1. Background
Multinodular goiter (MNG) comprises a spectrum of clinical features, consist of multiple hyper functioning nodules scattered throughout an enlarged thyroid gland that also may contain non-functioning nodules [1]. Using ultrasonography, in an area with borderline iodine deficiency, MNG is found in approximate 23% of the general population [2]. Medical care or radioactive iodine may use for larger goiters, but the best choice of MNG treatment is surgery, especially in cosmetic problem, compressive symptom, toxicity and suspicion of malignancy [3]. There are several methods for thyroid gland operation such as subtotal thyroidectomy (STT), near-total thyroidectomy (NTT), hemi-thyroidectomy plus subtotal resection (Dunhill procedure) and total thyroidectomy (TT). But the surgical method of benign thyroid disease treatment is still controversial [3, 4].
Before 20th century, the risks associated with major surgery for treating thyroid diseases and the problems of adequate hormonal replacement had deterred surgeons from performing total thyroidectomy, and in fact, this method, was only performed occasionally for thyroid cancers [5, 6]. Nowadays, the use of total thyroidectomy, which is designed to remove whole thyroid tissue, remains controversial for small differentiated thyroid carcinomas, but even more controversial is its use to treat benign diseases [7, 8]. The major complications related to total thyroidectomy are permanent hypoparathyroidism and recurrent laryngeal nerve injuries [9]. Also there are several studies which have showed that the complication rates of permanent recurrent laryngeal nerve palsy (0 - 1.3%) and permanent hypoparathyroidism (0.5 - 1%) following subtotal thyroidectomy are similar to those following total thyroidectomy [10-14]. Other disadvantages of subtotal thyroidectomy for treat multinodular goiters are that the procedure does not reduce the risk of persisting symptoms and has a high recurrence rate (30 - 50%) owing to gland remnants [15, 16]. The aim of a surgeon performing subtotal and near total thyroidectomy (STT and NTT) for MNG is to try to keep the patient euthyroid post-operatively avoiding the need for lifelong thyroid replacement. But despite of the little remnant thyroid tissue in all surgical procedures, except of total thyroidectomy, the necessity of treatment with thyroid hormone still remains [17]. On the other hand, the incidence of thyroid cancer varies from 7.5 - 13% in cases of nontoxic MNG [18] and due to the possibility of malignancy in remnant thyroid tissue or recurrence of MNG, sometimes it is necessary to reoperation for complete thyroidectomy. During this subsequence surgery, the incidence of complications such as serious indemnifies to recurrent laryngeal nerve (RLN) and parathyroid and near organs is higher [18, 19]. Otherwise, in TT method, the risk of repeated surgery and its complication decreases in large scale and it may be the prefer approach [20]. The objective of this study is describing the complication rates of total thyroidectomy in MNG treatment.
2. Patients and Methods
In this cross sectional study, from January 2009 to January 2011, 118 consecutive patients with MNG underwent TT operation in two referral surgery centers in Rasht (North of Iran): Razi and Pursina hospitals.
2.1. The Inclusion Criteria
All patients with MNG indicated for TT due to cosmetic problems, hoarseness or compressive disorders.
2.2. The Exclusion Criteria
Suspicion of malignancy, positive family history of thyroid malignancy, Grave’s disease, thyroiditis, previous thyroid surgery, positive history of head and neck radiation and disturbed calcium metabolism.
So, 17 cases excluded from this survey [1 case with positive fine needle aspiration specimen for malignancy, 3 cases with Grave’s disease, 1 case with positive history of thyroid malignancy in his father and 12 cases with unavailability of fine needle aspiration (FNA) results].
2.3. Pre-Operation Management
Clinical assessments in all patients included measurements of serum thyrotropin, thyroxine, triiodothyronine, thyroid antibodies and calcium, fine needle aspiration (negative, suspicious, indeterminate) and ultrasound estimation of thyroid volume and morphology. Surgery was performed under general anesthesia by an experienced surgeon. Written informed consent was obtained from all patients; patient information included detailed explanation of the treatment.
2.4. Surgical Methods
Surgical dissection of the thyroid took place after the identification and preservation of both laryngeal nerves and superior and inferior parathyroid glands. In all patients, we identified 3 - 4 parathyroid glands and left them in situation with their own vascularization. If we inadvertently removed or devascularized a parathyroid gland, we auto-transplanted the gland into the ipsilateral sternocleidomastoid muscle.
2.5. Post-Operation Management
At the time of extubation, the anesthesiologist evaluated vocal cord motility in all patients. Because unilateral recurrent laryngeal nerve palsy sometimes can be clinically difficult to detect, an otolaryngologist performed a laryngoscopy in all patients before they had discharged. We defined recurrent laryngeal nerve palsy as horseness associated with vocal cord paralysis at laryngoscopy within 6 months post-operatively. After 6 months, we considered recurrent laryngeal nerve palsy permanently. Hormonal treatment with levothyroxin began within 5 days after surgery in all patients. We drained the neck with bilateral suction drains for 48 hours and patients were discharged within 4 days after surgery. Calcium levels were obtained on the first and second post-operative days and on 6 months follow up appointment. Hypocalcaemia was defined as less than 2.00 mmol/L and permanent if requiring ongoing oral calcium supplementation beyond 3 months.
2.6. Follow up Planning
Outcome assessment was performed for two weeks, 1 month, 2 months, 10 months and 20 months after surgery for each patient. All clinical variables were assessed by unbiased observer (a research surgeon who was not involved in the surgery or clinical decisions and who was blinded to the treatment group).
We extracted data on sex, age, WHO classification of goiter [21] (Grade I: palpable but visible with the neck extended, Grade II: visible with the neck in normal position, Grade III: visible from a considerable distance), pre-operative assessment (operative time, intra operative blood loss, hematoma, mortality), seroma (a collection of fluid under the skin at the site of the surgical incision), recurrent laryngeal nerve palsy (temporary, permanent) and hypocalcemia rates (temporary, permanent), rates of other post-operative complications, final pathology and recurrence. We diagnosed recurrence if one of the following criteria showed up: 1) Volume of one lobe more than 9 mL for women and more than 12 mL for men or volume of both lobes more than 18 mL for women and more than 24 mL for men; 2) Presence of a nodule more than 9 mm; 3) Presence of an autonomous adenoma.
2.7. Statistical analysis
All data were statistically analyzed using SPSS-19 software (SPSS Inc., Chicago, IL, USA). Analysis of variance (ANOVA), Fisher exact test and χ2 test were used. P-Value < 0.0001 is considered statistically significant.
3. Results
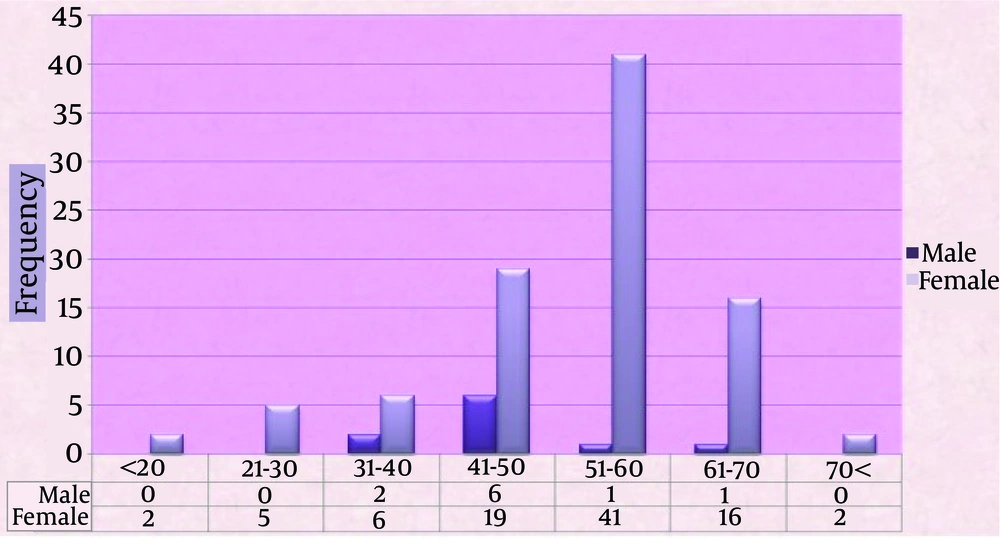
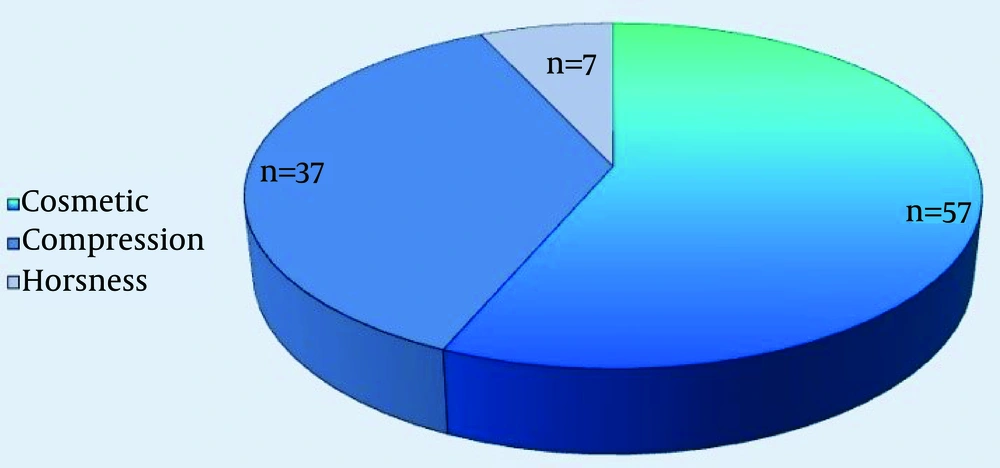
Of 101 included cases, with mean age of 47.1 ± 12.9 years, 10 cases were male and 91 cases were female (Figure 1). Eighty one percent of all cases aged below 60 years. Ultrasonography showed MNG in all patients. The minimum and maximum time between beginning of symptoms and operation time were 2 months and 40 years. More than 50% of cases referred after 6 years of beginning manifestations. Bilateral gland involvement showed in 88.11% (n = 89) of patients. Figure 2 shows the frequency of different symptoms of presentations among all cases.
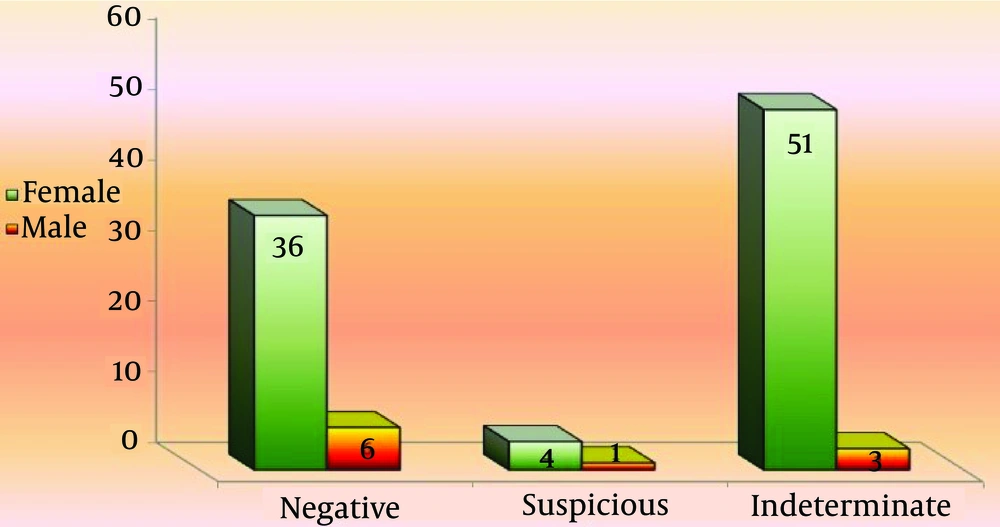
The FNA results in 41.6% (n = 42) of patients was negative for malignancy and was indeterminate and suspicious in 53.5% (n = 54) and 5% (n = 5) of all cases (Figure 3). The demographic features, intra operative characteristics and complications are showed in Table 1. No mortality happened during this survey and post-operative hematoma requiring repeat surgery occurred in no patients.
| Variables | Values |
|---|---|
| 47.1 ± 12.9 | |
| 91 (90.01) | |
| 89 (88.11) | |
| Grade I | 0 |
| Grade II | 23 |
| Grade III | 78 |
| 48 ± 11 | |
| 261 ± 21 | |
| 0 (0) | |
| 2 (1.98) | |
| 0 (0) | |
| 0 (0) |
a Data are presented as mean ± SD.
b Data are presented as No. (%).
Transient RLN palsy was observed in only one case. She was a 42 years old women with cosmetic complain and bilateral MNG. Transient hypocalcaemia showed up in 25 patients (2 cases with clinical presentations of tetanus and 23 cases with calcium level dropping in laboratory findings). There was no direct relationship between age and presenting transient hypocalcaemia or RLN palsy.
No permanent hypocalcaemia and permanent RLN palsy appeared (Table 2).
| Variables | Values |
|---|---|
| 100 (99.01) | |
| 1 (0.99) | |
| 0 (0) | |
| 76 (75.25) | |
| 25 (24.75) | |
| 0 (0) |
a Abbreviation: RLN, recurrent laryngeal nerve.
b Data are presented as No. (%).
Incidental malignancy within the pathology specimen was determined in 15.84% of patients (n = 16): 1 patient with medullary carcinoma, 2 cases with folicullar carcinoma and 13 patients with papillary carcinoma. There was no direct relationship between age and presenting malignancy. All these cases were female and had been presented with compression problems and bilateral involvement of MNG. The pre-operative FNA results of these patients were 2 cases (with follicular carcinoma) as suspicious, 4 cases (1 case with medullary carcinoma and 3 cases with papillary carcinoma) as negative and 10 cases (with papillary carcinoma) as indeterminate. No recurrence of MNG showed up during our follow up.
4. Discussion
Our study results revealed that post-operative transient hypocalcaemia and transient RLN palsy happened in 24.75% and 0.99% of all cases. No permanent complications and recurrence were shown. No patients in this study who required re-operation for hematoma. Also, we found incidental thyroid carcinomas on histology in 16 patients (15.84%): 1 patient with medullary carcinoma, 2 cases with follicular carcinoma and 13 patients with papillary carcinoma. There was no wound infection during follow-up.
Multi nodular goiter is clinically important for several reasons. It may cause thyroid dysfunction or compressive symptoms, but it is even more important because of the need to exclude thyroid cancer [22]. The reported prevalence of malignancy in thyroid nodules, evaluated by biopsy, ranges from 4% - 6.5% and is largely independent of the nodule size [22, 23]. Complications of thyroid surgery consist of temporary or permanent RLN palsy, temporary and permanent hypocalcemia, hematoma and seroma. Due to ligation of the all branches of vessels on superior and inferior pole, there were no patients in this study who required re-operation for hematoma.
The incidence of post-operative transient hypocalcaemia and transient RLN palsy were 24.75% and 0.99%. No permanent complications and recurrence were shown. Some other studies had been accomplished to show the same results. Gal et al. [24] studied 264 cases underwent TT and the results showed 31 cases (11.7%) with transient hypocalcaemia, but only 1 (0.3%) symptomatic and only 4 (1.5%) with permanent hypocalcaemia. Other complications included hematoma in 4 cases (1.5%), temporary RLN palsy in 7 cases (2.6%), permanent RLN palsy in 2 cases (0.75%) and seroma in 8 cases (3%). Incidental thyroid carcinomas were found on histology in 9 patients (3.5%) which was lower than our results (15.84%). No MNG recurrence presented in their study.
In a study of Veyseller et al. [25], the incidence of post-operative permanent hypocalcaemia and permanent RLN palsy were 0.6% and 1.86% whereas we had no cases of these complications. Efremidou et al. [26], showed the incidence of permanent RLN palsy as 0% and that of permanent unilateral RLN palsy as 0.2%. Their results showed permanent hypocalcaemia in 0.3% and temporary hypocalcaemia in 7.3%. Hemorrhage requiring repeat surgery occurred in 0.2% and post-operative mortality was zero. There was no wound infection during follow-up.
FNA biopsy was available but was not distinct tool for diagnosing thyroid malignancy and selecting candidates for surgery with a sensibility and specificity of 16% and 97% [27].
There are some studies which declare that using FNA in MNG had been unnoticed for more than 80% of carcinomas [28]. In our survey, incidental malignancy within the pathology specimen was determined in 16 patients. The pre-operative FNA results of these patients were 2 cases (with follicular carcinoma) as suspecious, 4 cases (1 case with medullary carcinoma and 3 cases with papillary carcinoma) as negative and 10 cases (with papillary carcinoma) as indeterminate. Patients with malignancy needed no re-surgery for completion thyroidectomy in our survey.
Due to the small remnant tissue and the scar of previous surgery, re-operation is difficult and carries a significant risk of damage to both RLNs and the parathyroid glands. It means that during completion thyroidectomy there is an increased risk in iatrogenic injuries. So, when the frequency of complications in recurrent operations and the malignity possibility of the thyroid tissue left behind (15.84% in our study) are taken into consideration, we believe that, despite the higher rate of post-operative complications, TT will be more beneficial in the surgical treatment of benign thyroid disorders, especially those which are bilateral or extended to substernal space or which presented with compression symptoms.
One of the most important limitations of our survey was no comparison between surgery and radioiodine therapy. To give attention to the high rate of thyroid malignancy in this study and low incidence of complication such as temporary RLN injury and no permanent injury to RLN and so parathyroid, total thyroidectomy could be a safe method in surgical treatment of MNG. As respects of breaking out more malignancy in patients with pressure symptom, surgeon should be more sensitive perform total thyroidectomy as soon as possible. Similarly mentioned in this study, FNA did not have any truth value in MNG diagnosis.