1. Background
Abdominal pain is one of the most common complaints during pregnancy and is always discussed due to its various differential diagnoses (1). Appendicitis means the inflammation of the appendix. Appendicitis occurs due to the obstruction of the lumen of the appendix by feces (2). Stool stasis often causes this phenomenon, and lymphoid hyperplasia, neoplasms, and plant parasites are other possible causes of obstruction (3).
Acute appendicitis is the most common complication requiring surgery during pregnancy, and its prevalence is reported to be 1 in 1,500 pregnant women (4). The diagnosis of appendicitis in pregnant women is more challenging than in nonpregnant women (5). Based on evidenced studies, acute appendicitis during pregnancy in 30 - 35% of cases is diagnosed later (6). Ultrasound in pregnancy is not very valuable for the diagnosis of appendicitis. In addition, computed tomography is avoided due to the presence of ionizing radiation in pregnancy, especially in the first trimester (7).
Classically, in appendicitis, initial abdominal pain will be in the periumbilical area and right lower quadrant (RLQ). As the appendiceal wall becomes inflamed, visceral afferent fibers are stimulated; these fibers enter the spinal cord at T8-T10, producing the classic diffuse periumbilical pain and nausea observed at the onset of appendicitis. Pain might be accompanied by one of several symptoms, including anorexia, nausea/vomiting, fever, diarrhea, generalized weakness, and increased urinary frequency or urgency (8).
Some patients might present with unusual clinical features. In these patients, the pain interrupts sleep; in addition, the patient might rarely complain of pain during walking or coughing. Clinical diagnostic findings are often important in primary appendicitis. Symptoms of peritoneal inflammation also include Mcburney’s point pain, Rovsing’s sign, and Dunphy’s sign (8).
Acute appendicitis is diagnosed in 1 in 800 to 1,500 pregnancies (9), which is more common in the second trimester (10). Maternal morbidity and mortality following delivery are low and comparable to nonpregnant women (11). The risk of intrauterine fetal demise (IUFD) during uncomplicated appendicitis is 2%; however, in the presence of generalized peritonitis and peritoneal abscess, it might increase to 6% (12). If the appendix ruptures, the risk of IUFD might increase to 36% (13). The prevalence of preterm labor due to appendectomy will be 4%, and with complications will be 11%. The association of negative appendectomy with preterm labor and fetal death is 10% and 4%, respectively (12).
The physician’s strong clinical suspicion, along with the use of appropriate and advanced paraclinical procedures, could reduce the incidence of diagnostic mistakes (13). There are several tests to help diagnose appendicitis, some of which include Rovsing’s sign (i.e., the presence of RLQ ( left lower quadrant) pain on palpitation, the abductor sign (i.e., the pain of the RLQ in the inner rotation of the buttocks), and the psoas sign (14). Pregnant women, especially in late pregnancy, do not usually show the classic symptoms of appendicitis because the appendix might be displaced by the enlarged uterus; then, the pain will be in the right upper quadrant (8, 15-19), and abdominal tenderness is less common during pregnancy. Due to the risks of unnecessary appendectomy, routine imaging is recommended in all pregnant women with suspected appendicitis to obtain an accurate diagnosis.
The initial study begins with an ultrasound in the RLQ at the point of maximum sensitivity. Ultrasound has the advantage of easy availability in normal pregnancy (19) and is helpful in providing information regarding the well-being of the fetus and ruling out preterm labor. However, the criteria for diagnosis in the United States are the same as for nonpregnant patients; these criteria include an enlarged, inflamed appendix (greater than 6 mm), immobility, and noncompression (8, 19). However, ultrasound is an operator-dependent technique, and the presence of a large uterus during pregnancy reduces the sensitivity of ultrasound (78%) and its specificity (83%) (19).
The incidence of appendicitis in Andersson and Lambe’s 2001 study was 0.06 (8). In Al-Dahamsheh’s study, the prevalence of appendicitis was 0.28 (20). In Bhandari et al.’s study on acute appendicitis and pregnancy in developed countries, the incidence of appendicitis was reported as 1 per 800 cases (0.12%) (21). Yuk et al.’s study showed that the incidence of acute appendicitis in South Korea was 110 out of 100,000 pregnant women (2). In a study by Mehdizadeh et al., the most common cause of acute abdomen was ectopic pregnancy with 62% and then ruptured ovarian cysts (27%), torsion of the ovary (10%), and acute appendicitis (1%), respectively (22). Bazdar et al. stated that 58 (9.94%) out of 584 patients who had appendicitis were pregnant women (23).
2. Objectives
Given the importance of appendicitis during pregnancy, it was decided to investigate the frequency of appendectomy in Zahedan, Iran. By explaining the epidemiology of one of the most important causes of acute abdominal pain, it is possible to have appropriate diagnostic and therapeutic strategies according to patients’ chief complaints.
3. Methods
The present study was a retrospective study. The studied population included pregnant women who referred to Ali Ebn-e Abitaleb hospital in Zahedan, Iran and underwent appendectomy from April 2015 to March 2019. In this study, 76 hospital files from 2015 to 2019 were reviewed and evaluated. Before the evaluation of patients, 58 cases were finally reviewed, and 19 women were excluded due to incomplete information. In this study, no restriction was considered the inclusion criteria.
The present descriptive study examined the frequency of appendectomy in pregnant women who referred to Ali Ebn-e Abitaleb hospital after obtaining an ethics code. By referring to the hospital archives, the researchers examined the hospital records of pregnant women who underwent appendectomy within April 2015 to March 2019. Finally, the information, such as age, gravidity, gestational age, abdominal tenderness, axillary temperature, clinical signs, complications of appendectomy, type of surgery, and white blood cells (neutrophil), were evaluated. SPSS software (version 21) was used for data analysis, and frequency distributions were determined using descriptive statistics, central and dispersion indices, charting, and table setting.
4. Results
Overall, out of 73,576 studied pregnancies, only 58 women were observed with definite appendicitis. Only 0.08% of the studied population underwent appendectomy. The mean age of the studied population was 28.1 ± 5.8 years.
In the present study, 47% and 53% of women were primiparous and multiparous, respectively. The most common pain in patients was RLQ pain. The mean gestational age of the studied women was 24.8 ± 4.9 weeks. Furthermore, the mean axillary temperature of the studied patients was 36.9°C.
The RLQ tenderness, nausea, rebound tenderness, and migratory pain, with prevalence rates of 87.93%, 75.9%, 70.7%, and 65.5%, were the most common clinical symptoms of patients in this study (Table 1). Additionally, the most common complication was reported as wound infection, with a prevalence of 10.3% (Table 2). The highest number of surgeries performed in this study belonged to laparotomy appendectomy. The mean number of leukocytosis in the present study was 12870 ± 8per microliter, and the mean percentage of neutrophils was 87.11 ± 18.21.%
| Variables | Values |
|---|---|
| Duration, d | 3.38 ± 1.66 |
| Generalized pain | 27 (46.5) |
| Tenderness in the right lower quadrant | 51 (87.93) |
| Rebound tenderness | 41 (70.7) |
| Migration of pain | 38 (65.5) |
| Grading | 12 (20.7) |
| Body temperature (°C) | 36.9 ± 1.01 |
| T > 38.5 | 12 (20.7) |
| Anorexia | 31 (53.4) |
| Nausea | 44 (75.9) |
| Vomiting | 34 (58.6) |
a Values are expressed as No. (%) or Mean ± Standard Deviation.
| Variables | Total (n = 58), No. (%) |
|---|---|
| Complications | |
| Wound infection | 6 (10.3) |
| Abdominal abscess | 1 (1.72) |
| Pneumonia | 3 (5.2) |
| DVT (deep vein thrombosis) | 2 (3.44) |
5. Discussion
Yuk et al., regarding the relationship between pregnancy and acute appendicitis in South Korea, reported that 110 out of 100,000 pregnant women had acute appendicitis (2). In the present study performed in Ali Ebn-e Abitaleb subspecialty hospital, a very crowded referral center throughout the vast province of Sistan and Baluchestan, about 0.1% of women who referred to the hospital had definite acute appendicitis. The incidence of appendicitis in Andersson and Lambe’s study was 0.06% (8). Al-Dahamshehetal suggested that the prevalence of appendicitis in pregnancy was 0.28% (20). In a study by Behandari et al. on acute appendicitis during pregnancy in developed countries, the incidence of appendicitis was reported as 1 per 800 cases (0.12%) (21).
The prevalence of appendicitis in pregnancy in the present study was the same as in other studies. In addition, in the current study, the most important finding was pain and tenderness in the RLQ (right lower quaderant) area. However, nausea and leukocytosis have also been widely observed in other studies. As a result, the findings of the present study are consistent with the findings of the aforementioned studies. Other studies have shown that the most common symptoms during pregnancy with appendicitis, pain in the RLQ, are the same as the common symptoms of appendicitis in normal individuals (3, 12, 14, 24).
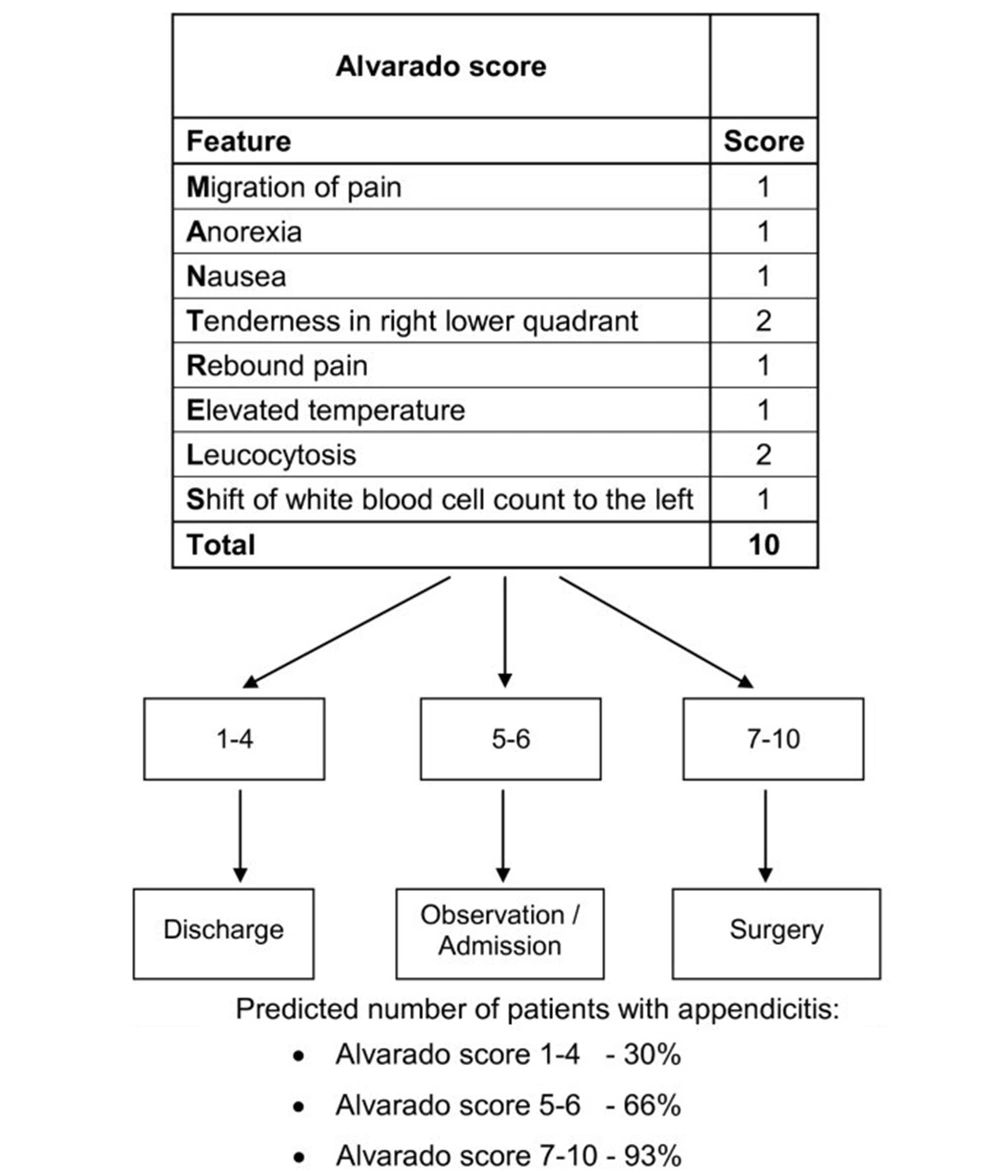
Meanwhile, the results of this study showed that pregnant women with acute appendicitis were associated with longer symptoms, lower body temperature, and postoperative pneumonia. The results of this study are comparable to previous studies (25-28). It was previously believed that acute appendicitis during pregnancy was associated with atypical symptoms and should be treated as soon as possible with surgery, which was associated with a higher rate of negative appendectomy during pregnancy (28). Abdominal surgeries are also associated with adverse pregnancy outcomes; however, the results of the present study suggest that acute appendicitis in pregnancy has similar characteristics in comparison to those of nonpregnant women. This issue is reflected in a significant number of clinical signs and Alvarado scores (Figure 1).
The results of the present study showed pain and tenderness in McBurney’s point, and nausea were high in pregnant women with appendicitis. However, one of the important findings was the low diagnostic value of ultrasound.