1. Background
A growing body of evidence has shown that positive emotions such as joy, happiness, love, and safety are not necessarily always pleasant, and sometimes, they may even be frightening (1). For instance, some people are not able to experience joy and happiness (i.e., anhedonia), and others may find positive emotions frightening and rather not experience them (2). This phenomenon is called fear of happiness (FOH) and has been well-documented in studies on self-criticism, stress, and major depression (3). According to Joshanloo (4), FOH is a relatively stable belief domain with potentially significant real life consequences. People with FOH believe that joy and happiness cause bad things to happen in their lives. In other words, these people have doubts about the positive value and pursuit of happiness (5). According to this conceptualization, individuals suppress their true positive feelings to avoid the occurrence of bad consequences that they think such positive emotions (e.g., happiness and joy) can cause them to happen (3).
It is assumed that FOH may be influenced by people’s responses to life events, and that suffering from a traumatic event can lead to negative and debilitating consequences. For instance, the individuals experiencing a traumatic event often have reactions such as fear and helplessness (6). However, studies on the relationship between traumatic events and FOH are limited. Sar et al. (7) reported a relationship between childhood traumas and FOH among college students. Regarding the correlation between childhood traumas and other psychological disorders, which can shed light on the relevance and importance of this phenomenon, researchers have noted that traumatic events are not only the core of post-traumatic stress disorders, but also depression, difficulties in emotion regulation, and dissociative personality disorder are among the consequences of repeated exposure to traumatic events (8). Some studies have shown a relationship between childhood traumatic events and adulthood depression and anxiety symptoms (9), obsessive-compulsive symptoms (10), borderline personality symptoms (11), depressive disorders (12, 13), and nonsuicidal self‑injury behaviors (14). Other studies have shown that childhood traumas have been significantly associated with suicidal thoughts and behaviors, paranoid thoughts, bulimia nervosa, schizophrenia spectrum disorders, bipolar disorders, and substance abuse disorders (15).
Most studies related to happiness are based on the assumption that happiness is a worthy goal for anyone and that failure to achieve this emotion is the greatest failure a person can experience (16). Studies on individuals from different cultures have shown that those who have negative views towards happiness or positive emotions may behave cautiously and fearfully in the case of being positioned in a happy situation (17), highlighting the importance of identifying FOH predictors. Although the relationship between childhood traumas and FOH has been confirmed, few studies (7) have examined this relationship. On the other hand, little attention has been paid to the factors mediating and influencing this relationship. Adaptive and maladaptive emotion regulation strategies can mediate the relationship between early childhood traumas and FOH. Early life traumatic experiences change the memory system at the cognitive level, impairing cognitive functioning in various areas, including executive functions, working and implicit memories, and emotional processing (18). Some researchers believe that examining emotion regulation strategies in vulnerable children and adolescents can disclose the biological pathways linking childhood traumas to later life mental disorders (19). The people experiencing traumatic or negative life events often use different emotional regulation strategies to cope with them (20, 21). Cognitive emotion regulation is defined as “the conscious cognitive way of handling the intake of emotionally arousing information” (21).
The ability to regulate emotions in early life is formed in the context of parent-child emotional interactions, and the quality of these interactions plays an important role in determining adulthood emotion regulation capacity. However, this ability is disrupted in children if they encounter traumatic events. Studies have shown that there is a relationship between early-life traumas (e.g., child maltreatment) and the development and utilization of emotion regulation skills. In addition, early childhood traumas can influence adaptive and maladaptive emotion regulation strategies and interpersonal skills (22). Numerous studies have been carried out on the role of emotion regulation in mediating the relationship between childhood traumas and emotion-related mental health problems, including anxiety and depression (9), symptoms of borderline personality (11), nonsuicidal self‑injury attitudes (14), depression (23), and internalizing/externalizing behavioral problems (24).
2. Objectives
There are few pieces of evidence on the relationship between childhood traumas and FOH (7); nevertheless, the relationship between childhood traumas and psychological disorders is well-documented. Given the importance of FOH and the necessity of understanding the psychological mechanisms related to FOH, the main purpose of this study was to investigate the role of cognitive emotion regulation strategies in mediating the relationship between early childhood traumas and FOH.
3. Methods
This was a descriptive correlational study. The statistical population consisted of all students of Islamic Azad University, Kashmar Branch, in 2017 - 2018. To determine the sample size based on the target population (n = 2500), we used the Krejcie and Morgan method, which recommended a sample size of 384 (the maximum sample size in Krejcie and Morgan’s table). An expected dropout rate of 10% was assumed for the estimated sample size, and the final adjusted sample size was determined as 420. Participants were selected by the convenience sampling method. Out of a total of 420 questionnaires received, 378 were found to be accurately and completely answered. The data was analyzed by structural equation modeling (SEM), LISREL 8.8, and SPSS version 24 software. The following instruments were used to collect data.
The Cognitive Emotion Regulation questionnaire (CERQ) was developed by Garnefski et al. (25) to assess cognitive emotion regulation strategies. It is a 36‑item self‑report measure. Each item is rated on a 5-point scale from 1 [(almost) never] to 5 [(almost) always]). It has nine subscales, including the self-blaming, rumination, catastrophizing, blaming others, acceptance, positive refocusing, refocusing on planning, positive reappraisal, and putting into perspective. Cronbach’s alpha coefficients for the subscales ranged from 0.71 to 0.81 (25). Besharat and Bazzazian (26) confirmed the validity and reliability of the Persian version of this questionnaire. They reported an appropriate internal consistency reliability, test-retest reliability, content validity, as well as convergent and discriminant validities. In addition, Cronbach’s alpha coefficients for the subscales were reported between 0.67 and 0.89 (26).
The Childhood Trauma questionnaire (CTQ) was developed by Bernstein et al. (27) to assess the severity of different types of childhood traumas. It is a 28‑item self‑report measure scored on a 5‑point scale ranging from 1 (never) to 5 (very often). It has five subscales, including emotional abuse (α = 0.87), emotional neglect (α = 0.91), physical abuse (α = 0.83), physical neglect (α = 0.61), and sexual abuse (α = 0.92). Garrusi and Nakhaee (28) reported that the scale had an appropriate validity. Also, test-retest reliability coefficients for the subscales were reported from 0.60 to 0.86.
The Fear of Happiness scale (FHS) was developed by Joshanloo (4) and is a 28‑item self‑report measure. Each item is rated on a 7-point scale from 1 (strong disagreement) to 7 (strong agreement). The psychometric characteristics of the scale were confirmed across 14 countries by reporting Cronbach’s alphas from 0.51 (the Indian version) to 0.88 (the Persian version). The predictive validity of the FHS was shown to be appropriate. The results of confirmatory factor analysis (CFA) indicated that the model appropriately fitted in almost every culture. These indices were also excellent (χ2 = 4.01, df = 4, P > 0.05, TLI = 1, CFI = 1, and RMSEA = 0.004) for the Persian version of the scale (5). Exploratory factor analysis (EFA), CFA, and Cronbach’s alpha coefficient were used to examine the validity and reliability of the Persian version of FHS, respectively. The KMO index was obtained 0.89, and the Bartlett test of sphericity was significant (P > 0.01, χ2 = 1353.74). Therefore, principal component analysis (PCA) with a varimax rotation was carried out for factor analysis, which posited a single-factor structure. This factor explained 76.31% of the total variance of FHS. Cronbach’s alpha for the four items was obtained 0.9. The results of CFA also showed good fit indicesindices (χ2 = 8.06, df = 5, P > 0.05, CFI = 1, NFI = 1, AGFI = 0.97, GFI = 0.99, and RMSEA = 0.052).
4. Results
Out of a total of 420 questionnaires distributed, 378 met the criteria for further analysis. Others either were not returned or identified as incompletely answered. Out of 378 respondents, 209 (55.29%) were females, and 169 (44.71) were males. From all the subjects studied, 210 (55.56%) were under 25 years of age, 89 (23.54%) were between 25 to 30 years of age, 56 (14.81%) were between 31 to 35 years of age, and 23 (6.09) were above 36 years of age. Table 1 shows the correlation matrix and provides the descriptive indices of research variables. The correlation coefficients presented in Table 1 supported the hypothesis of the lack of linearity in the multiple regression model. Our results showed the highest statistically significant positive correlation between the physical and sexual abuse dimensions (P = 0.75). On the other side, the lowest (and non-significant) correlation was observed between the catastrophizing and positive reappraisal dimensions.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | ||||||||||||||||
| 2 | 0.70** | 1 | |||||||||||||||
| 3 | 0.66** | 0.75** | 1 | ||||||||||||||
| 4 | 0.72** | 0.51** | 0.54** | 1 | |||||||||||||
| 5 | 0.58** | 0.52** | 0.62** | 0.63** | 1 | ||||||||||||
| 6 | 0.25** | 0.21** | 0.18** | 0.19** | 0.17** | 1 | |||||||||||
| 7 | 0.05 | 0.08 | 0.06 | 0.05 | 0.10* | 0.66** | 1 | ||||||||||
| 8 | 0.31** | 0.20** | 0.15** | 0.25** | 0.18** | 0.71** | 0.56** | 1 | |||||||||
| 9 | 0.23** | 0.16** | 0.19** | 0.24** | 0.13** | 0.15** | 0.10** | 0.22** | 1 | ||||||||
| 10 | -0.29** | -0.25** | -0.28** | -0.30** | -0.28** | -0.18** | -0.15** | -0.38** | -0.32** | 1 | |||||||
| 11 | -0.11** | -0.16** | -0.22** | -0.11** | -0.17** | -0.15** | -0.14** | -0.16** | -0.007 | 0.15** | 1 | ||||||
| 12 | -0.17** | -0.22** | -0.23** | -0.13** | -0.22** | -0.15** | -0.19** | -0.15** | -0.14** | 0.16** | 0.43** | 1 | |||||
| 13 | 0.25** | 0.19** | 0.26** | 0.14** | 0.24** | 0.29** | 0.26** | 0.31** | 0.13** | -0.33** | -0.29** | -0.32** | 1 | ||||
| 14 | 0.18** | 0.21** | 0.20** | 0.06 | 0.21** | 0.36** | 0.37** | 0.40** | 0.13** | -0.34** | -0.36** | -0.37** | 0.71** | 1 | |||
| 15 | 0.23** | 0.26** | 0.33** | 0.19** | 0.26** | 0.39** | 0.29** | 0.42** | 0.13** | -0.37** | -0.39** | -0.32** | 0.69** | 0.72** | 1 | ||
| 16 | 0.16** | 0.19** | 0.22** | 0.06 | 0.16** | 0.30** | 0.32** | 0.37** | 0.14** | -0.37** | -0.35** | -0.33** | 0.63** | 0.70** | 0.74** | 1 | |
| 17 | 0.25** | 0.28** | 0.30** | 0.16** | 0.24** | 0.29** | 0.20** | 0.35** | 0.16** | -0.39** | -0.34** | -0.31** | 0.71** | 0.69** | 0.72** | 0.69** | 1 |
| Mean | 8.57 | 6.42 | 5.47 | 7.80 | 6.21 | 15.79 | 15.63 | 15.69 | 18.06 | 23.98 | 16.56 | 10.34 | 1.82 | 1.96 | 1.71 | 1.84 | 1.73 |
| ± SD | 4.41 | 2.90 | 2.97 | 3.78 | 2.74 | 4.55 | 6.10 | 5.90 | 3.05 | 5.12 | 4.45 | 4.89 | 1.17 | 1.11 | 1.02 | 1.09 | 1.12 |
a*, P < 0.05; **, P < 0.01.
bNote: 1 = emotional abuse, 2 = physical abuse, 3 = sexual abuse, 4 = emotional neglect, 5 = physical neglect, 6 = self-blaming, 7 = other-blaming, 8 = rumination, 9 = catastrophizing, 10 = positive/planning refocusing, 11 = positive reappraisal, 12 = acceptance, 13 = fear of happiness first item, 14 = fear of happiness second item, 15 = fear of happiness third item, 16 = fear of happiness forth item, 17 = fear of happiness fifth item.
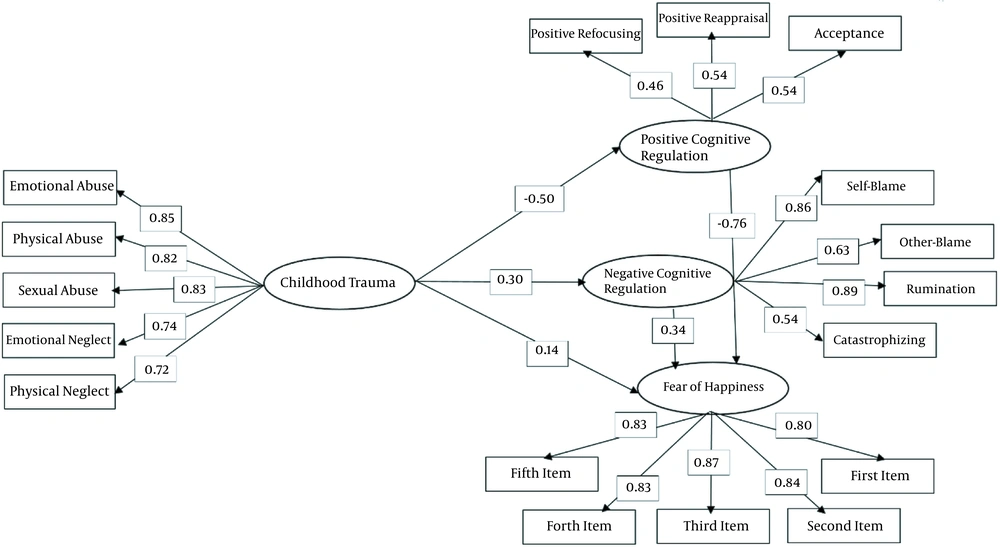
In Figure 1, the coefficients of the hypothetical model are presented. The path coefficients of the endogenous and exogenous variables have also been shown in Table 2.
| Effects | Predictor Variable | Criteria Variable | β | SE | t | P |
|---|---|---|---|---|---|---|
| Direct | Childhood trauma | Positive cognitive emotion regulation | -0.50 | 0.09 | 5.55 | < 0.01 |
| Negative cognitive emotion regulation | 0.30 | 0.06 | 5.26 | < 0.01 | ||
| FOH | 0.14 | 0.08 | 1.75 | > 0.05 | ||
| Positive cognitive emotion regulation | FOH | -0.76 | 0.14 | -5.43 | < 0.01 | |
| Negative cognitive emotion regulation | FOH | 0.34 | 0.05 | 6.59 | < 0.01 | |
| Indirect | Childhood trauma on FOH | Via positive and negative cognitive emotion regulation | 0.48 | 0.09 | 5.60 | < 0.01 |
| Total | Childhood trauma on FOH | Via positive and negative cognitive emotion regulation | 0.34 | 0.06 | 5.98 | < 0.01 |
According to Figure 1 and Table 2, the direct effects of childhood traumas on positive (β = -0.50) and negative (β = 0.30) cognitive emotion regulation were significant, but the direct effect of childhood traumas on FOH was non-significant (β = -0.14). The direct effects of positive (β = 0.76) and negative (β = 0.34) cognitive emotion regulation on FOH were also significant, and the indirect effects of childhood traumas on FOH based on positive and negative cognitive emotion regulation rendered the β value of 0.48. Also, the total effect of childhood traumas on FOH via both positive and negative cognitive emotion regulation was positive and meaningful (β = 0.34). In Table 3, the direct hypothesized model of fitness indices has been presented.
| Index | χ2 | df | GFI | CFI | NFI | IFI | NNFI | AGFI | RFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|---|
| Fit | 501.18 | 114 | 0.86 | 0.94 | 0.92 | 0.94 | 0.93 | 0.82 | 0.91 | 0.095 |
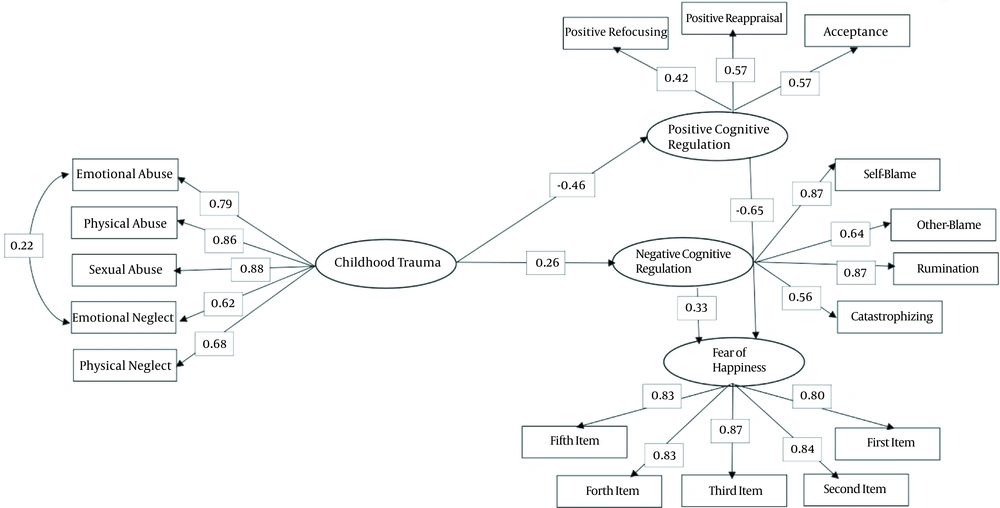
The results of Table 3 show that the chi‑square, GFI, CFI, NFI, IFI, NNFI, AGFI, RFI, and RMSEA indices were equal to 501.18 (P > 0.01), 0.86, 0.94, 0.92, 0.94, 0.93, 0.82, 0.91, and 0.095, respectively, so the values of GFI, CFI, NFI, and AGFI were greater than 0.90, but RMSEA was lower than 0.10. These indices indicate the relative fitness of the model into the data. We also used modification indices to change the model’s structure since some patch coefficients were statistically insignificant. The coefficients of the modified model have been presented in Figure 2. After eliminating the direct path of childhood maltreatment to FOH and connecting emotional abuse to emotional neglect, the values of GFI, CFI, NFI, IFI, NNFI, AGFI, RFI, and RMSEA were equal to 344.56 (P > 0.01), 0.90, 0.96, 0.94, 0.96, 0.95, 0.87, 0.93, and 0.074, respectively, implying that the model fitted into the data.
5. Discussion
The main purpose of this study was to investigate the mediating role of cognitive emotion regulation in the relationship between childhood traumas and FOH. Our results showed that childhood abuse and neglect could lead to FOH in students by using more maladaptive cognitive emotion regulation strategies (self-blaming, rumination, catastrophizing, and other-blaming) as well as less use of adaptive cognitive emotion regulation strategies (acceptance, positive refocusing, and positive reappraisal). Although no research was found to be consistent with the findings of the present study, Our results were consistent with a number of previous studies’ findings (9, 11, 14, 23, 24, 29-31), suggesting that cognitive emotion regulation could mediate the relationship between childhood traumas and psychological problems or disorders (e.g., anxiety, depression, post-traumatic stress disorder, borderline personality, nonsuicidal self-injury, internalizing/externalizing behavioral problems). On the other hand, only one study was found to examine the relationship between childhood traumas and FOH (7), which its results were consistent with those of the present study.
Huh et al. (9) found that the total score of maladaptive cognitive emotion regulation mediated the relationship between childhood traumas and the severity of adulthood depression and anxiety symptoms in people with depressive disorders, but the total score of adaptive cognitive emotion regulation was not a mediator of this relationship. When comparing the findings of the two studies, one should notice that the recent study was conducted on people with depressive disorders, but we enrolled university students in the present research. Khoramimanesh and Mansouri (11), in a recent study conducted on female-headed households, also reported that maladaptive cognitive emotion regulation strategies and negative spiritual coping strategies mediated the relationship between a history of traumas and borderline personality symptoms. Furthermore, Ghaderi et al. (14) reported that the relationship between early-life traumas and nonsuicidal self‑injury in adolescents was mediated by emotion regulation and intolerance of uncertainty. Researchers in the recent study enrolled adolescents and used the Difficulties in Emotion Regulation scale (DERS). Hopfinger et al. (23), in a study on patients with major depressive disorder and using the Emotion Regulation Skills questionnaire (ERSQ), found that deficits in general emotion regulation mediated the association between childhood traumas and depression. In a report from South Korea, Choi and Ja (24) reported that emotion dysregulation (measured by an emotion regulation checklist) mediated the relationship between cumulative childhood traumas and internalizing/externalizing behavioral problems in sexually abused children aged 6 - 13 years. The results of John et al. (29) showed that difficulties in emotion regulation) affected the relationship between a history of child abuse and current PTSD/depression severity in adolescent females, and Fossati et al. (30) found that emotion dysregulation mediated the link between childhood traumas and adulthood attachment and borderline personality disorder. Finally, Gratz et al. (32) showed that emotion dysregulation mediated the relationships of maltreatment and negative intensity/reactivity with borderline personality symptoms. All these studies emphasize that emotion regulation can mediate the relationship between childhood traumas or maltreatment and the development of psychological problems and disorders during later life. However, there are methodological differences (scales, samples, etc.) between these studies.
Huh et al. (9) presented several theories for emotion regulation development. Based on the biosocial and attachment theory, the maladaptive emotion regulation strategies originating from childhood traumas or invalidating environments can cause vulnerability to psychological problems (i.e., depression and anxiety). Based on the cognitive behavioral theory, the maladaptive appraisal of negative life events may be at the core of psychological dysfunctions. According to the social learning theory, emotionally-neglected individuals may have had deficient opportunities to learn adaptive strategies through caregiver modeling, which makes them vulnerable to psychological problems in adulthood (9). The results of the present study indicated that childhood traumas, by using more maladaptive strategies (self-blaming, rumination, catastrophizing, and other-blaming) and less use of adaptive strategies (acceptance, positive refocusing, and positive reappraisal) could lead to FOH in students.
The present study has some limitations. First, this was a cross-sectional study. Second, this study was conducted on a group of students, but future research can be carried out on a group of people with a history of childhood traumas. Third, in this study, a non-random sampling method was used; other studies can use probability sampling methods. Fourth, using self-report measures could have affected the results of the present research because of various reasons such as bias and social desirability responses. The findings of the present study recommend that mental health professionals should investigate a history of childhood traumas in individuals with mental problems and perform psychological interventions such as dialectical behavior therapy concerning the type of traumas and the time of its occurrence. Mental health professionals and researchers can also use the results of the present study to better understand mediators of the relationship between childhood traumas and FOH.