1. Background
Autism spectrum disorders [ASD] are characterized by difficulty in social communication, and repetitive and restricted behaviors and interests [1], but they lie on a continuum [2]. The term “broader autism phenotypes” represents that there is a quantitative difference between patients and non-patients. Clinicians have differentiated high functioning autism spectrum disorder [HFASD] from low functioning Autism spectrum disorder in terms of intelligence. Higher IQ is correlated with higher levels of psychological problems in HFASD [3]. Depression is the most common disorder in ASD and HFASD [4-6]. It was reported in a sample of 54 persons with HFASD that 70% of the participants had experienced at least major depression one time. It is also found that 50% of this population suffered from reoccurring episodes of major depression [7]. Depression has a host of aversive influences upon relationships, cognitive performance, and the physical health [8], leading to a decrease of personal health and the increase of treatment cost [9]. When depression is coupled with an ASD, it can lead to a significant decrease of well-being and influence functioning [10]. On one hand people with ASD have higher levels of depression [11], and on the other hand depression is the most frequent comorbid psychological disorder in this population [12]. Features of ASD may complicate observation of depressive symptoms and consequent diagnosis. Pre-existing symptoms of autism easily maske some symptoms of depression, including symptoms related to concentration, sleep, and communication of affect via facial expression or intonation [13]. Additionally, many depressive symptoms, including tearfulness and sadness [13], decreased self-care [14], psychomotor retardation [15], apathy, anhedonia, and loss of interest in activities [16] which are common in the general population are likely to be observed in people with comorbid ASD. The rate of depression in ASD is as high as 34 per cent [13] and the relationship between depression and autism has been confirmed in some in western studeis [7, 17-19]. However, a research showed less than 2 percent qualified for a diagnosis of major depressive disorder [20].
Hence, the results about the prevalence of depression in people with HFASD are contradictory. This inconsistency of results may lead to a lack of diagnosis and treatment, exacerbating the prognosis of ASD and depression. Similarly, it is not known which factors can predict the depression. Noteworthy, it is necessary to investigate cultural differences in manifestation of autistic phenotypes, because cross-cultural studies showed culture can impact on manifestation of autistic phenotypes [21]. Although a study investigated the relationship between depression and the autism-spectrum features in the Iranian female participants [22], no study has addressed this issue in men. In fact, ASD is more common in men than women, ranging from 4:1 in ASD [23]. Since the symptoms of ASD lead to impairment, other psychopathological symptoms- such as depression- are ignored and they are not the focus of diagnosis and treatment, making worse the central ASD symptoms [24], impacting negatively the family, and leading to significant increase of stress in autistic people’s caregivers [25]. Therefore, this paper is aimed at investigating the relationship between depression and autistic characteristics and the factors which can predict depression in men.
2. Methods
This cross-sectional study was conducted in Shahed University in 2016. Only male students were participated in this study. Researchers have indicated that a minimum sample size of 100 is necessary for structural equation models [SEM] [26]. 180 questioners were distributed, but the data of 120 students were appropriate to analysis. Subjects were selected based on the cluster sampling from four faculties, including faculty of humanities, engineering, basic sciences, and agricultural faculties. Informed consent was obtained from all subjects. The subjects were assessed on the depression [BDI-II] and the autism-spectrum quotient [AQ].
Beck depression inventory-II: this inventory is developed by Beck, Steer & Brown in 1996 [27] and is composed of 21 items. Studies conducted on this Inventory reported its desired reliability, validity and factor structure. Researchers [28] reported internal consistency ranging from 0.73 to 0.92 and alpha coefficient for the group of patients 0.86 and non-patients 0.81. BDI-II has positive correlations with self-report measures of depression and anxiety [29]. Also Iranian researchers [30] reported an alpha coefficient of 0.92 for outpatients, 0.93 for students. The convergent validity of BDI-II was confirmed using depression subscale of brief symptoms inventory.
The autism-spectrum quotient [AQ]: AQ was developed by Baron-Cohen et al. in 2001 [31]. These researchers included 50 questions in this questionnaire that measures five areas presented for autism spectrum traits, including social skills, attention switch, communication, attention to detail and imagination. Internal consistency has been reported as follows: communications [0.65], social skills [0.77], imagination [0.65], attention to details [0.63] and attention switch [0.67]. The results of factor analysis showed AQ has five subscale. A Persian translation of the AQ was used in the current study [32]. The reliability of this questionnaire within an interval of three weeks was 0.82 and Cronbach’s alpha was acceptable.
Data were analysed in SPSS 23 and AMOS. Descriptive results and Pearson correlation were calculated in SPSS, and structural equation modeling [SEM] was performed in AMOS. SEM provides researchers with the chance to examine causal effects [33].
3. Results
120 male students participated in this study, with a mean age of 21/11 [SD = 2]. Participants include 28 students from faculty of humanities [23.3 percent], 81 students from engineering faculty [67.5 percent], 9 students from basic sciences faculty [7.5 percent], and 2 students from agriculture faculty [1.7 percent]. Results presented in Table 1 shows the descriptive findings.
| Variable | Depression | AQ Total | Attention to Details | Imagination | Communication | Attention Switching | Social Skills |
|---|---|---|---|---|---|---|---|
| Mean | 12.233 | 21.091 | 5.362 | 4.079 | 3.308 | 5.316 | 3.025 |
| S.D | 9.2115 | 5.596 | 1.594 | 1.5917 | 2.020 | 1.687 | 1.896 |
| Skewness | 1.020 | 0.471 | 0.310 | 0.581 | 0.787 | -0.034 | 0.606 |
| Kurtosis | 0.792 | 0.366 | 0.299 | 1.910 | 0.586 | -0.164 | 0.375 |
Descriptive Findings of the Depression and Autism-Spectrum Quotien
Table 1 shows that Kurtosis and Skewness lie within the acceptable range for normal distribution of data. As a matter of fact, Hair [34] argued that data is considered to be normal if Skewness is between ‐2 to +2 and Kurtosis is between ‐7 to +7.
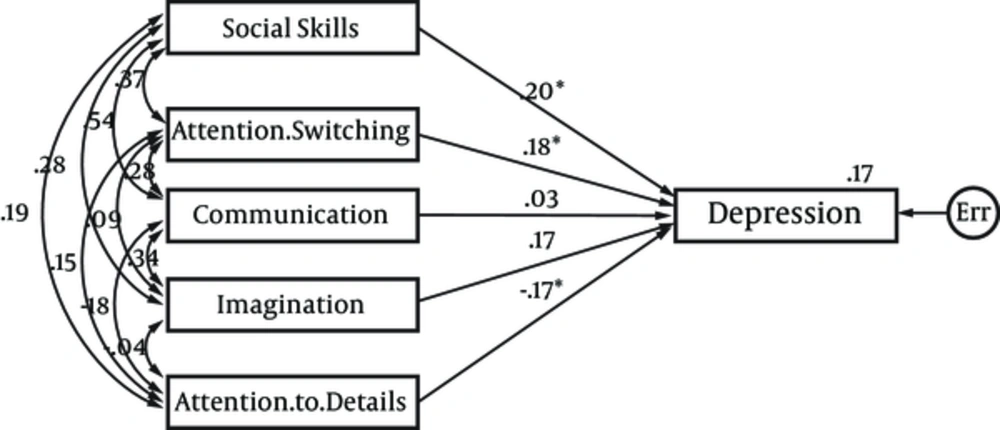
Table 2 shows that depression has a significant and positive relationship with four components of autism-spectrum quotient, including social skills [r = 0.299, P < 0.001], imagination [r = 0.26, P < 0.004], Attention Switching [r = 0.251, P < 0.006], and communication [r = 0.214, P < 0.019]. In order to obtain a more optimal calculation related to combination of the components of autism-spectrum quotient in prediction of depression, effects of five components of autism-spectrum quotient on depression were calculated simultaneously. Figure 1 shows the result of this effects after controlling the measurement error and overlap among components of Autism-Spectrum Quotient.
Figure 1 shows that after controlling the measurement error and overlap among components of autism-spectrum quotient, social skills [r = 0.20, P < 0.05], attention switching [r = 0.18, P < 0.05], and attention to details [r = -.17, P < 0.05] had significant effects on depression. Since the model was a saturated model [df = 0], no fitness indices were calculated.
4. Discussion
This research indicated there is a significant relationship between depression and broader autism phenotype in men. This result is consistent with earlier findings [7, 17-19]. In order to explain these findings it should be noted that some researchers believe the cause of the depression in people with HFASD is increased awareness of their deficit in interaction and communication with others [35]. In fact, people with HFASD have a higher intellectual level, leading to increased awareness of problems in the field of social interactions that is the predictor of the depression [35, 36]. It should be noted that intellectual level is considered as an important factor in dealing with ASD. Higher intellectual levels boost social comparison and deficit insight [37, 38]. Many studies investigated the relationship between different intellectual level, symptoms of autism and depression in people with ASD. For examples researchers [39] investigated 1,202 people with ASD with a wide range of intellectual levels and showed that a higher cognitive level and less serious symptoms in the spectrum were predictive of a higher risk of depression. Many higher functioning people with ASD have awareness of their social problems, resulting in the development of comorbid psychological disorders and higher psychopathology [40]. Researchers [25] suggested a correlation between depression and greater self-consciousness of social difficulties and problems. They showed people with ASD that are aware of their social problems are likely to experience more emotional pain and sadness in the face of social failures. Higher consciousness of failures in social life plays a significant role in increasing discouragement and lowering self-esteem [37], and leads to a significant increase of the risk of depression [41]. People with ASD have higher levels of helplessness, anxiety, and rejection by society. They also experience low quality of life, weak mental health, and restricted adaptive and social functioning [42].
Secondly, people with poor quality social relationships have the risk of stress, negative effect, loneliness, developmental psychopathologies, and depression [43]. This study showed social skills have a significant effect on depression. Hence, it is possible that loneliness plays a significant role in greater levels of depression. Researchers showed a significant correlation between social problems and negative state of mind in people with HFASD [38], anxiety and depression [44]. Some researchers believe that people with HFASD prefer loneliness, whereas some researchers showed that people with HFASD prefer social interaction, but they do not have the necessary abilities for social interaction [37]. People with HFASD prefer to experience greater exposure to their peers and to social stimulation than individuals with a lower level of cognitive functioning. This preference brings about a greater level of stress. This stress and increased social demands may result in depression [38]. Researches show a two-sided relationship between negative social self-perception and difficulties with peers. According to these studies combination of aforementioned factors predicts depression [39]. Similarly, researchers [40] showed that there is a correlation between the poorer quality of friendship to greater loneliness and depression in people with HFASD.
Thirdly, cultural differences may explain this finding. According to cross-cultural findings, there are significant differences between the West and the East cultures in terms of attention to detail and general. Abel and Hsu [45] presented Rorschach cards to Chinese subjects born in China and America and showed that Chinese subjects born in America more than other group focused on detailed points, while subjects born in China compared with Chinese subjects born in America perceived points as a general pattern. Additionally, culture can impact on manifestation of autistic phenotypes [21]. For example, researchers investigated autistic traits' signs on a sample of Western subjects [723 English students] and Eastern subjects [271 Hindi students and 245 Malaysian students] and showed that behaviors associated with autistic traits in Eastern culture occur more than Western culture. Also, in this research, Hindi subjects compared to other subjects had higher scores on the imagination sub-scale and Malaysian subjects had higher scores in sub-scale of attention switching. Thus, it is possible that different autistic phenotypes or the magnitude of phenotype expression influence the mediating impact of social problem solving on depression as a function of culture.
Last but not least, it is possible that gender differences in brain explain this finding. This study showed that attention switching had a significant impact on depression in men. The extreme male brain [EMB] [46] considers two psychological dimensions, including “systemizing” [S] and “empathizing” [E]. Systemizing is considered as the tendency and drive to analyze a system according to its basic regularities and as a result to create systems exploiting those regularities. Empathizing is considered as the drive to understand and identify people’s mental state, as well as to react and respond with a suitable emotion. It should be noted that women are stronger empathizers and men are stronger systemizes. Hence, the ‘extreme male brain’ theory suggests autism represents an extreme of the male pattern [impaired empathizing and enhanced systemizing].
This research had some limitations. First, this study was conducted on a student sample which limits the generalization of the findings. Secondly, the role of other variable related to HFASD was not investigated. According o researches, anxiety is another common problem in HFASD. Additionally, the role of underlying mechanisms, including the executive functioning problems in the link between ASD and depression has not been studied in this research. So, it is suggested that future research investigate the role of anxiety and the executive functioning problems in clinical sample.
In conclusion, Adults with HFASD commonly experience depressive symptoms. The differentiation between the symptoms of depression and ASD enable clinicians to diagnose and treat these disorders in the initial phase. The diagnosis of depression prevents from exacerbating the ASD symptoms and increasing conflict in autistic people’s caregivers.