1. Background
Also known as hyaline membrane disease (HMD), respiratory distress syndrome (RDS) is one of the most common respiratory disorders among premature infants. It usually occurs in infants with gestational ages of less than 37 weeks; however, it may be present in infants with higher gestational ages due to premature lungs (1). RDS is majorly resulted from alteration in Surfactant production, so most patients will be dependent on mechanical ventilation and Surfactant injections which decreases the time needed for intubation (2, 3).
Despite recent developments in application of corticosteroids for preventing RDS and its acceptable results, there are also concerns about superiority of benefits on possible complications that has made corticosteroid use a controversy (4, 5). Dexamethasone is a widely used systemic corticosteroid in RDS, which is being evaluated in many controlled clinical trials, and evidences have shown that using dexamethasone after birth has positive effects on improving respiratory functions of neonates, especially those under mechanical ventilation (6). Nonetheless, optimal time of dexamethasone administration has not been clarified yet (7). In previous studies, it has been concluded that treatment with dexamethasone should not be considered as a routine option for preventing or managing chronic respiratory diseases because it may lately result in neuromotor or cognitive disorders (8, 9).
N-Acetyl cysteine (NAC) is an antioxidant and antimucus agent which increases glutathione in cellular level and leads to destructing mucoprotein chains in lung mucus and loosing thick layers of mucus. Mucolytic agents help with cleaning respiratory discharges and improve respiration. This cleaning decreases the chance of growth for secondary bacteria. Effects of NAC have been studied in a variety of diseases such as cystic fibrosis, chronic bronchitis, noncystic fibrosis, pulmonary fibrosis, and many other medical conditions. Previous studies have concluded that NAC inhalation decreases hospitalization duration in infants with acute bronchiolitis, but it has not been yet assessed in RDS (10). Thus, in the present study we aimed at assessing the effect of inhaler NAC on respiratory distress syndrome by comparing it with intravenous dexamethasone.
2. Methods
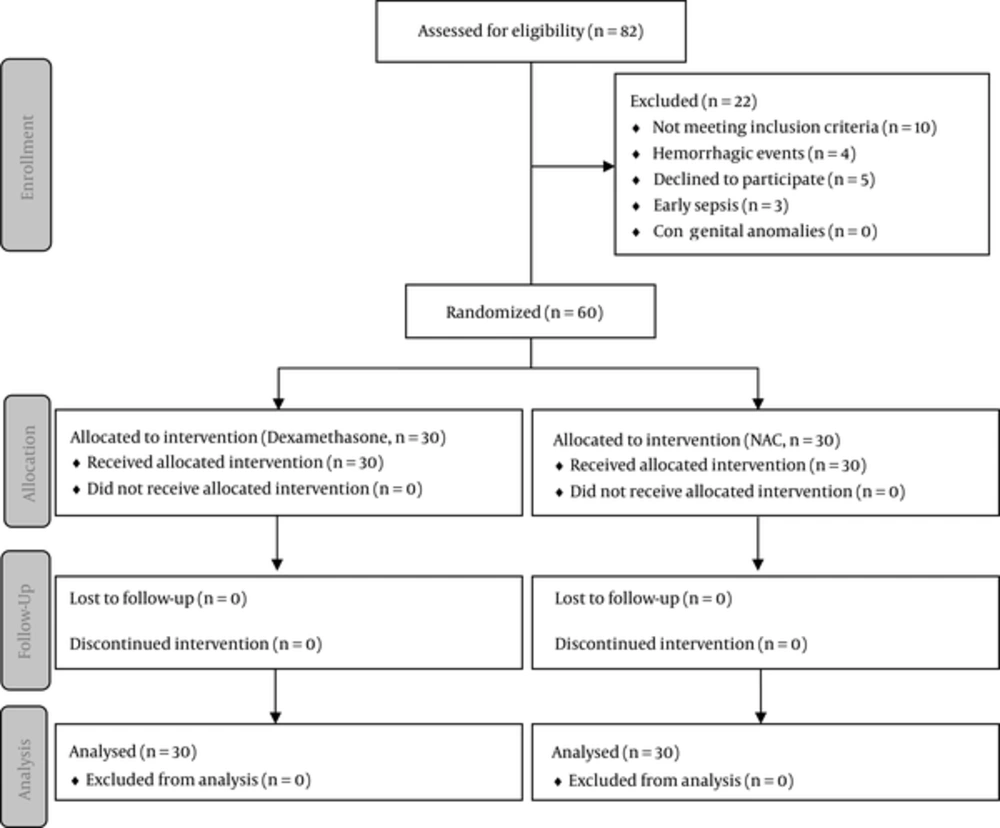
This randomized clinical trial was conducted between September 2014 and August 2015 in Najmiyeh hospital, Tehran, Iran. The present study was registered at ethics committee of Islamic Azad University (Reference code: IR.IAU.PS.REC.1392.24) and Iranian registry of clinical trials (Reference code: IRCT2016101917413N2). Figure 1 displays a flowchart of the trial. Infants with confirmed diagnosis of RDS based on chest radiography, respiratory rate, arterial blood gas (ABG), first and fifth minutes Apgar scores, grunting, cyanosis, and physical examination by a single neonatologist were assessed for eligibility in the first 4 hours of life. Patients with congenital or chromosomal anomalies, death before 72 hours of life, early sepsis, hemorrhagic events or those whose parents did not wish to participate in the study were excluded. Infants with the following criteria were included in the study: Infants with gestational age of less than 36 weeks, those in need of mechanical ventilation for at least 2 days, with birth weight between 1000 and 2500 gr, and those who required oxygen saturation of more than 30% after extubation. All the baseline characteristics as well as demographic information were recorded in a predesigned checklist. Study process was explained to all parents and a written consent was obtained.
After respiratory protection for 3 to 5 days and after extubation, infants were randomly allocated into 2 groups using random number table. The first group underwent treatment with intravenous dexamethasone (0.15 mg/kg every 12 hours) and the second group received NAC nebulizer (400 mg every 8 hours) as well as intravenous dexamethasone for 3 to 5 days. Treatment duration, disease and drug complications, and number of received doses as well as response to treatment (based on oxygen dependency and need for reintubation), and mortality rates were recorded in a checklist.
Data were analyzed using statistical package for social sciences (SPSS) for Windows (Version 21, IBM Corp, Armonk, NY). Normal distributed variables (approved by 1-sample Kolmogorov-Smirnov test) were compared using independent sample t test between the groups. Chi square test was used to compare categorical variables in the 2 groups. Mean and standard deviation (SD) were used to describe categorical variables.
3. Results
Finally, we evaluated 60 (33 males and 27 females) infants in 2 dexamethasone and N-Acetyl cysteine groups. Demographic information is demonstrated in Table 1. Cesarean section was the most prevalent delivery method in mothers of both dexamethasone (93.4%) and N-Acetyl cysteine (96.67%) groups. In Dexamethasone group 7 (23.34%) and in NAC group, 3 (10%) infants had a gestational age of less than 28 weeks. Infants in dexamethasone group had a mean birth weight of 1574.50 ± 561.75 gr, and this was 2477 ± 1479.42 gr in NAC group (P = 0.003). In NAC 10 (33.3%) and in dexamethasone groups, 5 (16.6%) infants had a birth weight less than 1000 gr. Among infants in NAC group, 15 (50%) and of those in dexamethasone group, 7 (23.3%) infants underwent mechanical ventilation for more than 3 days. Twenty-four (80%) mothers in dexamethasone group and 17 (56.6%) in NAC group had received antenatal corticosteroids. Premature rupture of membrane (PROM) more than 18 hours before birth was recorded for 1 (3.33%) infant in NAC group and 1 (3.33%) in dexamethasone group had premature meconium defecation. Placental decollement was seen in 3 (10%) infants in dexamethasone and 1 (3.33%) infant in NAC group. Disease complications are listed in Table 2. Infants in dexamethasone group showed less complication compared with the other group. Pneumonia (16.6%) and pneumothorax (16.6%) were the most prevalent complications among dexamethasone group. In NAC group, pneumonia (56.6%) was the most commonly seen complication, and 6 (20%) infants developed patent ductus arteriosus (PDA).
| Variables | NAC (N = 30) | Dexamethasone (N = 30) | P Value |
|---|---|---|---|
| Male | 15 (50) | 18 (60) | 0.758 |
| Gestational age, weeks | 0.279 | ||
| < 28 | 3 (10) | 7 (23.34) | |
| 28 - 33 | 13 (43.33) | 12 (40) | |
| 34 - 36 | 14 (46.66) | 11 (36.66) | |
| Birthweight, gr | - | ||
| < 1000 | 5 (16.66) | 10 (33.3) | |
| 1000 - 2000 | 14 (46.66) | 19 (63.33) | |
| > 2000 | 11 (36.66) | 5 (16.66) | |
| Mean Apgar score | |||
| 1st minute | 7.26 ± 0.98 | 6.9 ± 1.60 | 0.185 |
| 5th minute | 8.1 ± 1.62 | 7.86 ± 1.43 | 0.166 |
| PROM>18 hours | 1 (3.33) | 0 | 0.326 |
| Meconium defecation | 0 | 1 (3.33) | 0.326 |
| Placental decollement | 1 (3.33) | 3 (10) | 0.310 |
| Diabetes | 2 (6.66) | 1 (3.3) | 0.562 |
aValues are expressed as No. (%).
| Complication | NAC (N = 30) | Dexamethasone (N = 30) |
|---|---|---|
| Necrotizing Enterocolitis (NEC) | 2 (6.66) | 0 (0) |
| Sepsis | 2 (6.66) | 0 (0) |
| Intracranial Hemorrhage | 1 (3.33) | 2 (6.66) |
| Patent Ductus Arteriosus (PDA) | 6 (20) | 1 (3.33) |
| Pneumonia | 17 (56.66) | 5 (16.66) |
| Pneumothorax | 1 (3.33) | 5 (16.66) |
aValues are expressed as No. (%).
In dexamethasone group, mean arterial oxygen pressure (PaO2) was 62.36 ± 18.76 mmHg before, and it was 82.3 ± 19.58 mmHg after intervention. Mean arterial oxygen pressure (PaO2) was 62.53 ± 20.31 mmHg before, and it was 91.3 ± 26.90 mmHg after intervention in NAC group. Mean duration of hospitalization was 13.2 ± 9.3 days in dexamethasone and 17.60 ± 17.65 days in NAC group (P = 0.757). Mortality rate was 10% in dexamethasone and 3.3% in NAC group. Treatment complications have been listed in Table 3. The most prevalent complication among both groups was milk intolerance.
| Complication | NAC (N = 30) | Dexamethasone (N = 30) |
|---|---|---|
| Hyperglycemia | 0 (0) | 1 (3.33) |
| Hypertension | 0 (0) | 0 (0) |
| Raised intracranial pressure | 0 (0) | 0 (0) |
| Milk intolerance | 2 (6.66) | 2 (6.66) |
| Nausea | 0 (0) | 0 (0) |
| Abdominal distension | 1 (3.33) | 1 (3.33) |
| Coagulopathies | 0 (0) | 0 (0) |
aValues are expressed as No. (%).
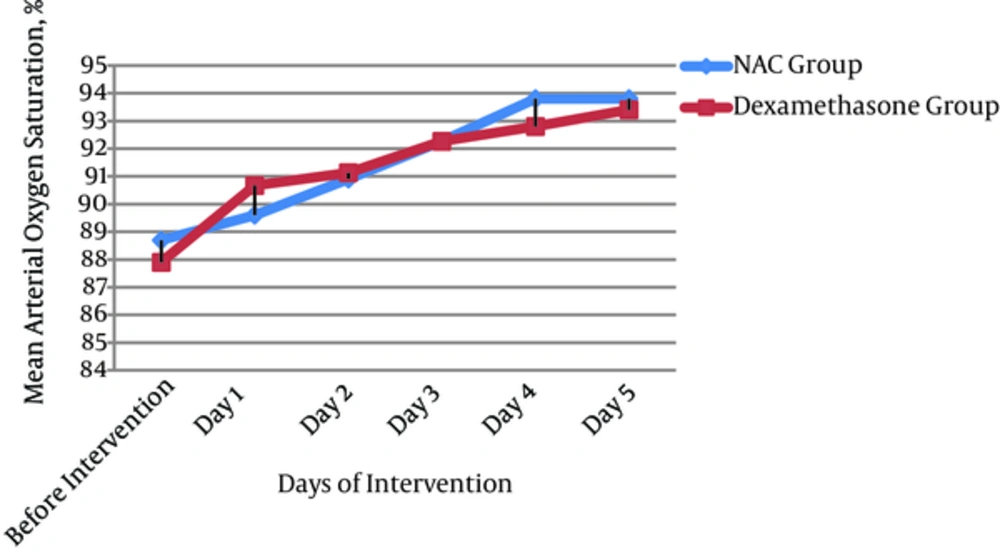
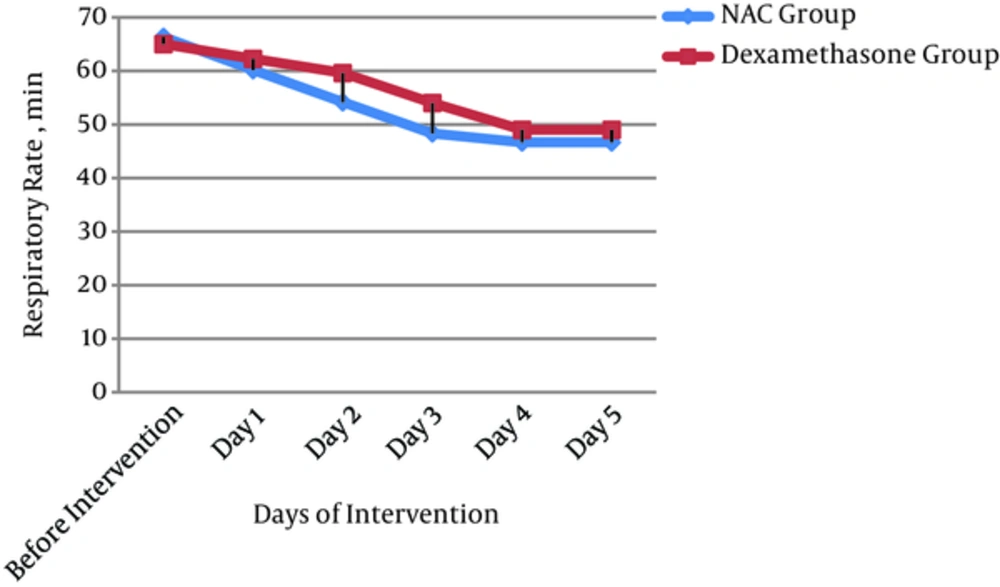
Mean arterial oxygen saturation (O2 sat) trend during treatment is displayed in Figure 2. Mean arterial oxygen saturation was 88.70 ± 4.31% in NAC and 87.90% ± 5.96% in dexamethasone groups before the intervention (P = 0.553). In the fifth day of the intervention, mean arterial oxygen saturation was 93.80 ± 3.86 in NAC and 93.4% ± 3.79% in dexamethasone groups (P = 0.321). Prior to intervention, infants in NAC group had a mean respiratory rate (RR) of 66.33 ± 8.33, and this was 65 ± 12.66 in dexamethasone group (P = 0.656). In the fifth day of intervention, infants had a mean RR of 46.67 ± 9.21 in NAC and 49 ± 12.66 in dexamethasone group (P = 0.454). Before intervention all infants in NAC group and 58 (96.6%) in dexamethasone group were oxygen dependent (P = 0.197). In the fifth day of intervention, 5 (8.3%) infants in NAC and 3 (5%) in dexamethasone group required oxygen therapy (P = 0.409). Before the intervention, 22 (23.33%) infants in NAC and 14 (36.67%) infants in dexamethasone group needed to be reintubated (p = 0.064). In the fifth day of intervention, 2 (1.67%) infants in NAC and 1 (3.33%) infant in dexamethasone group needed to be reintubated (P = 0.562).
4. Discussion
In the present study, we found no significant difference between dexamethasone alone and dexamethasone with N-Acetyl cysteine nebulizer for the treatment of respiratory distress syndrome in infants; however, both groups showed a significant response to treatment. This positive effect was seen for respiratory rate, mean arterial oxygen saturation, oxygen dependency after extubation, and a need for reintubation. Treatment goal for respiratory rate has been mentioned as less than 60 per minute in previous studies which was achieved in our both study groups as well. In both dexamethasone and NAC groups, mean oxygen saturation (based on pulse-oxymetry) was maintained between 90% to 92% in preterm infants weighting lower than 1250 gr and upmost 95% in preterm infants with gestational ages more than 32 weeks, which was the treatment goal. The aim of treating RDS is to decrease the required oxygen density after extubation which was reported in both dexamethasone and NAC groups in the present study. All the infants in both groups had intercostal retractions and about half of them in NAC group showed a significant decrease in retraction as the drug was administered; however, retraction was resolved in only 1 infant in dexamethasone group after the first day of intervention.
In our study, 60% of infants had gestational ages of less than 34 weeks, which confirms the previous fact that incidence of RDS is inversely related to gestational age (10, 11). Nearly all infants in both groups were conceived by cesarean section which has been mentioned as a risk for incidence of RDS (12). In the present study, more than 95% of infants in dexamethasone and about 64% of infants in NAC group were less than 2000 gr, which confirms the higher rate of RDS in low birth weight infants (1).
Milk intolerance was the most prevalent adverse effect of treatment in both dexamethasone and NAC group. There was no significant difference between the 2 groups for incidence of adverse effects. In a review article by Halliday et al., assessing the effectiveness of early treatment (less than 1 week) of RDS with dexamethasone, they have mentioned that despite beneficial results in extubation and decreased risk of respiratory disorders during 28 days, incidence of short-time complications such as hemorrhage, gastrointestinal tract perforation, hypertrophic cardiomyopathy, and hypertension was increased (13). In another clinical trial by Oktaviani, effects of administration of NAC or betamethasone were evaluated in women threatened with premature delivery, and was concluded that betamethasone was more effective than NAC for ling maturation of infants (14).
In previous studies, it has been concluded that prescription of NAC nebulizer decreases the hospitalization duration and accelerates the trend of improvement in infants with acute bronchiolitis (10). In another similar study, it was mentioned that intratracheal administration of NAC will increase airway resistance in premature infants; however, routine prescription of this drug was not recommended due to possible lung injuries in some infants, which was not in agreement with the present study (15). This may be due to lower duration of treatment with NAC in the present study. Prescription of inhaler NAC in children with cystic fibrosis and adults with chronic respiratory disease was associated with decreased pulmonary function (16).
Considering the fact that the prescribed doses of dexamethasone and NAC in the present study were in the lowest range of commonly used doses and taking into account the short treatment duration of infants (3 - 5 days) after extubation, incidence rate of adverse effects were unremarkable and it seems that RDS was appropriately managed in patients.
In the present study, no superiority was observed for intravenous dexamethasone or NAC nebulizer with intravenous dexamethasone in treatment of infantile RDS; however, adding NAC was more effective in treatment parameters such as respiratory rate, oxygen dependency, and mean arterial oxygen saturation due to more accurate delivery of the drug to respiratory system. Also, it was more effective in qualitative parameters of treatment such as intercostal retraction and a need for reintubation. Mortality rate and oxygen dependency were significantly decreased in both groups.
In conclusion, we found no significant difference between intravenous dexamethasone alone and intravenous dexamethasone with N-Acetyl cysteine nebulizer in treating infantile respiratory distress syndrome. However, a significant response to treatment was observed in both groups. According to the acceptable signs of response to treatment and considering that no remarkable adverse effects were reported, short-time administration of these drugs is recommended.
We suggest further studies with larger sample volume and more follow- up durations for better addressing the efficacy and possible long-term adverse effects of these medications. Moreover, it is recommended to prescribe NAC in a wider range of infantile respiratory diseases to evaluate its possible positive effects.