirmation clinical practice is supported by objective scientific evidence of effectiveness over and above personal experience or narrative (2, 3).
Nowadays, executive boards stress the use of EBM to prevent insecure practices that lack experimental support to decrease unacceptable individual disagreement, and finally to increase efficiency and health care quality (4). In reality, however, it is witnessed that not all health care professionals use EBM in their daily practice. In general medicine, about half of all medical treatments are evidence-based and only about one-fourth of all surgical treatments were found to be based on evidence (5, 6). This is related to a lack of surgical evidence, the fact that surgical questions cannot always be answered by randomized clinical trials or other studies, and limited inclusion criteria that barricade the application of trial recommendations to the average surgical patient (7, 8). Physicians also report a lack of knowledge and basic individual skills on critical evaluation and searching through the literature, as well as a lack of personal time (9); all being major barriers to practicing EBM (10). Several studies have been conducted on EBM in Iran (11-13) yet none have referred to barriers of EBM.
2. Objectives
In order to address this issue, we conducted a study on physicians to determine their attitudes toward the barriers to EBM.
3. Patients and Methods
3.1. Study Design and Sample
This study was an analytical cross-sectional study. After the approval of the Ethics Committee of Ilam University of Medical Sciences in December 2010, questionnaires were sent to 120 physicians of Ilam city, located west of Iran. They represented 60% of the 200 physicians in Ilam, based on statistics obtained from a national database. Furthermore, stratified random sampling was used for selecting the candidates. We define the strata as general practitioners, specialists and sub specialists. The questionnaire consisted of two main sections. The first section asked respondents to describe their personal and professional characteristics such as, age, total years of graduation, medical specialty and sub specialty, extra training in EBM, and number of hours per day spent in different clinical areas. In the second section, attitudes towards the barriers to EBM were determined using visual analogue scales such as: patient-related barriers, physician-related barriers, evidence-related barriers and health system managers-related barriers.
We allocated four options for each question on physician attitudes toward barriers to EBM. As indicated by Table 2, three scores were given to the agree option, two scores to the no opinion and one score to the disagree option. Cronbach's-alpha coefficient was used in order to assess the reliability of the questionnaire. Content validity index (CVI) and content validity ratio (CVR) were used to evaluate the quantitative content validity of the questionnaire. In order to evaluate CVR and CVI, a translated version of the questionnaire was given to five experts, and they were requested to express their opinion on clarity and simplicity of the items.
3.2. Statistical Analysis
To express the results we used Mean ± SD and percentages. Pearson correlation coefficients were used to compute the association of containable variables. Normality of data was checked using a one sample Kolmogorov-Smirnov test. A two-way ANOVA test with post hoc analysis was used to compare the difference between the attitude of general practitioners and the attitude of specialists related to evidence-related barriers. Analyses were done using the R 3.1.1 software. P < 0.05 were considered significant.
4. Results
Of the 120 distributed questionnaires, 94 questionnaires were completed and returned (78.3%). Table 1 compares the demographic features of the responders. Only 12% of physicians had participated in workshops about EBM. About 56.6% of the participants used the Internet to answer questions about their patients, while, 61.4% had used medicine to find clinical evidence. Only 38.5% of the respondents had access to the Internet at their office, while 3.6% and 57.9% of them had access to the Internet at their local library and homes, respectively. Table 1 shows physician’s attitudes towards main barriers to EBM.
There was a significant relationship between patient-related barriers and managers-related barriers (r = 0.237, P = 0.023). The correlation coefficient shows that an increase in manager-related barriers scores led to an increase in patient-related barriers scores. There was no relationship between age, number of hours spent in clinical arenas, years of graduation and the attitude toward barriers to EBM (P > 0.5) (Table 3).
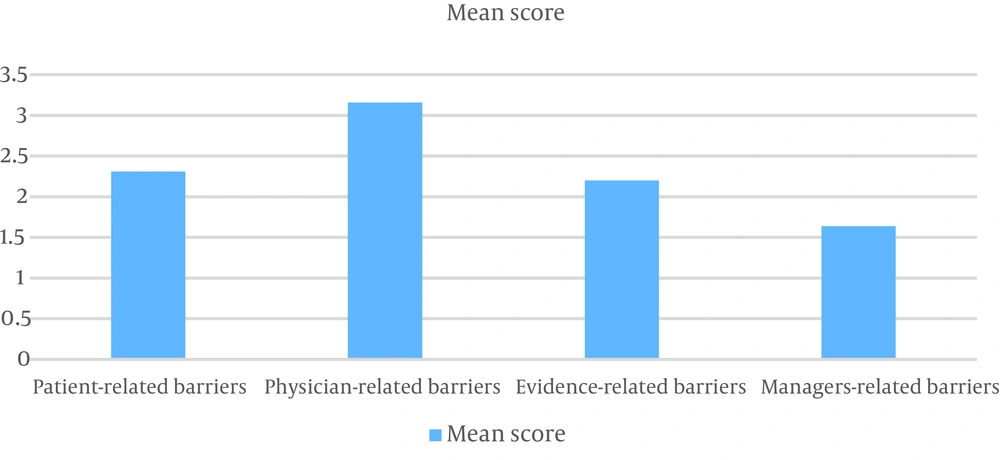
Post hoc tests showed a significant difference between the attitude of general practitioners and the attitude of specialists regarding evidence-related barriers (mean difference = 2.4, Standard deviation = 1.1, P = 0.47). There was a significant difference between the attitude of general practitioners and the attitude of specialists regarding manager-related barriers (mean difference = 0.95, Standard deviation = 0.45, P = 0.038). There was no relationship between the attitude of general practitioners, specialists and subspecialists towards other barriers to EBM under the evidence-related barriers section. The clinical evidence means were more than the other priority means (P > 0.5) (Table 4). The mean score of physician-related barriers were more than the mean scores of other barriers (Figure 1).
| Subject | Agree | No Opinion | Disagree |
|---|---|---|---|
| Patient-related barriers | |||
| To satisfy patients by EBM is difficult. | 57.94 (60.6) | 20.94 (21.3) | 17.94 (18.1) |
| To treat patients who do not cooperate with EBM is difficult. | 53.93 (57) | 33 (35.5) | 7 (7.5) |
| EBM implementation requires a lot of time spent to justify the patient. | 63.94 (67) | 17 (18.1) | 14 (14.9) |
| Inaccurate medical information about the patient prevents a successful implementation of EBM. | 56.94 (59.6) | 26 (27.7) | 12 (12.8) |
| Physician-related barriers | |||
| EBM is a threat for physicians. | 8.94 (8.5) | 12 (12.8) | 74 (78.7) |
| EBM is used more for academic physicians. | 16.94 (77.1) | 11 (11.7) | 67 (71.2) |
| History and physical examination in EBM is less often used. | 10.94 (10.7) | 20 (21.3) | 67 (68.1) |
| EBM will rejected experience of the physician. | 10.94 (10.6) | 26 (27.7) | 58 (61.7) |
| I do not have enough time to use EBM. | 54.94 (57.4) | 21 (22.3) | 19 (20.3) |
| EBM is new and needs to be learnt. | 71.94 (75.5) | 15 (16) | 8 (8.5) |
| Evidence-related barriers | |||
| Using EBM with a lot of medical information is difficult. | 46.94 (48.9) | 25 (26.6) | 23 (24.5) |
| Lack of access to some evidence is a problem of EBM. | 53.94 (56.4) | 22 (23.4) | 19 (20.3) |
| Evidence in many medical fields is not valid. | 55.94 (58.5) | 26 (27.7) | 13 (13.8) |
| Many doctors do not know how to use evidence. | 70.94 (74.4) | 20 (21.3) | 4 (4.3) |
| Health system managers-related barriers | |||
| EBMis not important for managers | 77.94 (81.9) | 14 (14.9) | 3 (3.2) |
| Managers do not invest on implementation of EBM. | 82.94 (87.3) | 12 (12.7) | 0.94 |
| Managers do not provide grants for physicians who use EBM. | 82.93 (88.2) | 11 (11.8) | 0.94 |
a Values are No. (%) of subjects who chose each response.
| Patient-related barriers | Physician-related barriers | Evidence-related barriers | Managers-related barriers | Age | Number of hours spent in clinical arenas | Years of graduation | |
|---|---|---|---|---|---|---|---|
| Patient-related barriers | |||||||
| R | 1 | -0.12 | 0.09 | 0.23 | 0.09 | 0.02 | -0.07 |
| P | 0.22 | 0.35 | 0.02 | 0.37 | 0.79 | 0.46 | |
| Physician-related barriers | |||||||
| R | 1 | 0.08 | -0.00 | -0.00 | -0.19 | 0.02 | |
| P | 0.39 | 0.95 | 0.36 | 0.05 | 0.04 | ||
| Evidence-related barriers | |||||||
| R | 1 | 0.07 | 0.01 | -0.10 | 0.04 | ||
| P | 0.48 | 0.88 | 0.30 | 0.67 | |||
| Managers-related barriers | |||||||
| R | 1 | 0.12 | 0.10 | 0.05 | |||
| P | 0.26 | 0.92 | 0.62 | ||||
| Age | |||||||
| R | 1 | 0.65 | -0.40 | ||||
| P | 0.00 | 0.00 | |||||
| Number of hours per spent in clinical arenas | |||||||
| R | 1 | -0.30 | |||||
| P | 0.00 | ||||||
| Years of graduation | |||||||
| R | 1 | ||||||
| P |
aValues are Presented as Mean ± SD.
5. Discussion
This study was the first study to consider the graduate physicians’ attitudes towards barriers to EBM in Iran and Middle East, and determine the barriers to EBM considered by general practice, specialist and sub specialist physician. A response rate of 78.3% is a considerable achievement as a response rate to questionnaire surveys among physicians; this amount is higher than the difference between the respondents’ attitude in previous studies, and their perception of their colleagues’ attitude could be explained by the more positive attitude of the respondents towards EBM than non-respondents (14). In total, 87.2% of physicians had access to the Internet. This amount is more than the previous study (15).
There was a significant relationship between patient and managers barriers (P = 0.023), possibly because physicians think that more barriers in implementation of EBM exists in patients’ and managers’ barrier views. There was no correlation between age, number of hours spent in clinical arenas, years since graduation and the attitude towards barriers to EBM (P > 0.05); this finding is in agreement with previous studies (8).
There was a significant difference between the attitude of general practitioners and the attitude of specialists related to manager-related barriers (mean different = 0.95, Standard deviation= 0.45, P = 0.038) because most sub specialists and specialists are managers. Patient non-compliance militates against the best evidence being used in practice (16), and the respondents are aware of such non-compliance as this thread was the second priority in this study. Patients unwilling to agree to a treatment or those who ask for a non-evidenced treatment present a real problem for physicians. However, there is certain evidence that better informed patients accept evidence-based change (17). The perceived relevance of research in primary care, difficulty in searching for information, and limited incentives to use EBM are significant barriers for physicians.
The results indicate that physicians also lacked managerial support to implement EBM. Future studies should investigate this perception further at the local level, and national strategies need to be put in place to address this problem, while managers should be required to plan in this field.
The main barriers determined by our study are manager-related. Among the 302 general practitioners, the major perceived barrier to practicing EBM was a lack of time (10). In a descriptive study involving 34 general practitioners (GPs) from England, some expressed their concern about applying guidelines based on trial data to their own patients (17). In an Australian study based on 60 GPs, an important barrier to practicing EBM was identified by most participants, which was the patients’ demand for treatment despite lack of evidence for effectiveness (2). In McKenna et al.’s study, GPs believed that the most significant barriers to using evidence in practice were the limited relevance of research to practice, keeping up with all the current changes in primary care and the ability to search for evidence-based information (15). In a study from Amsterdam, a lack of time to read research reports and to implement new ideas and unclear implications for practice were the major barriers perceived by surgeons and nurses (8). The low number of physicians is a limitation of this study.