1. Introduction
Patients with heart failure (HF) have difficulty maintaining adequate oxygenation; therefore, they are likely to be restless and anxious and feel overwhelmed by breathlessness. These symptoms tend to intensify at night (1). Emotional stress stimulates the sympathetic nervous system, which causes vasoconstriction, elevated arterial pressure, and increased heart rate. This sympathetic response increases the amount of work that the heart has to do. By decreasing anxiety, the patient’s cardiac work also is decreased (2, 3).
Oxygen and other medication, such as anxiolytic agents, may be administered during an acute event to diminish the work of breathing and increase the patient’s comfort. In this case report, we describe a case of cardiac palpitations that temporally appears to be caused by standard doses of oxazepam, an event that has not been previously described in the medical literature.
2. Case Presentation
A 48-year-old man, weighing 55 kg, presented to cardiac care unit (CCU) with a history of systolic heart failure. He reported class 3 pectoris angina (CCS3) and significant dyspnea on exertion (DOE) and no history of hospitalization for his compliant. In physical examination, in heart sound auscultation, we found mitral click in midsystolic phase. He had a history of using drugs such as captopril (ACE i), carvedilol (β-blocker), hydrochlorothiazide (diuretic), and ASA 80 mg, and had no allergies. There was also no significant family medical history. A clinical diagnostic evaluation (echocardiography) showed that 45% ejection fraction and mild mitral regurgitation and his cardiac biomarker analysis showed that ck-MB is in a normal range (below 25) and troponin I is negative. Complete blood count (CBC) diff values were normal and biochemistry levels showed normal levels, except potassium level (K = 5.1 mEq/L). He had not any evidence of abnormal conductivity pathways; however, he had a degree 1 AV block (PR interval = 24 ms) in his electrocardiography (ECG).
He was commenced on a regimen of lozartan 25 mg; tds, metoprolol 50 mg; bid, ASA 80 mg; qd, hydrochlortiazide 5 mg; qd, nitrocantine 2.6 mg; bid, salbutamol 2 puff; tid and prn, and oxazepam 10 mg; qhs. His last vital signs before drug administration were heart rate, 67 bpm, respiratory rate, 17 RR, blood pressure = 137/72 mmHg, and axillary temperature measurement was 36.6˚C.
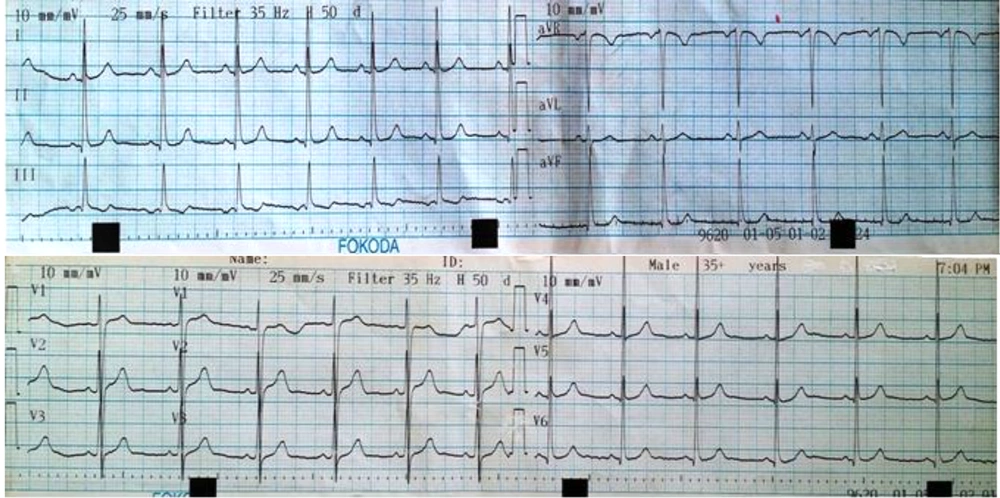
The last ECG before drug administration has shown in (Figure 1).
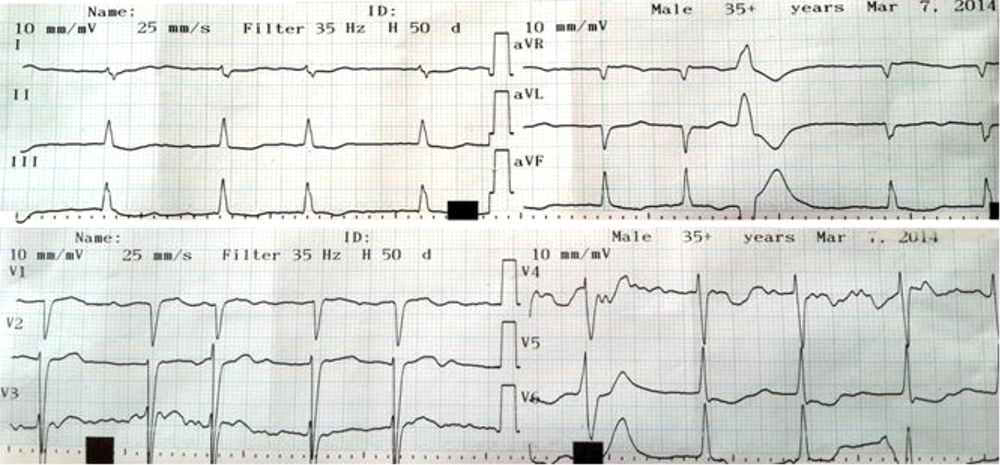
Shortly after taking the second 10 mg dose of oxazepam, he felt sweaty and reported a sensation of palpitations. There were associated lightheadedness, retrosternal and upper abdominal discomfort, but felt no frank chest or abdominal pain. Electrocardiography concurrent with symptoms demonstrated atrial fibrillation (AF) with nonpathologic premature ventricular contractions (PVCs) in ECG trace. His heart rate in this situation is in normal range and with no rapid ventricular response (Figure 2).
The mentioned symptoms lasted only a few minutes. No other symptoms, in particularly those suggestive of either an allergic reaction or an acute coronary syndrome, were noted.
Our patient continued with oxazepam treatment for another day, with exacerbation of his symptoms after taking each oxazepam dose. After informing his cardiologist of her symptoms, his oxazepam medication was discontinued. His symptoms ceased thereafter. After discussion with our patient, a decision was made to not rechallenge his with oxazepam.
3. Discussion
Oxazepam is an anxiolytic- hypnotic drug that widely use in hospitalized patients after cardiac events. (4) Albeit, in previous studies (2, 5), was shown that anxiolytic medication use, is not associated with anxiety level and no effect on length of stay (LOS). Other studies (2) have demonstrated that adverse drug reactions (ADR) to anxiolytic and hypnotic drugs involve the psychomotor function disorder, central nervous system (CNS), accelerated depression, induction of hepatic drug-metabolizing enzymes, acute intermittent porphyria (AIP), and cardiovascular collapse. There is no powerful evidence that show any new cardiac arrhythmia due to anxiolytic use in patient with cardiac events.
Since our patient experienced only symptoms common to those associated with the sensation of palpitations with no symptoms suggestive of an allergic etiology, this case was not one of Kounis syndrome (6).
Atrial fibrillation is an important and potentially serious arrhythmia that is associated with a high prevalence of clinical consequences such as ischemic stroke, hemodynamic impairment and may predispose patients to systemic embolism. The symptoms in the patient were not intensified and following discontinuation of oxazepam administration and absence of its rechallenge, it is probable that standard dose of oxazepam was the causative link with the symptoms of palpitations. This case report appeared to be the first case of cardiac arrhythmia due to standard dose of oral oxazepam administration.
To identify the pathophysiological mechanism of oxazepam-induced cardiac arrhythmia, more research is required in electrophysiological studies.
3.1. Consent
A written informed consent was obtained from our patient for publication of this case report and any pendant image.