1. Introduction
Coronavirus disease 2019 (COVID-19) is an emerging disease with a rapid increase in incidence and mortality since its first detection in Wuhan, China, in December 2019 (1). The causative agent is potentially deadly and a major concern for the World Health Organization (2). The most common symptoms of COVID-19 include fever, cough, and fatigue. Other symptoms entail sputum, headache, bleeding, diarrhea, indigestion, and lymphopenia (3-6). Diagnostic symptoms are abnormal findings on chest radiography, lymphopenia, leukopenia, and thrombocytopenia (6, 7). The onset of COVID-19 symptoms varies from 6 to 41 days, with an average of 14 days until death. This period depends on the age and immune system of the patient, which is shorter in patients over 70 years of age than in patients under 70 years (8).
Intrauterine transmission of COVID-19 is contradictory (1, 9). During pregnancy, the body is affected by physiological changes (10), such as decreased functional residual volume, diaphragm height, and altered cellular immunity, which lead to higher susceptibility to viral infections and worse disease consequences (9). Limited studies report that viral diseases sometimes occur during pregnancy, along with an augmented risk of maternal illness and death (11) and congenital anomalies (e.g., measles and varicella) (12). A study by Alzamora et al. showed that COVID-19 during pregnancy results in respiratory failure, mechanical ventilation, and preterm delivery. This adds to the growing evidence about worse maternal outcomes in pregnancy (9). Overall, 21% of pregnant mothers with COVID-19 were discharged without serious complications (13). Limited information is available about COVID-19 during pregnancy, treatment, and its complications (1). Therefore, this study reported a positive coronavirus case in pregnancy that was released after treatment with an excellent general condition and healthy fetus.
2. Case Presentation
A 30-year-old woman on the third pregnancy with two previous cesarean sections, including a live baby and a sudden infant death syndrome. She did not know the exact date of the last menstrual period. According to the ultrasonography, she was 18 weeks pregnant. She had no medical history and worked as a service in a limited surgical center. She reported a mild cough on 2020/3/16, went to the health center, and was visited by the center's doctor. Diphenhydramine syrup was prescribed, and she was sent home. The next day, on 2020/3/17, the coughs increased, and she had shortness of breath, a fever of 38 degrees, and blood pressure of 140/90. Other asses factors entailed: (1) fetal heart rate (FHR) = 156; (2) O2 saturation = 97; (3) pulse rate (PR) = 100; (4) respiratory rate (RR) = 30; (5) blood pressure (BP) = 140/90; and temperature (T) = 38.
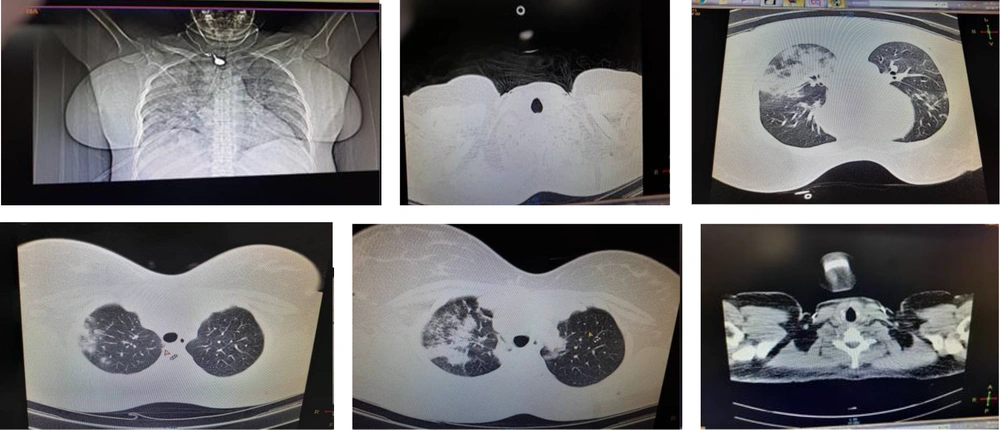
Oxygen therapy and serum therapy were performed, and complete blood count differential (CBC diff), fasting blood sugar (FBS) tests were requested. The results of the laboratory assessment included: (1) hemoglobin (Hb) = 12; (2) FBS = 75; (3) leukopenia, and positive C-reactive protein (CRP). The electrocardiogram (ECG) was taken from the patient, and the result was normal. Aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), and bilirubin were requested, the results of which were normal. The patient was visited by a gynecologist and had no obstetric problems, and the fetal heart rate was normal. She was visited by an infectious disease specialist due to shortness of breath. A computerized chest tomography (CT) scan was performed, showing scattered involvement of both lungs (photo number one). The patient was transferred to the isolated room. Chloroquine, vancomycin, selenium zing, seroflo spray, and B complex were prescribed daily. In addition, three doses of immunoglobulin were given intravenously.
The patient had stress and tachycardia, and the center's counselor spoke to her. It was better for her to continue oxygen therapy with a mask until the seventh day, after which the patient would breathe easily. Serum therapy was continued. On the seventh day, the fever stopped, and the CT of the lungs was repeated, indicating that lung involvement had reduced. The CBC diff was also repeated every other day, and pregnancy ultrasonography was performed. The ultrasound findings were normal, and the gestational age was approximately 18 weeks. After thirteen days, the patient was discharged with the medications prescribed.
For 10 days, she used cefixime pills, diphenhydramine syrup, pantoprazole capsules, and seroflo spray. During the two weeks of quarantine, blood pressure was monitored daily, ranging from 110/70 to 140/90. After quarantine, she went to a gynecologist and had CBC diff, Glocuse, 2 hour post prandial (2hpp), liver function tests (LFT), and 24-hour urine tests. The results of all these tests were normal. The one-hour blood sugar was 198, based on which following a diet was recommended. The only complication that persisted for the patient was high blood pressure, which had to be monitored daily. The patient monitors her blood pressure at home and does not currently take medication for high blood pressure. Written consent was obtained from the patient to obtain a history (Figure 1).
3. Discussion
In our case, the pregnant woman with COVID-19 showed a similar pattern of clinical features compared to non-pregnant adults (14). According to the report of Rasmussen et al., the common manifestations in hospitalized patients included fever (83 - 100%), cough (82 - 84%), myalgia (11 - 35%), headache (7 - 8%), and diarrhea (2 - 10%). On chest radiographs, all patients had abnormalities. In the presented case, the patient first had a cough, followed by fever, and both lungs were shown to be affected in the CT scan (1).
Pregnant women are particularly at risk for respiratory illness and severe pneumonia due to the slight suppression of the immune system during pregnancy, part of the physiological changes during pregnancy (7, 15). Due to data constraints, there is no evidence that pregnancy increases sensitivity to COVID-19 (16, 17). In a study by Karami et al., a pregnant woman had leukopenia, lymphopenia, elevated creatinine, positive CRP, and blood pressure of 100/60. In our study, an increased blood pressure of 140/90, leukopenia, and positive CRP were observed (18).
Alzamora et al. reported a patient with fever, fatigue, and general weakness. The patient's pulse was 131 beats/min, respiration rate was 38 breaths/min, and oxygen saturation was 99% with fraction of inspired oxygen (FiO2) at approximately 90%. The findings showed high D-dimer and slightly high glucose. Reverse transcription-polymerase chain reaction (RT-PCR) was performed, showing a positive result. The immunoglobulin G (IgG) and immunoglobulin M (IgM) were negative on the first day after delivery and positive on the fourth day (9). In the current study, fever, positive CRP, and slightly higher glucose were found.
Breslin et al. reported a patient hospitalized on week 37 of pregnancy due to high blood pressure (19). The patient had asthma and type 2 diabetes. Patients with fever are suspected of chorioamnionitis and are given ampicillin, gentamicin, and acetaminophen. The RT-PCR following coughing and shortness of breath was positive. Treatment with hydroxychloroquine (600 mg twice daily for 1 day and 400 mg daily for the next 4 days) was considered in the same study. The patient was given hydroxychloroquine at the same dose, along with azithromycin and ceftriaxone for another 37 weeks with fever, cough, and shortness of breath.
In our study, the patient experienced changes in blood pressure (19). In a study by Lou and Bob, triple antibiotics (i.e., gentamicin, metronidazole, and cefazolin) were given for possible chorioamnionitis to a patient with 40 weeks of fever and positive RT-PCR (20). Wang et al. reported a 30-week-pregnant patient with fever who tested positive in RT-PCR and had scattered turbidity in the CT scan of the lungs. The latter case was treated with arbidol tablets (0.2 g orally every 8 h), lopinavir, and ritonavir tablets (400/100 mg orally every 8 h), sodium cefoperazone, sodium sulbactam (0.3 g intravenously every 8 h), and human serum albumin (20 g intravenously daily). Furthermore, dexamethasone and magnesium sulfate were given to prevent preterm labor. The patient's condition could deteriorate, and she was at risk of preterm birth (21).
In a case report by Khan et al., a 34-week and 5-day pregnant woman with fever and cough had a positive RT-PCR test. The medications used for this patient were intravenous azithromycin, oral Lianhua Qingwen capsules (Chinese medicine), and the antiviral agent oseltamivir (22). According to Liu et al., based on the mother's condition, the decision to terminate pregnancy could be made despite the preterm birth due to the initiation of antiviral medicines in pregnant women (23).
3.1. Conclusions
All patients, including pregnant women, should be evaluated for fever and respiratory infection symptoms. In most reports, antiviral agents, immune-boosting medications, and oxygen therapy have been used for treating pregnant women with COVID-19, which have been effective. These measures were also used in our case and were found to be effective. If you have symptoms, such as fever, cough, or any other respiratory problem, get checked. Ideally, the screening process should begin before entering the maternity ward or pregnancy care clinic. For example, when planning appointments, patients should be instructed that if they have respiratory symptoms on the day of the appointment or if the patient has symptoms before visiting, respiratory signs and symptoms should be evaluated by telephone before referral.