1. Background
The high prevalence of chronic kidney disease (CKD) is now considered a major public health problem. According to the Centers of Disease Control and Prevention, more than 20 million (10%) of adults in the United States have CKD, and by 2020 around 750,000 U.S. people will be diagnosed with end stage renal disease (ESRD) (1). The prevalence of CKD among the Iranian population is known to be high. The prevalence and incidence of ESRD are 357 per million population (pmp) and 66 pmp, respectively, and 48.5% are treated with hemodialysis therapy (2). The successful hemodialysis therapy is highly depends on patient adherence to various aspects of the therapy such as regular attendance, restriction of fluid intake, medication and diet adherence (3, 4). Despite the importance of adherence to treatment, no adherence to medical regimes is widely recognized as a serious problem in dialysis. The reported prevalence of no adherence rates in ESRD varies widely, ranging from 22% to 74% (5). Poor adherence is associated with higher mortality, increased health-resource utilization and decreased quality of life of patients undergoing dialysis (6, 7). However, few studies investigated predisposing factors to no adherence in hemodialysis patients (5).
Health literacy has been recognized as an important factor that may influence adherence in chronic diseases (8, 9). The National Institute of Health defines health literacy as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions” (10). Compared to patients with adequate health literacy, those with low health literacy are 1.5- 3 times more likely to experience poor health outcomes (11). They are more likely to have difficulty in understanding healthcare professionals, written health materials/health label, processing health information, and navigating health care environments, as well as, restricted health-related knowledge, limited use of preventive care and less self-care behaviors, such as medication adherence. In addition, inadequate health literacy is linked to higher depressive symptoms, lower quality of life, a higher risk of mortality, frequent hospitalization and higher health care costs (12).
Several conceptual models have been developed to clarify the mechanisms through which health literacy is associated with health actions (13-15). Despite a theoretical association, the relationship between health literacy and adherence has been varied (16). While many studies have investigated health literacy and its association with adherence in patients with chronic conditions, there has been limited researches studying the role of health literacy in patients with kidney disease (17); to our knowledge, no study has examined specifically the relationship between health literacy and adherence behaviors in patients under hemodialysis.
2. Objectives
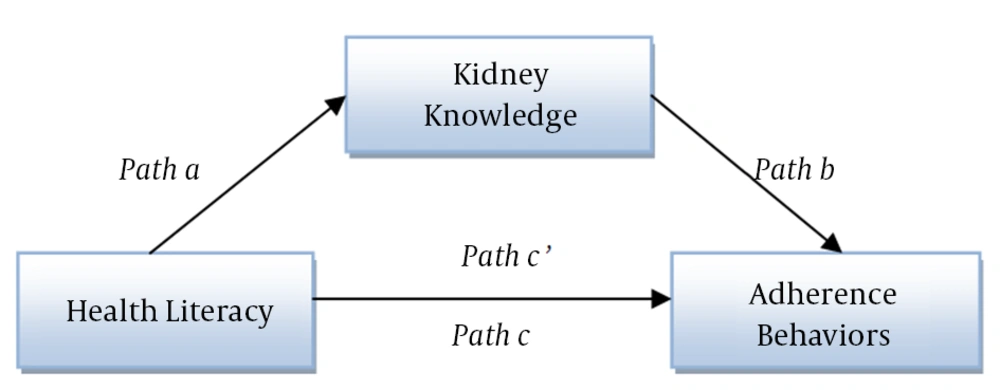
Based on past research and in light of these considerations, the primary objectives of this study were to investigate health literacy in kidney disease and the mediating role of kidney knowledge on the relationship between health literacy and adherence. We hypothesized that health literacy influences adherence through its effect on kidney knowledge.
3. Patients and Methods
3.1. Participants and Procedures
We recruited consecutive patients diagnosed with ESRD who had scheduled appointments at dialysis ward affiliated to Tehran University of Medical Sciences from March 2014 to June 2014. The patients aged 20 to 64 years with ESRD in their medical records, and no other health problems, and with a clinic appointment for receiving hemodialysis were included in the study. Patients were excluded from the study if they did not understand Persian or if the research assistant determined, by interaction or mini-mental state examination (MMSE) score < 24, that they were too ill or cognitively impaired to participate. A total of 240 patients under dialysis were selected from dialysis clinics at four sites. Then, the written informed consent was obtained after the research had been explained to them, and participants were assured that they were free to participate or decline to participate or withdraw from the research at any time. All who provided the written consent were given the questionnaires.
3.2. Questionnaires
3.2.1. Mini-mental State Examination
The 11-item MMSE, the most commonly used instrument for screening cognitive function, examines the cognitive function on a 0- to 30-point scale: orientation to time (5 points), place (5 points), registration (3 points), attention and calculation (5 points), recall (3 points), language (8 points), and visual construction (1 point) (18). Scores 24 and less indicate the cognitive impairment; therefore, individuals with a score less than 24 were excluded from the this study (19). The questionnaire showed the strong validity and reliability in Iranian samples. Cronbach’s alpha has been reported 0.81 for the questionnaire in an Iranian sample indicating it has good internal consistency (20).
3.2.2. Health Literacy
Health literacy was measured using the short test of functional health literacy (S-TOFHLA), a fully validated measure of health literacy that includes an assessment of reading comprehension, as well as numeracy. Scores range from 0-100 and are divided into three levels of health literacy: score ≥ 67 corresponds to adequate health literacy, score of 54-66 delineates marginal health literacy, and score ≤ 53 represents inadequate health literacy. Cronbach’s alpha has been reported 0.68 for the 4 numeracy items and 0.97 for the 36 items in the 2 prose passages (21). Cronbach’s alpha for the Iranian version of the questionnaire was 0.78 for reading comprehension and 0.69 for numeracy scale (22).
3.2.3. Kidney Disease Knowledge Survey
Kidney disease knowledge was assessed using the Kidney disease knowledge survey (KiKS) presented by Wright et al. (2011). The KiKS has 28 multiple choices or yes/no items with good psychometric properties, including strong reliability and validity (23). The survey was forward and back-translated using a multistep method to ensure the quality of translation (24), and then pilot-tested with 30 patients to test reliability in Iranian sample.
3.2.4. The End Stage Renal Disease-Adherence Questionnaire
The end stage renal disease-adherence questionnaire (ESRD-AQ) is a 46-item instrument, consisting of four subscales: dialysis sessions, medications, and fluid and diet adherence. All four subscales had strong validity and reliability (25). The subscales were forward and back-translated using a multistep method to ensure the quality of the translation, and then pilot-tested with 30 patients to test reliability in Iranian sample.
3.3. Statistical Analyses
Data were analyzed using the SPSS version 21 (IBM New York, USA), and chi-square analyses were conducted to determine if there were any significant differences among the health literacy levels on education, employment, age group, sex, insurance, and marital status. The results of these analyses are presented in Table 1. A one-way analysis of variance (ANOVA) was conducted to determine if differences existed between these three levels on kidney knowledge and adherence (Table 2). Also, the Games-Howell test was done to compare these multiple groups. To test mediating effects of knowledge, mediation analysis was conducted using bivariate regression, hierarchical regression and Sobel test as proposed by MacKinnon, Fairchild, and Fritz, respectively. In a mediation model, a predictor should significantly influence both the mediator (Figure 1, Path a) and criterion variable (Figure 1, Path c), and the mediator should be significantly related to the criterion variable (Figure 1, Path b) (26).
| Total sample (%) | Inadequate | Marginal | Adequate | P Value | |
|---|---|---|---|---|---|
| Gender | 0.78 | ||||
| Male | 58.8 | 26.7 | 10 | 63.3 | |
| Female | 22.1 | 22.6 | 9.5 | 67.9 | |
| Age, y | 0.81 | ||||
| 20-29 | 7.8 | 18.8 | 12.5 | 68.8 | |
| 30-39 | 6.9 | 28.6 | 0 | 71.4 | |
| 40-49 | 17.2 | 20.0 | 5.7 | 74.3 | |
| 50-59 | 42.6 | 27.6 | 10.3 | 62.1 | |
| 60-64 | 25.5 | 25.0 | 35.0 | 24.1 | |
| Education | 0.003 | ||||
| Elementary | 44.6 | 30.8 | 11.0 | 58.2 | |
| Middle School | 14.7 | 33.3 | 20.0 | 46.7 | |
| High School | 26.9 | 9.1 | 3.6 | 87.3 | |
| Higher education | 13.7 | 28.6 | 7.1 | 64.3 | |
| Employment | 0.43 | ||||
| Employed | 22 | 22.9 | 6.7 | 70.4 | |
| Housewives | 25.9 | 21.7 | 39.2 | 39.1 | |
| Un-employed | 13.2 | 45.0 | 11.7 | 43.3 | |
| Retired | 35.3 | 20.2 | 15.8 | 64 | |
| Others | 3.4 | 0 | 78.3 | ||
| Marital Status | 0.52 | ||||
| Married | 71.2 | 22.6 | 8.2 | 69.2 | |
| Single | 16.6 | 17.6 | 14.7 | 67.6 | |
| Other | 12.2 | 27.4 | 12.5 | 62.5 | |
| Insurance | 0.45 | ||||
| Insured | 97.1 | 24.2 | 10.1 | 65.7 | |
| Un-insured | 2.9 | 50.0 | 0 | 50 |
aData are presented as No (%).
| Variables | Total | Levels of Health Literacy | P Value | ||
|---|---|---|---|---|---|
| Inadequate | Marginal | Adequate | |||
| Knowledge | 18.0 ± 4.3 | 15.0 ± 5.05 | 18.3 ± 2.5 | 19.1 ± 3.5 | < 0.001 |
| Adherence | 7 ± 2.1 | 6.3 ± 2.1 | 7.7 ± 1.2 | 8.1 ± 1.9 | < 0.001 |
a Data are presented as mean ± SD.
4. Results
Of 240 eligible patients, 9 refused participation, 27 failed to complete all questionnaires; therefore; a total of 204 men and women undergoing dialysis completed all measures. All measures had good reliability and validity. In the current study, Cronbach’s alpha of KiKS and ESRD-AQ were calculated 0.83 and 0.74, respectively, indicating strong internal consistency. Participants were, on average, 50.9 ± 10.9 years old. As shown in Table 1, the majority of the sample was male, married, retired, had elementary school education, and had health insurance. Approximately one fourth of the sample had limited health literacy according to the S-TOFHLA. Health literacy was significantly associated with education; participants with higher education had higher level of health literacy (X2 = 19.7, P = 0.003) (Table 1). No significant relationship was observed between health literacy levels on gender, age, employment, insurance and marital status. Adherence scores differed significantly by health literacy level (P < 0.02) (Table 2). Post-hoc pairwise comparisons indicated individuals with inadequate health literacy had significantly lower adherence scores (mean = 383.3) than those with adequate health literacy (mean = 434.9, P < 0.02). There was no significant difference between marginal and adequate health literacy (P = 0.49) or marginal and inadequate health literacy (P = 0.89). For kidney knowledge, one-way ANOVA revealed that kidney knowledge scores varied significantly by level of health literacy (P < 0.001). Post-hoc pairwise comparisons showed that individuals with inadequate health literacy had significantly lower kidney knowledge scores than those with either marginal (mean = 18.3, P = 0.002) or adequate health literacy, P < 0.001). There was no significant difference between marginal and adequate health literacy (P = 0.43).
Bivariate analysis showed that health literacy was significantly related to the kidney knowledge (P < 0.001) and adherence (P < 0.006) (Table 3). Also, there is a significant relationship between kidney knowledge and adherence (P < 0.005). Health literacy was positively related to kidney knowledge (β = 0.08, SE = 0.01) and adherence (β = 1.04, SE = 0.37). Kidney knowledge was positively associated with adherence behaviors (β = 5.3, SE = 1.9). The hierarchical regression revealed that a reduced effect of the health literacy on adherence behaviors occurred when knowledge entered as a mediator into the equation (the β value for health literacy was reduced from 1.04 to 0.71). The Sobel test indicated that kidney knowledge was a mediator of the influence of health literacy on adherence in kidney disease (z = 2.6, P = 0.008). Taken together, kidney knowledge mediates the relationship between health literacy and adherence behaviors in dialysis patients.
| Variables | Β | SE | P Value | r |
|---|---|---|---|---|
| Health Literacy-> Kidney Knowledge | 0.08 | 0.01 | 0.00 | 0.42 |
| Kidney Knowledge- > Adherence | 5.8 | 1.9 | 0.005 | 0.20 |
| Health Literacy- > Adherence | 1.04 | 0.37 | 0.006 | 0.19 |
a Abbreviation: SE, Standard Error; B, Beta; r, correlation coefficient.
5. Discussion
The current study examined health literacy and its associated factors among patients undergoing dialysis. Our findings showed that approximately one fourth (25%) of the participants had adequate health literacy (65.2%), implying that the majority of the patients had considerable difficulty in understanding and reading information. However, some studies found that the prevalence of low health literacy is much higher in Iranian sample (27, 28). The difference may result from the more frequent hospitalizations of dialysis patients, their weekly exposure to the medical setting, educational programs or health materials and their more frequent communications with medical staff rather than normal population or other patients.
Our findings indicate that low health literacy is a predictor of kidney knowledge. Consistent with other studies, lower kidney knowledge has been reported in dialysis patients with inadequate health literacy compared to those with marginal and adequate health literacy (29, 30). Lower disease-specific knowledge in patients with inadequate health literacy may be attributable to their limited abilities to read or understand medical information about the disease and its management. Due to these limited abilities, patients with low health literacy are less likely to experience printed health materials or communicate with medical staff; therefore, they will get less disease-related information and have less chance to expand their knowledge regarding their disease. Moreover, health literacy was significantly associated with adherence behaviors. Consistent with the previous evidence (31-33), patients with limited health literacy showed significantly lower adherence scores than most literate participants did. Patients with low health literacy may not be able to read drug labels, medication instructions, and health booklets or understand their health professionals thus causing them to take their medications inappropriately, stop prescribed diet, and choose irrelevant treatment options.
Our findings highlighted the importance of health literacy promotion, demonstrating a significant association of kidney disease knowledge with both health literacy and adherence, and indicating that kidney knowledge was a significant mediator of the relationship between health literacy and adherence. This finding provides empirical evidence to support significance of health literacy in promoting disease-specific knowledge and improving adherence. Based on these results, further investigations should be undertaken to design appropriate educational interventions during the initial stages of CKD to prevent ESRD and further increase in burden of kidney failure and disease management.
Our study has several limitations. First, the small sample size limited the ability to generalize the findings. We were also not able to compare our model by socio-demographic variables, which may be confounders or moderators. Second is related to measurements used in the current study; the S-TOFHLA cannot assess all aspects of health literacy.
The results could be important in establishing the role of health literacy in the daily care of patients with kidney disease. In addition, understanding the relationship between health literacy and self-care behaviors should enhance efforts to improve dialysis outcomes.