1. Introduction
Primary malignant esophageal melanoma makes up 0.1% to 0.2% of all esophageal malignancies (1-6). The expected location of melanoma is melanocyte enriched areas, thus the gastrointestinal tract does not seem to be an appropriate site for primary melanoma. In fact, although the first report of primary esophageal melanoma was in 1906, the term “primary” was not completely accepted until 1963, when the presence of normal melanocytes was demonstrated in the esophagus (1). The presence of melanocytes may be justified due to aberrant migration of melanoblasts through the neural crest during embryogenesis (7).
This malignancy is more common in the 6th and 7th decades of life and is mostly found in men (1, 4). The prominent symptoms of the aforesaid malignancy are dysphagia (the most common), weight loss, pain or discomfort in the chest or epigastric zone, hematemesis and melena (1, 4). The tumor is usually found as a pigmented polyposis lesion in the lower two-thirds of the esophagus (1, 4, 6). The black appearance of this malignancy plus special pathological findings, which are obtained via endoscopy modality, are the diagnostic approach for primary esophageal malignant melanoma. Primary esophageal malignant melanoma has an aggressive behavior with poor treatment prognosis (1-4). This tumor has a rapid dissemination to multiple organs by the means of the lymphatic system and blood vessels. In fact, the five-year survival of malignant esophageal melanoma is about 4% (8). Surgery is the method of choice for this tumor (1, 2, 8). Other adjuvant therapies like chemotherapy, radiotherapy or immunotherapy have also been used, but their efficacy remains unclear (3).
Unfortunately, most physicians assume malignant melanoma as a skin originated neoplasm, yet it can occur wherever in the gastrointestinal tract especially in the esophagus. Thus it is essential to consider malignant melanoma in differential diagnosis of any esophagus mass. Regarding the rare prevalence of this tumor, no population study has been performed and based on review of the literature only case reports have been published. In this study we introduce a case of primary malignant esophageal melanoma and the method of investigation based on the patient’s complains. Then, we evaluate the best method of treatment and assess prognosis and survival in our special case.
2. Case Presentation
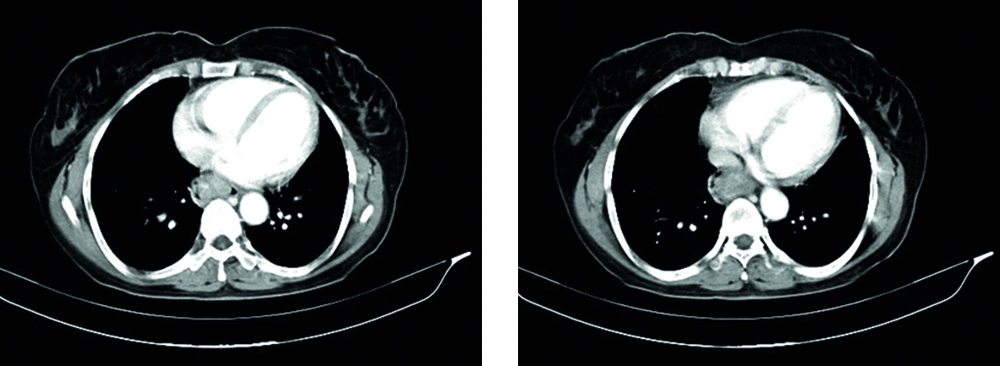
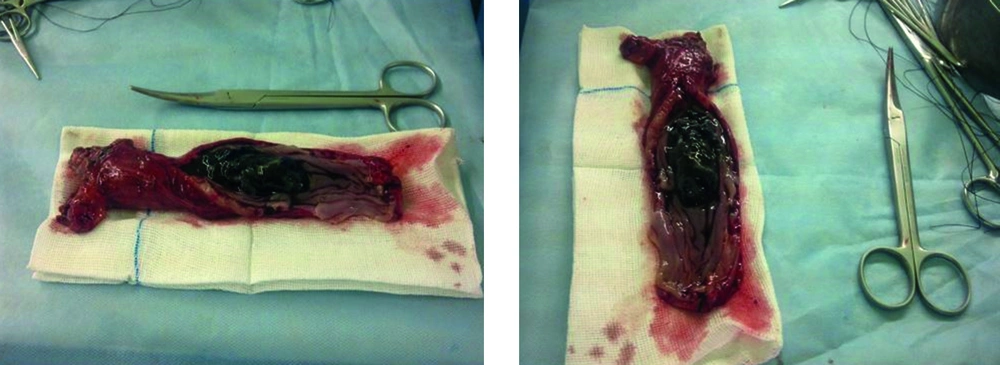
A 47-year-old woman was admitted to the surgery ward with the complaint of progressive solid dysphagia for two months. She had a history of 10% weight loss and decreasing appetite during the last two months. Endoscopic findings revealed a black polypoid tumor, 32 cm from her incisive teeth. Tumor size was about 3 cm with a black appearance, which partially obstructed the lumen. Pathological results showed melanoma cells with irregular hyper chromatic nuclei and melanin pigments, which was in favor of malignant melanoma. In the next step, multiple examinations were performed for finding other sources or metastasis. Total colonoscopy revealed normal findings while brain, thoracic (Figure 1) and abdomino-pelvic CT scan was also done. The only noticeable finding from the CT scan was esophageal wall thickening with no signs of metastasis or other malignancy sources. Based on the aforesaid findings, the patient underwent surgery with the diagnosis of primary esophageal melanoma. Total esophagectomy was done through the right thoracic approach (McKeown approach) and the lesion (Figure 2) with five mediastinal lymph nodes was excited for further surgical staging.
Macroscopic pathology findings included a 5 × 3.5 cm tumor which was located in the one-third distal part of the esophagus. Moreover, pathology examinations revealed melanoma tumor cells with melanin granules in squamous epithelium of esophagus with submucosal invasion. Both the proximal and distal margins were free of tumoral invasion. Also, all of the five mediastinal lymph nodes were free of malignant cells. The patient was discharged one week after the surgery with a good general condition. Our two-week, one, two, four and six month follow up revealed a normal general status.
3. Discussion
Primary esophageal malignant melanoma has an incidence rate of 0.0036 cases per one million individuals per year (9). This tumor includes approximately 0.5% of non-cutaneous melanomas (1, 9). In fact, the low prevalence of typical normal melanocytes in the esophageal mucosa of the general population (2.5%-8%) leads to the rare prevalence of malignant melanoma. Due to its rare prevalence, the genetic basis of this cancer is unclear. However, a few genetic alterations in NRAS, BRAF, and KIT were reported for esophageal melanoma (2). Except for esophageal melanosis, none of the predisposing factors of cutaneous melanoma are considered as risk factors for primary esophageal melanoma in different studies (1, 9).
The literature has revealed that dysphagia, especially to solids, is the most important complaint of the aforesaid patients, which is compatible with our study. One of the previous surveys reported non-solitary lesions in 12% of cases. Also, this study noted that the endoscopic appearance of some lesions was ulcerated. Another study mentioned non-pigmented but melanin contained samples in histological examination of a large group of their patients (1, 9). Both of the aforesaid studies are not compatible with our histopathology results. Thus, it is important to rule out all of the polypoid lesions based on malignancy presence, either it is pigmented or non-pigmented.
Immuno-histochemical examination with positive results of S100 protein, HMB45 and neuron-specific enolase allow a definitive diagnosis for primary malignant melanoma of the esophagus (3). Some studies noted that there is no exact criterion for clinic or histopathology properties, to differentiate primary melanoma from the metastatic form in the esophagus, which makes the diagnosis of primary melanoma a challenge. However, some clues can help. It seems that metastasis to esophagus is a late event in cutaneous melanoma (7). Thus, no previous history of melanoma or signs of other organ involvement apart from esophageal involvement is in favor of primary cancer. In the histology examination, the presence of junctional or in situ melanoma (cells containing melanin granules) in the intact epithelium was in favor of primary origin (Allen and Spitz criteria) (1, 7). Thus, our patient’s histological report was another clue for the primary source of malignancy.
Primary esophageal melanoma metastasis can spread via the lymphatic system and also blood vessels. Common sites of metastasis include the liver, mediastinum, lung and brain (1). However, metastasis to other organs may also occur. For instance, a case of a choroid metastasis of a primary esophageal melanoma has been reported (10). Thoracic and abdominal CT scan is a proper metastatic workup based on the common metastatic sites (1). In our study, brain CT scan was additionally performed. For the aforesaid patient, imaging did not show any sign of metastasis. Endoscopic ultra sonography (EUS) is also a useful tool for preoperative staging of the esophageal melanoma (1, 9) and can show the depth of local tumoral invasion and regional lymph node involvement. However, in this case, EUS was not performed. Although this malignancy has a poor prognosis, and its survival rate is low, surgery is the method of choice for managing esophageal melanoma in cases with resectable tumors (1, 9, 10).
Esophagectomy is believed to be an effective approach for localized primary malignant melanoma of the esophagus. Five-year survival rate of 37% or higher has been recently achieved (11). The type of surgery (radical or palliative) depends on the patient’s situation, including the grade of invasion and presence of metastasis. In our patient, based on imaging findings and staging, which did not show any metastasis or extensive tumoral expansion, and regarding the patient’s age, a radical surgery was chosen. However, the survival rate after radical esophagectomy differs, from the mean of 10-14 months (2) to 5 years (9), in different studies. Through review of previous literature it was indicated that other treatments, such as chemotherapy, radiotherapy or immunotherapy either have no beneficial effects or their efficacy has not been proven (1, 4, 9).
In order to investigate malignant melanoma as soon as possible, whole body examinations are required, while, the patient’s complains are important as well. After malignancy exploration, selection of the most appropriate treatment is the ultimate goal. Educating health care providers reduces the burden of such malignancy for both the patient and the health care system.