1. Background
A low level of high-density lipoprotein cholesterol (HDL-C) is one of the common types of dyslipidemia in patients with early coronary artery diseases (CADs) and has a strong, inverse, and independent association with the incidence of these disorders (1, 2). Therefore, any reduction in HDL increases the risk of CADs by 2% - 3% (3). The frequency of low HDL levels, either alone or combined with other lipid disorders, varies across countries (6% to 34%) (4). According to the report of the National Center for Health Statistics, the prevalence of low HDL levels in adults was 21.3% in 2009 - 2010 (5) and 19% in 2011 - 2014 (1). Low HDL is more common in Asian populations. A systematic review of 37 studies in Asia revealed that 33.1% of the population had low HDL levels (4). According to several studies on the prevalence of dyslipidemia in Iran, 43.9% of the studied population had low HDL levels (6). In another study in Iran, 13% of women and 30% of men in Tehran had HDL levels lower than 35 mg/dL (7). In addition, in northwestern Iran, 73% of the people aged 20 years and above had HDL abnormalities (8). In a study on adolescents in Birjand, 24.7% had HDL levels lower than 40 mg/dL (9).
The molecular mechanisms of the biological effects of HDL on CADs remain unknown. Various roles of HDL, as a protective factor against CADs, include enhancing macrophage cholesterol efflux and reversing cholesterol transport, as well as its anti-inflammatory, anti-thrombolytic, anti-apoptotic, and antioxidant properties (10).
Coronary artery diseases are associated not only with dyslipidemia and metabolic syndrome, including hypertension and diabetes mellitus, but also with unhealthy behaviors such as smoking, physical inactivity, and an unhealthy diet (11). These vascular risk factors are generally controlled using a combination of drugs and lifestyle modifying measures, including quitting smoking, choosing healthy foods, increasing physical activity, and using adequate medications for a lifetime (12, 13).
2. Objectives
Considering the importance of lifestyle in patients with lipid disorders, this study aimed to evaluate the lifestyle of people with low, normal, and high HDL levels in order to divulge modifiable risk factors in this regard. In this study, we also investigated the relationship between cardiovascular risk factors and HDL cholesterol level in the patients referring to the Heart Clinic of Birjand, Iran, during 2016 - 2017.
3. Methods
3.1. Study Design and Population
In this cross-sectional study, 401 patients referring to the heart clinic, Cardiovascular Diseases Research Center, of Birjand, during 2016 - 2017 were selected through the convenience sampling method. Considering a 43% prevalence of low HDL and using a sample size calculation formula designed for the comparison of ratios, a 95% confidence interval, and 0.05 margin of error, the sample size was determined as 376. However, regarding probable attrition, a total of 410 people were finally recruited. Inclusion criteria were age over 20 years, satisfaction for participation, and regularly visiting the center for blood lipid profile screening. The exclusion criterion involved inability to continue participation due to travel or non-cooperation. Eventually, 401 people remained in the study. Written informed consent was obtained from all the studied individuals.
3.2. Measures
After recalling the patients, a questionnaire prepared on the basis of the IRAPEN Standard Nutrition and Physical Activity questionnaire (a translation of the WHO standard questionnaire by the Ministry of Health and Medical Education), was completed by them. Furthermore, the subjects’ demographic data, including a history of smoking and illnesses, were collected, and clinical data were extracted from their medical records and entered into the questionnaire.
The IRAPEN questionnaire consisted of seven items about moderate and vigorous physical activity, including walking and seated activities such as watching the television. The scoring method was based on the relative frequency of the existence or absence of any kind of moderate or vigorous walking activity and, if any, the duration of each activity per day. The second part of the questionnaire was about the frequency of consuming 25 important food items, including daily, weekly, or monthly consumption, as well as rarely and never, and the relative frequency of rarely and never consumed food items and the frequency of their consumption per day, week, or month. There were also three questions about salt intake and two questions about the type of the oil consumed (cooking, frying) and eating breakfast. In our study, we complied with American Heart Association guidelines proposing seven indicators, including four behavioral indicators (diet, physical activity, smoking, and BMI) and three risk factors (cholesterol, blood pressure, and blood glucose), as the criteria for assessing cardiovascular health. The physical activity, diet, and smoking status were determined based on the mentioned questionnaire (11).
Based on the data obtained from the questionnaire, physical activity was converted into MET (or the basal resting metabolism) by multiplying the number of days of physical activity by the minutes of activity per day multiplied by four. Subsequently, the MET values of walking and moderate and vigorous activity were summed up. Finally, the MET values of less than 600, between 600 and 1500, and higher than 1500 were regarded as low, moderate, and high physical activity, respectively (14). With respect to the diet, the consumption of fruits and vegetables at least five times daily was considered as ideal, 1 - 4 times as intermediate, and less than one occasion as poor diet. The height and weight of the participants were measured, and according to which, body mass index (BMI) was determined. The subjects’ blood pressure, fasting blood sugar (FBS), and cholesterol levels were determined. Smoking status was also asked from the participants and recorded in the questionnaire. Altogether, these seven criteria were used to classify patients into poor, intermediate, and ideal categories.
Based on HDL levels, the subjects were categorized into three groups: Low (less than 40 mg/dL in men and less than 50 mg/dL in women), normal (between 40-60 mg/dL in men and 50-60 mg/dL in women), and high (more than 60 mg/dL) HDL levels.
3.3. Statistical Analysis
After collection, the data was analyzed by SPSS-15. The risk factors of CADs were studied in three groups and analyzed using the chi-square or Fisher’s exact test. Logistic regression was used to determine the factors affecting HDL levels and predicting a low HDL level. The significance level was considered P < 0.05.
3.4. Ethical Approval
This study was approved by the Ethics Committee of Birjand University of Medical Sciences, with the following ethics code: IR.BUMS.REC.1395.208.
4. Results
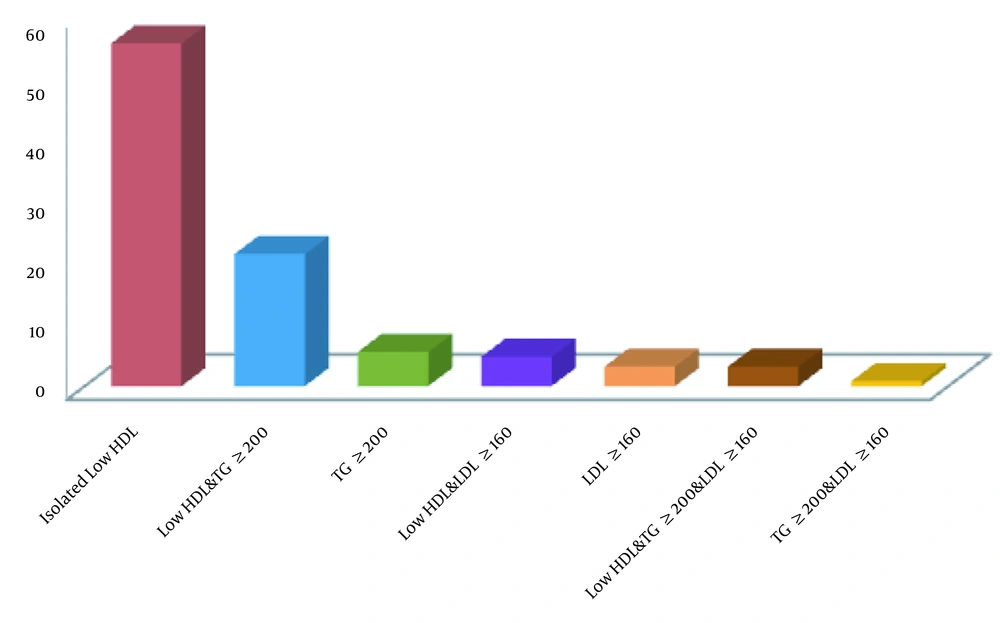
A total of 401 subjects with an average age of 52.94 ± 13.03 (23 - 89 years) participated in the present study. Most of the participants were in the age group of 40 to 60 years. Also, 221 (55%) participants were female; 227 (56.6%) were married, and 92% settled in urban areas. Various types of lipid disorders were assessed in the dyslipidemia group. Overall, 59.4% of the participants had a normal lipid profile, while most people with dyslipidemia (58.8%) had isolated low HDL (Figure 1).
Based on HDL levels, the subjects were categorized into three groups: Low, normal, and high HDL levels, most of whom (n = 214, 53.3%) being in the low-HDL group, while the minority (n = 73, 18.2%) were in the high-HDL group.
Table 1 compares the demographic data of these three groups (i.e., low, normal, and high HDL), showing a significant difference between them in terms of the marital status, but not age, place of residence, and education level (Table 1).
| Characteristics | Low HDL (N = 214), No. (%) | Normal HDL (N = 114), No. (%) | High HDL (N = 73), No. (%) | P-Value |
|---|---|---|---|---|
| Age | 0.06 | |||
| ≤ 40 | 45 (52.9) | 19 (22.4) | 21 (24.7) | |
| 40-50 | 61 (58.7) | 23 (22.1) | 20 (19.2) | |
| 50-60 | 57 (53.3) | 20 (28.2) | 17 (16.5) | |
| ≥ 60 | 51 (46.8) | 43 (39.4) | 15 (13.8) | |
| Sex | < 0.001 | |||
| Male | 106 (60.9) | 59 (33.9) | 9 (5.2) | |
| Female | 108 (47.6) | 55 (24.2) | 64 (28.2) | |
| Marriage status | 0.02 | |||
| Single | 7 (50) | 1 (7.1) | 6 (42.9) | |
| Married | 207 (53.5) | 113 (29.2) | 67 (17.3) | |
| Residency | 0.74 | |||
| Urban | 194 (53) | 106 (29) | 66 (18) | |
| Rural | 20 (57.1) | 8 (22.9) | 7 (20) | |
| Education | 0.53 | |||
| Under the diploma | 126 (51.2) | 74 (30.1) | 46 (18.7) | |
| Diploma and higher | 88 (56.8) | 40 (25.8) | 27 (17.4) | |
| Comorbidity | ||||
| Coronary arterial disease | 57 (54.3) | 39 (37.1) | 9 (8.6) | 0.004 |
| Diabetes mellitus | 37 (59.7) | 18 (29) | 7 (11.3) | 0.28 |
| Chronic kidney disease | 3 (50) | 1 (16.7) | 2 (33.3) | 0.58 |
| Cerebral infarction | 2 (33.3) | 4 (66.6) | 0 (0) | 0.09 |
The Demographic Characteristics of the Study Participants
As shown in Table 2, regarding each of the seven cardiovascular health criteria, the participants were categorized into three groups (i.e., poor, intermediate, ideal). According to this classification, most of the participants were in the poor group in terms of BMI and physical activity, in the intermediate group in terms of the smoking status and cholesterol and FBS levels, and in the ideal group in terms of diet and blood pressure (Table 2).
| Characteristics | No. (%) |
|---|---|
| Dietary pattern | |
| Poor | 46 (11.5) |
| Intermediate (1-4-a-D) | 297 (74.1) |
| Ideal (≥ 5-a-D) | 58 (14.5) |
| Physical activity | |
| Poor (< 600 MET h/week) | 266 (66.3) |
| Intermediate (600 - 1500 MET h/week) | 55 (13.7) |
| Ideal (≥ 1500 MET h/week) | 80 (20) |
| Smoking status | |
| Poor (current smoker) | 19 (4.7) |
| Intermediate (ex-smoker) | 8 (2) |
| Ideal (never smoker) | 374 (93.3) |
| Body mass index | |
| Poor (≥ 27) | 220 (54.8) |
| Intermediate (24 - 26.9) | 105 (26.2) |
| Ideal (< 24) | 76 (19) |
| Cholesterol | |
| Poor (≥ 240) | 33 (8.2) |
| Intermediate (200 - 239) | 93 (23.2) |
| Ideal (≤ 199) | 275 (68.6) |
| Blood pressure | |
| Poor (SBP ≥ 140 or DBP ≥ 90) | 156 (38.9) |
| Intermediate (SBP120-139 OR DBP80-89) | 176 (43.9) |
| Ideal (SBP < 120 and DBP < 80) | 69 (17.2) |
| FBS | |
| Poor (≥ 126) | 48 (12) |
| Intermediate (100 - 125) | 105 (26.2) |
| Ideal (≤ 100) | 248 (61.8) |
Health Metrics’ Specific Definitions and the Prevalence of Cardiovascular Health Criteria
The highest rate of moderate and vigorous physical activity was observed in the normal-HDL group, while the lowest rate of activity was recorded in the high- and low-HDL groups. There was a significant relationship between physical activity and HDL level. Comparing the three groups, there were significant differences in FBS, BMI, and blood pressure, but not in the dietary status, smoking history, and blood cholesterol level (Table 3).
| Characteristics | Poor, No. (%) | Intermediate, No. (%) | Ideal, No. (%) | P-Value |
|---|---|---|---|---|
| Dietary pattern | 0.42 | |||
| Low HDL | 22 (10.3) | 166 (77.6) | 26 (12.1) | |
| Normal HDL | 13 (11.4) | 80 (70.2) | 21 (18.4) | |
| High HDL | 11 (15.1) | 51 (69.9) | 11 (15.1) | |
| Physical activity | 0.01 | |||
| Low HDL | 151 (70.6) | 26 (12.1) | 37 (17.3) | |
| Normal HDL | 63 (55.3) | 24 (21.1) | 27 (23.7) | |
| High HDL | 52 (71.2) | 5 (6.8) | 16 (21.9) | |
| Smoking status | 0.16 | |||
| Low HDL | 10 (4.7) | 3 (1.4) | 201 (93.9) | |
| Normal HDL | 7 (6.1) | 5 (4.4) | 102 (89.5) | |
| High HDL | 2 (2.7) | 0 (0) | 71 (97.3) | |
| Body mass index | < 0.001 | |||
| Low HDL | 135 (63.1) | 56 (26.2) | 23 (10.7) | |
| Normal HDL | 102 (89.5) | 34 (29.8) | 27 (23.7) | |
| High HDL | 32 (43.8) | 15 (20.5) | 26 (35.6) | |
| Cholesterol | 0.21 | |||
| Low HDL | 13 (6.1) | 48 (22.4) | 153 (71.5) | |
| Normal HDL | 10 (8.8) | 25 (21.9) | 79 (69.3) | |
| High HDL | 10 (13.7) | 20 (27.4) | 43 (58.9) | |
| Blood pressure | < 0.001 | |||
| Low HDL | 100 (46.7) | 89 (41.6) | 25 (11.7) | |
| Normal HDL | 39 (34.2) | 56 (49.1) | 19 (16.7) | |
| High HDL | 17 (23.3) | 31 (42.5) | 25 (34.2) | |
| FBS | 0.01 | |||
| Low HDL | 29 (13.6) | 60 (28) | 125 (58.4) | |
| Normal HDL | 16 (14) | 33 (28.9) | 65 (57) | |
| High HDL | 3 (4.1) | 12 (16.4) | 58 (79.5) |
Comparison of Cardiovascular Health Between Participants with Different HDL Categories
Compared with the low-HDL group, the rate of moderate and vigorous physical activity was 1.94- and 1.27-time higher in the normal-HDL and high-HDL groups, respectively. After adjusting for age and sex, subjects with high and normal HDL levels had 2- and 1.96-time higher rates of moderate and vigorous physical activity, respectively, than subjects with low HDL levels.
Table 4 depicts the number of cardiac risk factors in terms of different HDL levels. In subjects with poor cardiovascular health, there was a significant difference in the distribution of risk factors between the three groups, so that the risk factors were markedly higher in the low-HDL group compared to other groups. The prevalence of subjects with ≥ 3 cardiovascular risk factors was 36% in the low-HDL, 22.9% in the normal-HDL, and 17.9% in the high-HDL groups (Table 4).
| Number of Cardiovascular Risk Factors | Total (N = 401) | Low HDL (N = 214) | Normal HDL (N = 114) | High HDL (N = 73) |
|---|---|---|---|---|
| 0 | 31 (7.7) | 11 (5.1) | 15 (13.2) | 5 (6.8) |
| 1 | 105 (26.2) | 46 (21.5) | 31 (27.2) | 28 (38.4) |
| 2 | 149 (37.2) | 80 (37.4) | 42 (36.8) | 27 (37) |
| 3 | 83 (20.7) | 56 (26.2) | 19 (16.7) | 8 (11) |
| 4 | 29 (7.2) | 19 (8.9) | 6 (5.3) | 4 (5.5) |
| 5 | 4 (1) | 2 (0.9) | 1 (0.9) | 1 (1.4) |
Number of Cardiovascular Risk Factors (Poor Cardiovascular Health) by the HDL Level (P-Value = 0.01)
Table 5 shows the results of logistic regression for the factors predicting a low HDL level. Among the variables included in the model, gender, BMI, and physical activity correlated with low HDL levels.
| Characteristics | B | SE | P-Value | Odd Ratio | 95 CI (Exp B) |
|---|---|---|---|---|---|
| Sex | 0.61 | 0.24 | 0.01 | 1.84 | 1.15 - 2.96 |
| Age | -0.14 | 0.10 | 0.17 | 0.86 | 0.69 - 1.06 |
| SBP | -0.13 | 0.19 | 0.51 | 0.87 | 0.59 - 1.29 |
| DBP | -0. 27 | 0.17 | 0.12 | 0.76 | 0.53 - 1.07 |
| Cholesterol | 0.30 | 0.17 | 0.07 | 1.35 | 0.96 - 1.89 |
| Physical activity | 0.35 | 0.13 | 0.01 | 1.42 | 1.08 - 1.85 |
| Smoking | 0.20 | 0.25 | 0.41 | 1.22 | 0.74 - 2.02 |
| BMI | 0.55 | 0.14 | < 0.001 | 1.73 | 1.30 - 2.31 |
| FBS | -0.18 | 0.16 | 0.24 | 0.82 | 0.60 - 1.13 |
| Diet | -0. 19 | 0.21 | 0.36 | 0.82 | 0.54 - 1.24 |
| Constant | -2.25 | 1.38 | 0.10 | 0.10 |
The Independent Association of Different Variables with Low HDL
5. Discussion
Various genetic and environmental factors can play a role in reducing the HDL level (8, 15). In this cross-sectional study, most of the patients with dyslipidemia had isolated low HDL. Regarding gender distribution, the number of women was significantly higher than men in the high-HDL group, while in the normal- and low-HDL groups, the ratio of men to women was almost equal. Considering that the mean age of women in the high-HDL group was lower than in the other groups, it can be predicted that the majority of women in the high-HDL group were at or before menopause, which could explain the higher ratio of females in the high-HDL group. A low level of HDL has been considered to be a major risk factor of CAD for 50 years. Considering the fact that high HDL is a protective factor against cardiovascular diseases (16), the incidence of CAD is expected to be lower in patients with higher levels of HDL, as seen in the present study.
The highest rate of moderate and vigorous physical activity was observed in the normal-HDL group, while the lowest rate of moderate-vigorous activity was recorded in the high- and low-HDL groups. There was a statistically significant relationship between physical activity and HDL level. As shown in another study, among different types of serum lipids, HDL was the most common lipoprotein that improved by physical activity (17). For example, a study indicated that regular physical activity could increase HDL levels in adults (1).
The prevalence of smoking was higher in people with normal HDL and lower in those with elevated HDL. However, there was no significant difference between the groups regarding the smoking status. It has been shown in other studies that smoking has an unfavorable impact on HDL cholesterol level, reducing its concentration by 5.7% (18, 19), which has been attributed to the effect of smoking on HDL metabolism, and subsequently on the risk of CAD.
In the present study, the prevalence of obesity and overweight was significantly higher in the low-HDL group than in the normal- and high-HDL groups. In a study by Cabrera et al. (20) on the factors associated with dyslipidemia, BMI was linked with dyslipidemia in the studied population. Another study showed that obesity and high BMI could increase blood pressure and LDL level and decrease HDL (15).
Moreover, TG level was significantly higher in the low-HDL group than in the other groups. Finally, after adjusting for other factors in a regression model, high LDL and TG levels were associated with low HDL levels.
5.1. Limitations
Being a single-center (the Heart Clinic of Birjand, Iran) retrospective study is an obvious limitation. Moreover, other factors that could have affected HDL levels, such as hormone therapy, menopause, and the use of contraceptives, were not investigated in this study. A number of the patients were not newly diagnosed cases, and some patients had a history of coronary arterial diseases and diabetes, which might have affected the results.
5.2. Conclusions
Considering the relationship between the persistent risk factors of CAD and HDL cholesterol level, encouraging people to adopt a healthy lifestyle can help prevent cardiac diseases.