1. Background
Individual armament and violence is increasing all over the world and is a preventable public health problem that needs to be solved urgently (1, 2). Gunshot injuries (GSIs) affect the pediatric age group and adults, and the rate of GSIs in innocent children is increasing daily in many countries (3). In the United States of America (USA), approximately 7000 children are hospitalized every year due to GSIs (4). In the USA, GSI-related deaths are the third most common cause of mortality in children aged 1 - 17 years (5). In the pediatric age group (range: 0 - 19 years), the second most common cause of death due to trauma (25% of pediatric deaths) is GSIs (after motor vehicle accidents), and it is the cause of more than 25% of all pediatric deaths reported in trauma centers (6, 7). Almost half of all children who survive GSIs, which is a significant cause of morbidity in the pediatric age group, are discharged from the hospital with disabilities, and 8.2% of them develop a long-term disability, primarily neurological (8). These data show that trauma care is essential not only for survival but also for functional outcomes.
2. Objectives
This study aimed to describe the injuries that occurred in children aged 0 - 16 years who were brought to the emergency department (ED) of Şehitkamil State hospital in Gaziantep, Turkey, due to GSIs. In addition, the current study aimed to reveal the duration of intensive care unit (ICU) stay, surgical needs, demographic characteristics, and mortality rate of the patients.
3. Methods
This study was conducted in the ED of Şehitkamil State hospital in Gaziantep. The approval of the Ethics Committee was obtained from Gaziantep University (date: 24/03/2021; decision no.: 2021/06). This study was both descriptive and retrospective. The ED is the child trauma center of the city. There is a trauma unit with a capacity of 10 beds and accepting only children aged 0 - 16 years. It is run by a pediatric surgery clinic. Child trauma cases (approximately 5%) constitute a significant workload of the ED, which receives 400,000 - 500,000 emergency patient admissions annually.
3.1. Data Collection
This study retrospectively scanned the records of children aged 0 - 16 years admitted to the ED with GSIs within 01/01/2014 to 30/09/2020. The ED anamnesis forms, picture archiving and communication system records, inpatient epicrisis, surgery notes, and consultation notes of the patients were reviewed. Moreover, this study analyzed patients’ age groups, genders, injury sites, presence of internal organ/vessel/bone injuries at the first admission (i.e., all organs in body cavities, vital or significant vessel injuries, and all bone fractures are included in this definition), surgical needs (within 7 days), trauma ICU hospitalization periods, and mortality data.
3.2. Inclusion/Exclusion Criteria
Pediatric GSI cases aged 0 - 16 years that occurred within the borders of Gaziantep province during a 7-year period when the study was planned were included in the study. The GSIs, which occurred due to war (Syrian civil war) or terrorist acts, and patients referred to other external centers after their first intervention were excluded from the study. Patients older than 16 years of age and missing information in hospital records were also excluded from the study.
3.3. Statistical Analysis
The compliance of the data with normal distribution was examined using the Kolmogorov-Smirnov test. The student’s t-test was used to compare customarily distributed features in two independent groups. The Mann-Whitney U test was used to compare non-normally distributed features in two independent groups. The Kruskal-Wallis test was used to compare the features in more than two separate groups. The relationships of categorical variables were analyzed using the Pearson and exact chi-square tests. Mean ± standard deviation, minimum and maximum for numerical variables, number and percentage values for categorical variables are presented as descriptive statistics. SPSS software (version 24.0) was used for statistical analysis, and P < 0.05 was considered statistically significant.
4. Results
A total of 66 GSI cases were included in the study. The mean age of the patients was 9.33 ± 4.05 years, and most patients were male (n = 54, 81.8%). The most common injury was in the abdominal region. Internal organ/vessel/bone injuries were detected in 59.1% of the cases (n = 39). Surgical operation was applied to 60.6% of the cases (n = 40) within 7 days. The mortality rate was 12.1% (n = 8). The length of stay in the trauma unit was 4.34 ± 4.33 days (Table 1).
| Parameter | Values |
|---|---|
| Age | 9.33 ± 4.05 (1 - 16) |
| Gender | 66 (100) |
| Male | 54 (81.8) |
| Female | 12 (18.2) |
| Region of injury | |
| Head-neck | 15 (22.7) |
| Thorax | 15 (22.7) |
| Abdomen | 20 (30.3) |
| Upper extremity | 5 (7.6) |
| Lower extremity | 11 (16.7) |
| Internal organ/vascular/bone injuries | |
| Yes | 39 (59.1) |
| No | 27 (40.9) |
| Surgical operation in 7 days | |
| Yes | 40 (60.6) |
| No | 26 (39.4) |
| Outcome | |
| Discharge | 58 (87.9) |
| Exitus | 8 (12.1) |
| Duration of ICU stay | 4.34 ± 4.33 (0 - 15) |
| Discharge | 4.91 ± 4.3 (0 - 15) |
| Exitus | 0.25 ± 0.5 (0 - 15) |
Abbreviation: ICU, intensive care unit.
a Values are expressed as mean ± standard deviation (min-max) or No. (%).
In this study, 20.5% of the cases with internal organ/vessel/bone injuries at the first admission were mortal. In these cases, more frequent surgery was required within 7 days, and the duration of ICU stay was longer (5.79 ± 4.95 days) (P < 0.005). No significant relationship was observed between the presence of internal organ/vascular/bone injuries and the site of damage at the first admission (Table 2).
| Parameter | Internal Organ/Bone/Vascular Injuries | P-Value b | |
|---|---|---|---|
| Yes (n = 39) | No (n = 27) | ||
| Outcome | 0.017 | ||
| Discharge | 31 (79.5) | 27 (100) | |
| Exitus | 8 (20.5) | 0 (0) | |
| Surgical operation | 0.010 | ||
| Yes | 29 (74.4) | 11 (40.7) | |
| No | 10 (25.6) | 16 (59.3) | |
| Duration of ICU stay | 5.79 ± 4.95 (0 - 15) | 2.26 ± 1.87 (0 - 6) | 0.008 |
| Region of injury | 0.513 | ||
| Head-neck | 11 (28.2) | 4 (14.8) | |
| Thorax | 10 (25.6) | 5 (18.5) | |
| Abdomen | 11 (28.2) | 9 (33.3) | |
| Upper extremity | 2 (5.2) | 3 (11.1) | |
| Lower extremity | 5 (12.8) | 6 (22.3) | |
Abbreviation: ICU, intensive care unit.
a Values are expressed as mean ± standard deviation (min-max) or No. (%).
b P-values were obtained from the exact and Pearson chi-square tests.
Although most discharged patients (86.2%) were male, half of the patients who died were male. Internal organ/vascular/bone injuries were present in all cases who died. No relationship was observed between the need for surgery within 7 days and the outcome (Table 3).
| Parameter | Outcome | P-Value b | |
|---|---|---|---|
| Discharge (n = 58) | Exitus (n = 8) | ||
| Gender | 0.031 | ||
| Male | 50 (86.2) | 4 (50) | |
| Female | 8 (13.8) | 4 (50) | |
| Internal organ/vascular/bone injuries | 0.017 | ||
| Yes | 31 (53.4) | 8 (100.0) | |
| No | 27 (46.6) | 0 (0.0) | |
| Surgical operation in 7 days | 0.907 | ||
| Yes | 35 (60.3) | 5 (62.5) | |
| No | 23 (39.7) | 3 (37.5) | |
a Values are expressed as mean ± standard deviation (min-max) or No. (%).
b P-values were obtained from the exact and Pearson chi-square tests.
5. Discussion
Individual armament is an essential issue on the agenda of countries after the school massacres in different geographies of the world and the attacks made on some communities without targeting them. The data that 74% of weapons in circulation worldwide belong to civilians show that civilians have more weapons in their hands than armies. According to the studies of the Umut Foundation, which operates in individual armament in Turkey, Turkey ranks 14th among 178 countries (1).
Although GSI deaths and injuries were common in the military before the 1980s, they have become more common among the public since the 1980s due to the widespread use of firearms acquired by civilians. Therefore, the number of patients presenting to the emergency services of civil hospitals due to GSIs is gradually increasing (9). In numerous countries, the rate of GSI among children and adolescents is increasing daily. It is known that most of these injuries are unintentional or accidental in children injured or died due to GSIs (3). As a significant cause of illness and death among children and adolescents in the USA, GSIs cause excellent material and moral damage to the affected children and society (10).
The GSIs are considered one of the leading causes of high mortality and morbidity in trauma centers. It has been observed that GSIs are regarded as the second leading cause of trauma-related deaths in the pediatric population (range: 0 - 19 years) (after motor vehicle accidents) and are the cause of more than 25% of all pediatric deaths reported from trauma centers (4, 6). A study reported the overall mortality rate due to ASF as 15.1% (11). Another study showed that the mortality rate of GSIs was within the range of 12 - 16%. This mortality rate was affected by the injury site and the number of injured organs (9). According to a study by Newgard et al., although GSIs constitute only 1% of disabled children, it was observed that they were associated with more than 20% of deaths after injury (12). In another study, although GSI-related deaths constituted 22.5% of children and adolescents within the age range of 1 - 19 years, they constituted 32.2% of all injury deaths among adolescents aged 15 - 19 years (13). The present study determined the mortality rate due to GSIs in children at 12.1%.
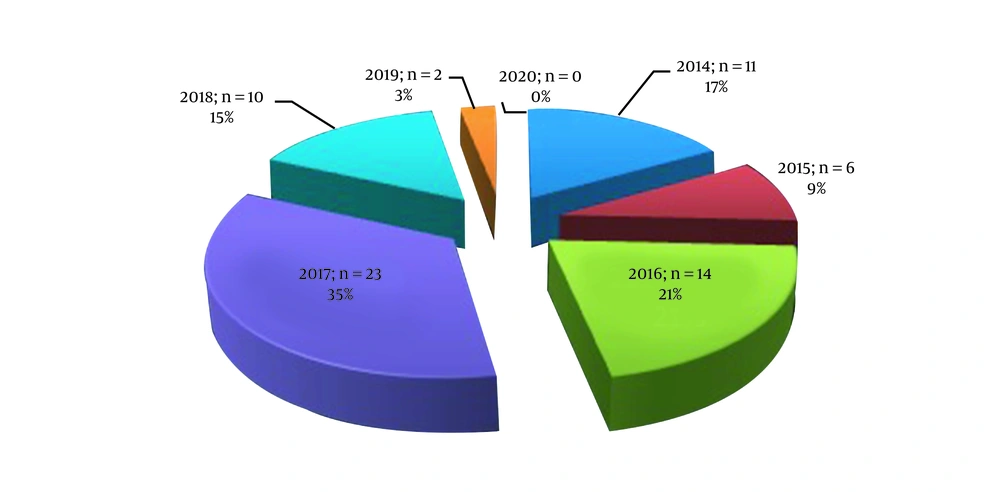
The GSIs affect the male gender disproportionately to a higher degree (82 - 86%) (11, 14). In the current study, GSIs in children were more common in males, with a rate of 81.8%, similar to other studies. In the present study, which was planned retrospectively for 7 years, no GSI case was reported in children in 2020. This might be due to the coronavirus disease 2019 pandemic, which has been ongoing since the beginning of 2020, and the restrictions and quarantine practices in place in Turkey. Figure 1 shows the distribution of GSI cases in children by year.
The head and neck area is affected in 30% of all GSI cases (15). According to another study, the head and neck (often with eye involvement) is the most frequently injured body area (16). In a study by Kaymak and Gul, it was shown that injuries were most common in the lower extremities (48%), followed by head and neck (31%) and thoracic injuries (17). Penetrating injuries constitute 5 - 20% of abdominal injuries due to firearms (17). The most common causes of peripheral vascular injuries have been identified as firearms in the USA, blunt traumas in European countries, and cutting tools in Turkey due to iatrogenic reasons (18). Unlike other studies, the present study revealed that 30.3%, 22.7%, 22.7%, 16.7%, and 7.6% of patients were injured in the abdomen, the head and neck, the thorax, the lower extremity, and the upper extremity, respectively. Simultaneously, significant vessel injuries were observed in 7.6% of the patients. Internal organ/vascular/bone injuries were observed in 39 patients (59.1%). It was observed that all patients with exitus had internal organ/vascular/bone injuries. Simultaneously, 74.4% of individuals with internal organ/vascular/bone injuries underwent a surgical operation. This result suggested that internal organ/vascular/bone injuries are considered an indicator of poor prognosis in GSIs.
Peleg et al. showed that the rate of ICU stay in GSI patients was 23% and that they had long periods of stay in the case of multiple wounds (19). In a study by Karaca et al., the rate of ICU stay was observed to be 2.8%, and the average length of ICU stay was 4 days (9). Moreover, they thought the relatively short hospital stay was due to the low rate of hospitalized patients in the ICU (9). In the current study, 78.8% of the patients (n = 52) stayed in the child trauma ICU for at least one day. The average length of ICU stay due to GSIs in children was determined at 4.34 ± 4.33 days. The mean ICU stay values were 4.91 ± 4.3 and 0.25 ± 0.5 days in discharged patients and those who died, respectively. The high rate of ICU stay is attributed to the hospital having a child trauma ICU, the shorter duration of ICU stay for those who died, and being in the severe patient group with multiple organ injuries (i.e., internal organ/bone/vascular injuries).
The GSIs in children is considered a public health crisis (20). It is known that most such injuries are unintentional or accidental in children injured or killed due to GSIs (2, 3, 20, 21). As a potential solution to this issue, it has been suggested to raise public awareness, particularly among parents, about opening a children’s rehabilitation center and the dangers of firearms (3). In another study, it was suggested that administrative regulations and prohibitions should affect the GSI problem. However, it was stated that an integrated approach should be developed in this process, and priority should be given to tackling all aspects of the problem using informative instruments that prevent incentive actions (1).
The GSIs can occur as a result of suicide in children and especially adolescents. Programs that help children and adolescents manage emotions and develop skills to solve problems in relationships, school, and with their peers can reduce adolescents’ suicidal behavior and improve their ability to seek help and cope (14). Almost 40% of parents believed their children were unaware of where weapons were stored, and 22% believed their children had never used weapons at home (20). Safe storage (i.e., unloading and locking all firearms and ammunition) is one of the most effective ways to reduce morbidity and mortality caused by GSIs (4, 6, 16, 20). The authors of the current study believe that lowering individual armament, preventing uncontrolled gun acquisition, enacting stricter security legislation, providing child and parent firearms counseling, rehabilitating citizens with violence potential, adhering to safe storage procedures, determining public health policies on armament, and treating childhood trauma of the injured in ICUs would reduce morbidity.
There are some limitations to the current study. Firstly, the study has a retrospective, single-center, and relatively small sample. Multi-center, large-scale, and prospective analyses can be arranged in this regard. Simultaneously, in the present study, the types of weapons used to injure the children and the reasons for the injury could not be determined. However, all cases originated from individual events outside the war zone. This situation shows that it is related to personal armament.
5.1. Conclusions
The GSIs are considered a preventable public health crisis. The GSIs are primarily unintentional or accidental and cause high mortality and morbidity in children. Most injuries are detected in the abdomen. The GSIs are disproportionately observed in male patients. The prognosis is worse in those with internal organ/vascular/bone injuries. These patients have higher mortality, longer hospital stay, and a higher rate of surgical operation.