1. Introduction
Acute abdominal pain during pregnancy should be evaluated in the same way as during non-pregnancy (1). In examining these patients, diagnosing diseases or identifying potentially life-threatening conditions is of great importance and our first treatment option. In pregnant women, a series of other issues such as acute abdominal and pelvic pains and physiological changes related to pregnancy is of great importance. Due to complications that may affect the baby and the mother, more attention should be paid to pregnant women (2). Since any delay in the diagnosis and treatment of these patients may have irreparable complications and mortality, imaging and laboratory interventions should be considered immediately (3).
In these pregnant patients with acute abdominal pain, the ultimate goal for performing any diagnostic work is to find and quickly identify serious and life-threatening causes and perform immediate interventions. Meanwhile, the symptoms that help us diagnose very serious diseases in these patients include high or low blood pressure fluctuations, very severe and moderate abdominal pain, digestive symptoms, such as vomiting, vaginal bleeding, fever, and a history of abdominal trauma (4, 5).
Since abdominal pain related to pregnancy is much more effective than other causes, the causes of abdominal pain related to pregnancy are examined first. These causes may be associated with symptoms such as vaginal bleeding or fluctuations in blood pressure, which are considered very key symptoms in pregnancy abdominal pain.
In cases where a severe drop in blood pressure is seen in the mother without vaginal bleeding, it can be a sign of severe bleeding, and possible sites of bleeding should be checked, such as the abdomen, vascular organs, and organs such as the spleen (6).
Ovarian vein thrombosis usually presents within 7 days after delivery. Clinically, patients appear very ill, and their accompanying symptoms include back pain, fever, and abdominal pain. In these patients, the right ovarian vein is more probable (80% vs 6%). In 14% of patients, conflict occurs bilaterally. In the examinations, pelvic sensitivity to the touch may bring diagnoses such as ileus, digestive problems, and endometritis (7-10).
Pregnant women with deep pelvic thrombosis may develop high fevers early or up to 3 weeks after delivery. These patients are apparently healthy; fever and chills may be the only clinical signs and findings. There is no tenderness or pelvic pain when palpating the abdomen of these patients, which helps to differentiate it from ovarian vein thrombosis (11, 12).
The computed tomography (CT) scan and magnetic resonance imaging (MRI) are more useful and efficient than ultrasound to diagnose and evaluate pelvic diseases.
2. Case Presentation
A 24-year-old pregnant woman was referred to Ali Ibn Abi Taleb Hospital in Zahedan (southeast of Iran) with fetal death (13 - 14 weeks of gestational age). Based on past medical and obstetric history, she has no problem, and the patient was fasting because of Ramadan.
She received 600 μg of misoprostol intravaginally every 12 hours. The next day, a dead fetus with a placenta was aborted, and 8 hours later, she suffered from the right and left lower quadrant pain with anorexia and vomiting. Abdominal and pelvic ultrasonography, prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), complete blood cell count (CBC), blood urea nitrogen (BUN), creatinine (Cr), urine analysis (U/A), liver function test (LFT), BHCG (blood HCG), and general surgery consultation for rule out of appendicitis were requested (which was normal).
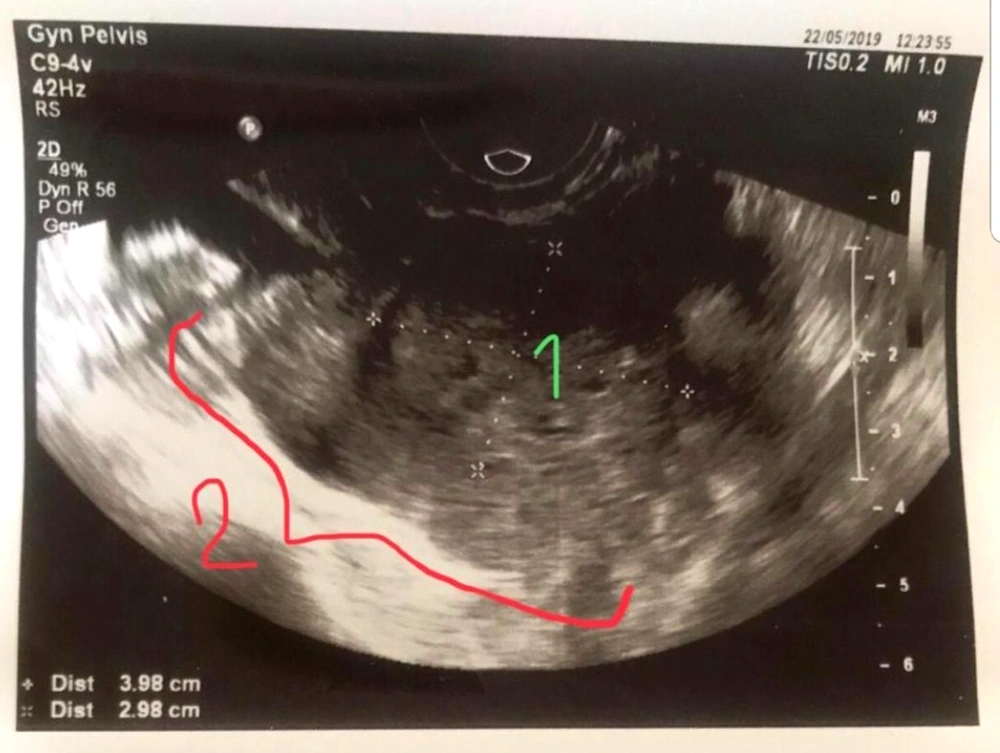
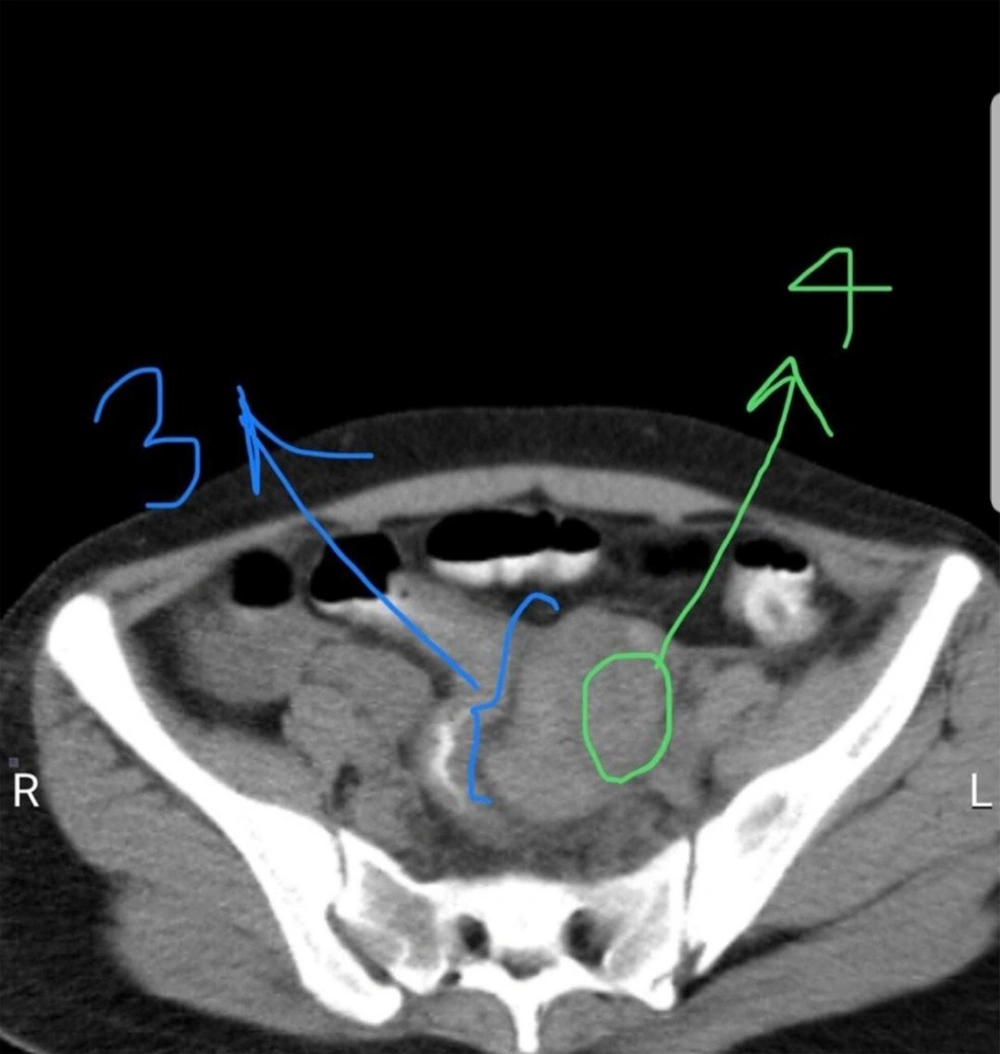
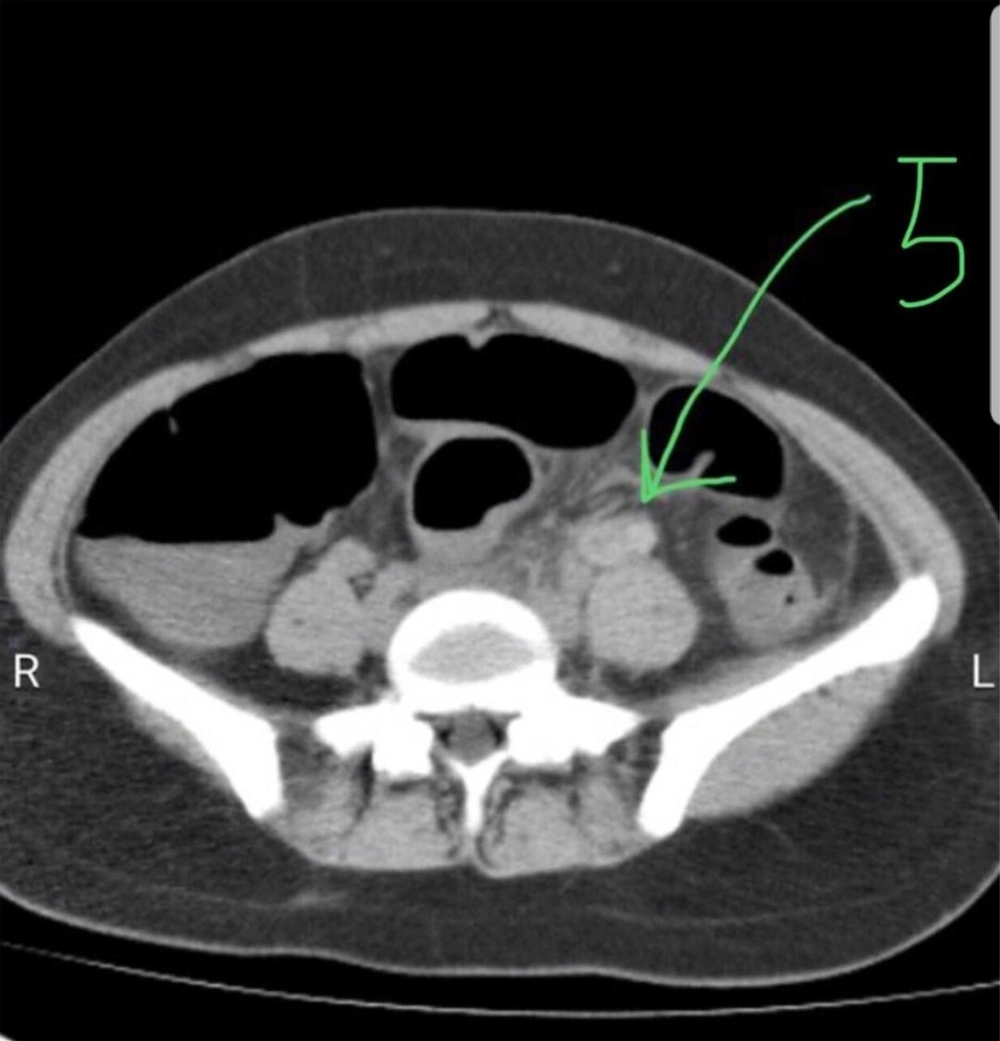
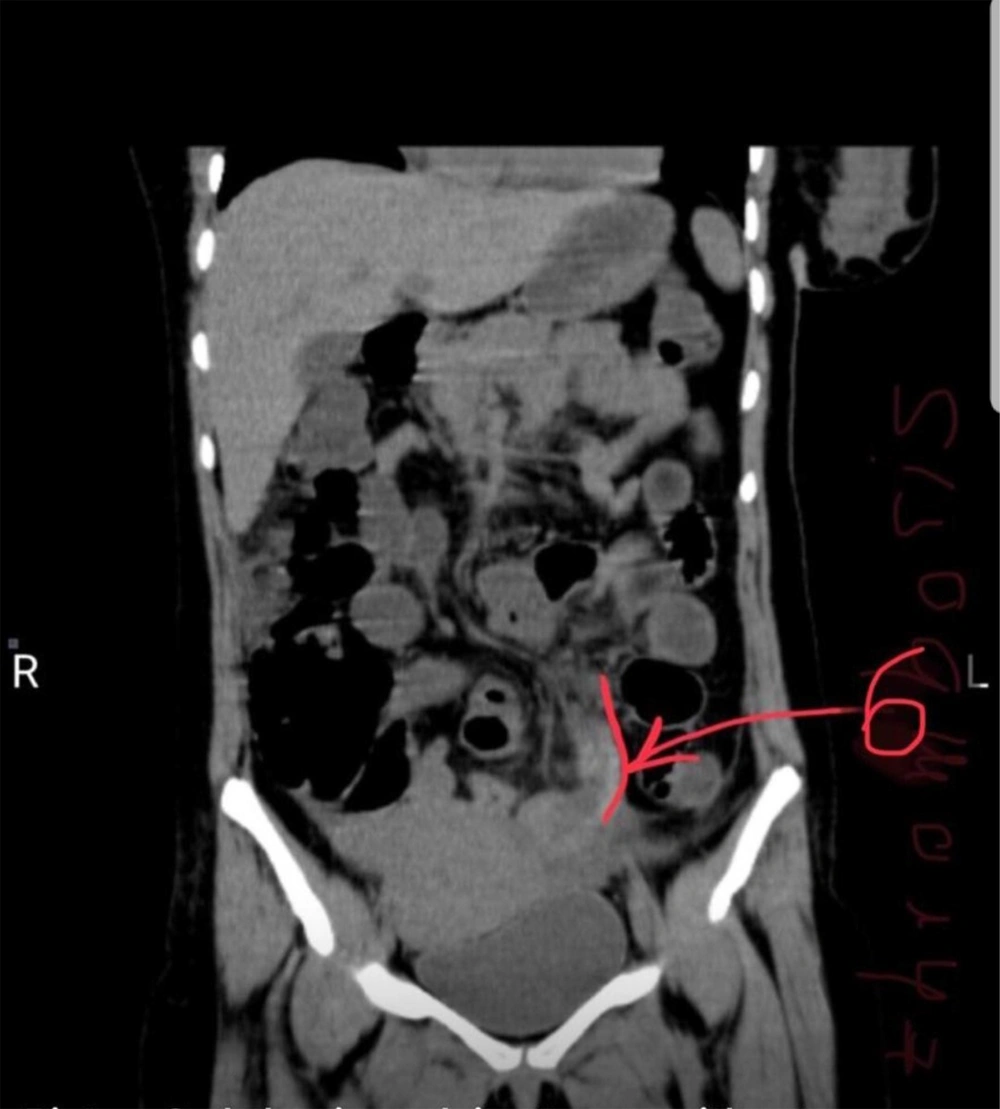
In a transvaginal ultrasound, the left ovarian vein thrombosis was observed. Other organs were normal, and there were no products of pregnancy (Figure 1). An abdominal spiral CT scan with IV and oral contrast (Figures 2, 3 and 4) and without contrast (Figures 5 and 6) confirmed the diagnosis of ovarian vein thrombosis. Other surgical sources of pain and appendicitis were ruled out. Immediately, anticardiolipin (IgG-IgM), anticoagulant lupus (IgG-IgM), b2glycoprotein1 (IgG-IgM), dsDNA, protein C, protein S, antithrombin c were requested that were totally normal. Anticoagulant therapy with heparin started at 5000 IU (initial dose) and 1000 units per hour. Due to thrombocytopenia, heparin was changed to enoxaparin 40 mg (4000 IU) subcutaneously every 12 hours. Right lower quadrant (RLQ) and left lower quadrant (LLQ) pain were suppressed with heparin therapy. After 5 days, warfarin, 5 mg, was started daily in combination with enoxaparin. The patient had complete bed rest (CBR) for 7 days; then, her situation was changed to relative bed rest, and her vital signs were normal. After 12 days, the patient was discharged with warfarin daily.
Blood analyses were carried out (HB = 11, WBC = 85 000, and PLT = 140 000 per μg), and Cr, BUN, LFT, and hypercoagulability work-up were normal. BHCG was 79 mIU/mL the day after the abortion, and 3 days after the abortion, it was10 mIU/ML.
3. Discussion
Ovarian vein thrombosis (actually thrombophlebitis) occurs as a rare complication in women who have given birth. This disease also has severe complications, such as pulmonary embolism. In these people, this disease occurs in the form of acute pelvic pain during the postpartum period, which is suspected to be acute abdominal pain (1).
Austin explained the first case of ovarian vein thrombosis after delivery in 1956 (2). Ovarian vein thrombosis is most commonly found within 7 days to 4 weeks postpartum (3). Ninety percent of cases show signs during the first 10 days after delivery (4). Ovarian vein thrombosis has also been seen as a less common complication in some patients who have undergone pelvic surgeries (5-7). A retrospective study done at the Mayo Clinic examined around 40 patients with ovarian vein thrombosis and found that 34% of ovarian vein thrombosis patients were associated with malignancies, 23% with pelvic inflammatory disease, and 20% with surgeries (8).
The incidence of postpartum ovarian vein thrombosis is 1/600 to 1/2000 deliveries (9). The symptom of clinically significant ovarian vein thrombosis is a pain in RLQ and LLQ and fever, usually appearing approximately 7 days after delivery or abortion without response to antibiotic treatment (9).
In more than 80% of patients, due to the involvement of the right ovarian vein, a lump can be felt during the examination, and in this regard, the left vein prevents infection with the retrograde method. In 14% of cases, there may be bilateral involvement, and only in 6% the left vein is involved (10).
Due to the presence of intestinal gas, ultrasound is very difficult and practically impossible (11).
For ultrasound diagnosis, the presence of tube-shaped hypo-echo structures in the adnexal region next to the ovarian artery and the absence of flow in the case of vein visualization are considered diagnostic by the Doppler method.
In the CT scan diagnosis, they can be identified and evaluated according to the anatomy of the veins and their drainage location (right ovarian vein to the inferior vena cava and left ovarian vein to the left renal vein). The best treatment will be a combination of anticoagulation and antibiotics. However, the appropriate diagnosis is considered in the postpartum patient.
Complications that may occur after ovarian vein thrombosis are the extension of the same thrombosis into the inferior vena cava and pulmonary embolism (12).
Considerations include hydro ureter, and acute appendicitis can be differential for the clinical presentation.
Anticoagulation is the main treatment; traditionally, heparin and warfarin have been used. However, there was no support for the use of new oral anticoagulants (NOACs) in the treatment of ovarian vein thrombosis (12).
Totally the complications of ovarian vein thrombosis can be significant, and the diagnosis relies on a careful examination of the radiographic findings (ultrasound, CT scan, and MRI).