1. Background
Headache is one of the most prevalent types of pain (1), which imposes a very economic burden on patients, their families, healthcare systems, and societies worldwide (2). One of the most common types of primary headache is migraine, which is characterized by recurrent pulsatile headaches (3). Migraine is often described as an episodic or chronic neurovascular brain disorder (4). The most common form of migraine characterized by recurrent disabling headache and associated autonomic symptoms is migraine without aura (MWO) (4, 5). Based on previous studies, migraine affects 12% of the general population globally (6). In Iran, about 14% of people have been suffering from migraine, which is higher than that reported worldwide (7). Migraine leads to loss of financial resources and reduces work capacity and productivity and also individuals’ quality of life (8).
Despite many efforts, the exact cause of migraine is still unknown, and there is no definitive cure for that; thus, management of this disease is necessary (9, 10). According to the literature, many patients with migraine will have other problems that aggravate their tendency to headaches, including anxiety, depression, and other pain syndromes such as fibromyalgia syndrome (FMS). Proper management of these is essential to maximize the effect of any other migraine treatments (8, 11). FMS is an idiopathic chronic pain syndrome characterized by generalized body pain, tenderness of tender point areas in palpation, and constitutional symptoms (12). It is estimated that the prevalence of FMS in the general population of Iran has been 4% (13).
Both migraine and FMS can stimulate the nervous system (8). The FMS patients were 1.3 times more likely to experience headaches than those without coexisting FMS (12). Several studies regarding comorbid FMS in migraine patients have shown a high incidence of FMS in patients with migraine, among other symptomatic headaches. It is suggested that the existence of FMS indicates a more severe migraine (4, 8, 14-16). Since in comorbidity, the specific treatment of a disease has been shown to improve the symptoms of other diseases (17). Therefore, it is necessary to investigate the association between FMS and migraine.
2. Objectives
This study aimed to investigate the effect of comorbid FMS on migraine severity between migraineurs with and without FMS based on demographic and clinical grounds.
3. Methods
3.1. Study Design and Participants
This cross-sectional observational study was conducted at the Al-Zahra Hospital in Isfahan, Iran between 2015 and 2016. The study was approved by the Human Research Committee of Islamic Azad University of Medical Science (Najafabad branch) and carried out in accordance with the principles stated in the 1975 Declaration of Helsinki.
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, as reflected in a prior approval by the institution's human research committee.
After a sufficient explanation of the objectives and study design, written informed consent was obtained from all participants. In this study, 80 outpatients aged 18 - 65 years with a definitive diagnosis of MWO, according to the most recent diagnostic criteria of the International Headache Society (IHS) (18), were diagnosed by a special experience neurologist. Additionally, the participants had to understand and complete the study questionnaires. Patients were excluded from the study if they were not willing to continue the study or for whatever reason they wanted to leave it, had a history of diabetes mellitus, neurological or psychiatric disorders (previously diagnosed), and also showed any chronic pain (except Fibromyalgia Syndrome) or acute pain (except for fibromyalgia flare-up). Initially, information on sociodemographic characteristics (age, gender, marital status, and education) was recorded on the registration form. Then, the following self-report questionnaires for the clinical diagnosis of FMS with the Fibromyalgia Survey Questionnaire (FSQ-P) (19), severity of migraine with the Headache Impact Test 6 (HIT-6) (20), and quality of life with the Migraine-Specific Quality of Life Questionnaire (MSQ) were completed by all patients (21).
3.2. Statistical Analysis
All statistical analyses were performed using SPSS 22.0 software. All data were analyzed using the Fisher’s exact test, chi-square test, student t-test, two-way ANOVA, and Pearson correlation coefficient. Categorical variables were expressed as numbers and percentages, while continuous variables were expressed as mean ± standard deviation (SD). Also, logistic regression analysis was employed to calculate the odds ratio (OR) as the estimate of the relative risk of the different variables for FMS in patients with migraine. Additionally, internal consistency was measured by Cronbach's alpha test, which showed the reliability of the questionnaires. P-value of less than 0.05 was considered to be statistically significant.
4. Results
Overall, 80 patients who had MWO, aged 38.1 ± 12 years (min - max: 18 - 63 years), were enrolled in the study. Male/female ratio was 21/59 (26.2%/73.8%) in our study. Based on this analysis, MWO was less prevalent in single (11.2%) than married patients (88.8%), and the frequency of education level was higher in those patients with less than diploma (43.8%), diploma, and associate (35%), and bachelor and over (21.2%) (Table 1). Generally, the results showed that the frequency of comorbid FMS was 22.5% among patients with MWO. In addition, the mean migraine severity and quality of life scores in these patients were 62.7 ± 8.3 (min - max: 40 - 78) and 45.66 ± 15.49 (min - max: 27.7 - 64), respectively. According to the results, Cronbach's alpha coefficients of the internal consistency for FSQ-P, HIT-6, and MSQ questionnaires were 0.74, 0.77, and 0.82, respectively, which indicated the appropriate reliability of these questionnaires.
| Variables | Values |
|---|---|
| Demographic Data | |
| Age (y) (min - max) | 38.1 ± 12 (18 - 63) |
| Gender | |
| Male | 21 (26.2) |
| Female | 59 (73.8) |
| Marital status | |
| Single | 71 (88.8) |
| Married | 9 (11.2) |
| Education level | |
| Less than diploma | 35 (43.8) |
| Diploma and associate | 28 (35.0) |
| Bachelor and above | 17 (21.2) |
| Clinical Data | |
| Fibromyalgia syndrome (FSQ-P) | |
| FMS (+) | 18 (22.5) |
| FMS (-) | 62 (77.5) |
| Migraine severity (HIT-6) (min - max) | 62.7 ± 8.3 (40 - 78) |
| Quality of life (MSQ) (min - max) | 45.66 ± 15.49 (27.7 - 64) |
The comparative analysis of demographic and clinical characteristics of MWO in patients with (+) and without (-) a history of FMS is shown in Table 2. In this study, the mean age of patients with FMS was significantly higher than patients without FMS (49.3 ± 10 vs. 34.8 ± 10.5, P < 0.001). In this study, regardless of age, there was no significant difference in the demographic characteristics of patients suffering from migraine with and without FMS. Interestingly, the mean life quality scores in MWO patients suffering from FMS were higher than in MWO patients without FMS (52.4 ± 11.6 vs. 43.7 ± 16, P = 0.035). According to the MSQ, lower scores indicate better quality of life. In addition, according to logistic regression analysis, age (OR = 1.1, 95% CI = 1.006 - 1.2, P < 0.001] and quality of life (OR = 1.03, 95% CI = 1.002 - 1.07, P = 0.04) were the predictive factors for FMS in migraine patients.
| Variables | FM (+) Migraine Patients (n = 18) | FM (-) Migraine Patients (n = 62) | P-Value |
|---|---|---|---|
| Demographic data | |||
| Age (y) | 49.3 ± 10 | 34.8 ± 10.5 | < 0.001 |
| Gender | 0.294 | ||
| Male | 3 (16.7) | 18 (29.0) | |
| Female | 15 (83.3) | 59 (71.0) | |
| Marital status | 0.086 | ||
| Single | 0 (0.0) | 9 (14.5) | |
| Married | 18 (100.0) | 9 (85.5) | |
| Education level | 0.233 | ||
| Less than diploma | 11 (61.1) | 24 (38.7) | |
| Diploma and associate | 4 (22.2) | 24 (38.7) | |
| Bachelor and above | 3 (16.7) | 14 (22.6) | |
| Clinical Data | |||
| Migraine severity (HIT-6) | 62.8 ± 7.3 | 62.7 ± 8.6 | 0.962 |
| Quality of life (MSQ) | 52.4 ± 11.6 | 43.7 ± 16 | 0.035 |
Comparative Analysis of Demographic and Clinical Characteristics in Migraine Without Aura Patients with (+) and Without (-) Fibromyalgia Syndrome a
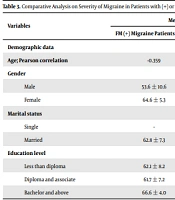
The comparative analyses revealed that the mean migraine severity in patients with (+) or without (-) a history of FMS had no significant difference based on demographic characteristics (Table 3). Based on these analyses, the mean migraine severity was higher in females migraineurs than in males with and without FMS; however, these differences were not statistically significant (P = 0.066).
| Variables | Mean Migraine Severity | P-Value | |
|---|---|---|---|
| FM (+) Migraine Patients (n = 18) | FM (-) Migraine Patients (n = 62) | ||
| Demographic data | |||
| Age; Pearson correlation | -0.359 | -0.130 | 0.144, 0.313 |
| Gender | 0.066 | ||
| Male | 53.6 ± 10.6 | 62.5 ± 9.4 | |
| Female | 64.6 ± 5.3 | 62.8 ± 8.4 | |
| Marital status | NA | ||
| Single | - | 60.4 ± 11.8 | |
| Married | 62.8 ± 7.3 | 63.1 ± 8.1 | |
| Education level | 0.470 | ||
| Less than diploma | 62.1 ± 8.2 | 64.0 ± 9.3 | |
| Diploma and associate | 61.7 ± 7.2 | 62.5 ± 8.1 | |
| Bachelor and above | 66.6 ± 4.0 | 60.8 ± 8.6 | |
Comparative Analysis on Severity of Migraine in Patients with (+) or Without (-) Fibromyalgia Syndrome Based on Demographic Characteristics a
5. Discussion
Migraine, with a prevalence of 5 - 20%, is one of the main factors of patients’ disability, which can reduce their work capacity, productivity, and quality of life and impose a huge economic burden on societies. On the other hand, 2 - 4% of people are affected by FMS worldwide, which is a cause of noticeable functional impairment (4). Although pain distributions are different, migraine and FMS are often encountered as comorbid with each other (5, 8, 12). It has been indicated that there is an association between migraine and FMS due to a common pathophysiological mechanism (10, 22). Improving evidence suggests that central sensitization phenomena play a role in the pathogenesis of both migraine and FMS (23, 24). This study was conducted on 80 patients aged 38.1 ± 12 years suffering from MWO to assess the effect of comorbid FMS on migraine severity in the aforementioned patients, regarding both demographic and clinical grounds. A high proportion (73.8%) of patients were women, which is justified by the higher prevalence of MWO in females (25). The frequency of comorbid FMS was 22.5% among patients with MWO, which was considered high, according to the reported ratios in the general population (4, 14). This was in agreement with the previous reports by Marcus et al. (12) and Ifergane et al. (8). However, in a reverse study carried out by Vij et al., it has been reported that 55.8% of the patients with FMS suffer from migraine (11). High prevalence of FMS proves the importance of screening and diagnosis of FMS in patients with MWO. Early diagnosis and proper treatment of FMS may reduce disability of patients with migraine and significantly improve the quality of their personal and social life (26).
Based on our study, the mean age of patients with MWO who concomitantly had FMS was significantly higher than those without FMS. In other words, the elderly population with MWO was more likely to be affected by FMS. Therefore, screening and early diagnosis for older patients should be given more attention. Nevertheless, it was in conflict with the findings reported by Marcus et al. (12), and this may be due to different demographic features of the studied population. Based on our findings, the number of female migraineurs with FMS was higher than female migraineurs without FMS; however, it was not significant. No statistically significant difference was seen between females and males in both FMS (+) and FMS (-) migraine patients.
The results obtained were almost similar to previous studies conducted by Marcus et al. (12). Regarding marital status and level of education, no significant difference was seen between two groups of FMS (+) and FMS (-) migraine patients. Generally, it was shown that demographic variables, including gender, marital status, and education levels, might not be relevant to the incidence of FMS in patients with MWO. Therefore, these demographic variables are not appropriate for screening in migraine patients. In this study, it was displayed that migraine severity was not related to FMS. In other words, the severity of migraine was similar in migraineurs with and without FMS. This was in line with the previous reports by Marcus et al. and Ifergane et al. (8, 12). It should be noted that evaluation of migraine severity in these two groups (with FMS and without FMS) with other standard questionnaires, as well as the increase in the number of patients with FMS may lead to different results. Based on our findings, the quality of life in MWO patients with comorbid FMS was significantly lower than those without FMS. Several studies have indicated that there is an association between migraine and quality of life as migraineurs have a poor quality of sleep, as well as family and social life, due to the debilitating nature of migraine (8, 12, 27, 28). Simultaneous development of FMS may increase the negative burden of disease and the degree of disability (12).
Our data revealed that the severity of migraine had no significant relationship with age (P = 0.167), gender (P = 0.066), marital status (P = NA), and education level (P = 0.470) of migraine patients with and without FMS. Our findings showed that the mean migraine severity was higher in female patients with FMS than in male migraineurs without FMS. It was almost similar between female and male patients without FMS but not significantly different (P = 0.066). Hence, females with MWO who simultaneously suffer from FMS experience a more severe headache than men with matched conditions (15). According to these findings, it is highlighted that physicians should be aware of the high prevalence of FMS among patients with migraine and consider the possible role of migraine as a trigger for the FMS. Generally, all patients with MWO should be screened for FMS because some studies have revealed that early diagnosis will result in better outcomes (26). Based on our study, older migraine patients and also women with migraine with FMS should be considered a special group for screening. Therefore, early diagnosis of FMS in old female patients with MWO is necessary because it results in eliminating the severity of migraine pain and increasing patients’ social and personal quality of life.
In conclusion, FMS did not affect the severity of migraine in patients with MWO, but the high prevalence of comorbid FMS among migraineurs strengthens a possible association between these diseases, which highlights the importance of screening and early diagnosis of FMS during management of the patients with MWO. Accordingly, early diagnosis and proper treatment of FMS may result in improving migraine patients' disability as well as quality of life. The results of this study revealed that older MWO patients are more likely to develop FMS and MWO patients with FMS have a lower quality of life. However, gender, marital status, level of education and migraine severity score did not show a significant difference between the two groups of migraineurs with and without FMS. Finally, this study showed that the FMS did not have a significant impact on the severity of migraine in patients with MWO; however, further studies are needed to understand the effect of the comorbid FMS on migraine.