1. Background
Childbirth is a significant physiological event for a woman, which has profound physical, psychological, and emotional effects on her. This phenomenon is associated with pain, stress, vulnerability, possible physical injury, and rarely death (1). The cesarean section, which involves the removal of the fetus through an incision on the abdomen and uterine wall, is one of the most common surgical procedures for women. The increasing number of cesarean sections in many countries has raised concerns among researchers and public health officials. Currently, the cesarean section prevalence in most countries is significantly different from the statistic approved by the World Health Organization (WHO), namely 10 - 15% of births (2).
Generally, it is agreed that all women with a history of a cesarean section should attempt a natural birth. Of course, vaginal birth after cesarean section is associated with potential risks and is sometimes clinically indicative of recurrent cesarean section. Clinical judgment is essential in the selection of the appropriate method of delivery. Normal delivery is prohibited in cases with natural scar cesarean, inferior vertical scar extended to the upper segment, and T-scar (3). If the selection of patients is accurate and the procedure is monitored adequately, most women who have had a cesarean section can undergo vaginal birth (4).
Cesarean section is not always necessary, and vaginal birth after cesarean section can reduce the number of recurrent cesarean sections (5). Vaginal birth after cesarean is a safe and desirable method for most women with a history of cesarean section, as suggested by the Canadian Association of Midwives and the American College of Obstetrics. Selection of this method will result in greater overall safety for the mother and baby, less risk of infection, less need for anesthesia, and shorter recovery time (6). Natural vaginal delivery is a physiological and natural process for the birth of a fetus that does not require medical intervention and does not harm the mother's health. Physiological delivery means providing the conditions leading to protecting the privacy of the mother giving birth (7). However, cesarean section, similar to other surgeries, has complications such as wound infection, pelvic infection, pulmonary infection, urinary tract infection, pulmonary embolism, anesthesia, and even maternal and neonatal morbidity and mortality (8).
Most women with previous transverse cesarean sections are candidates for experimental surgery after the previous cesarean section. Women with two previous cesarean sections, a low vertical incision, and twin pregnancies are also candidates. Those at high risk for complications such as a previous history of classic or T-shaped incision, more extensive surgery, and other conditions have a vaginal birth prohibition.
The maternal mortality rate is two times more in cesarean section than in vaginal birth. In the past, aspiration, infection, and bleeding were the most common causes of maternal mortality following surgery, but the progress of preventive techniques and measures has decreased this rate sharply. Currently, the most common cause of maternal mortality following surgery is thromboembolic events (followed by pulmonary embolism).
A study conducted by Cunningham et al. on the evaluation of normal birth after cesarean section and its effect on pregnancy outcomes in 2005 showed that if a cesarean section is repeated, the length of hospital stay (3.1 vs. 1.2 days) and complications increase following surgery. There was no case of uterine rupture, which is the most important complication after cesarean section. The results show that if patients are carefully selected for vaginal delivery and necessary care is performed during birth, a normal birth after cesarean section can be a low-risk method [cited in (9)].
Haumonté et al. study on the causes of uterine rupture following vaginal delivery after a cesarean section indicated that the success rate of normal delivery after cesarean section is 75%. Therefore, natural vaginal birth following a cesarean section can be used to reduce unnecessary cesarean sections [cited in (10)].
2. Methods
In the present descriptive-analytical study, all hospital records of women hospitalized in Ali Ibn Abi Talib hospital's obstetrics and gynecology ward in 2016 and 2017 were studied. The total number of cases studied in this period was 176 hospital records. The inclusion criterion was a history of cesarean section delivery, followed by natural vaginal birth. A data collection tool was used to abstract the hospital records of patients using pre-designed forms. Sampling was done using a simple and convenient method. In this study, all hospital records of patients from 2016 to 2017 were analyzed. Descriptive statistics were used to describe the data, including tables, diagrams, and percentages. Data were analyzed by SPSS 22 software, and the significance level was set at 0.05.
3. Results
We studied 176 cases that met the inclusion criteria. The mean age of the studied women was 29.30 ± 6.70 years. The mean gestational age was 37.64 ± 3.13 weeks. The mean number of pregnancies in the study population was 4.52 ± 2.19. The mean neonatal Apgar score was 9.56 ± 1.42, and the mean neonatal weight of the neonates was 3,076.07 ± 590.62 g.
In this study, 48 (27.3%) people were literate, and 128 (72.7%) were illiterate. Also, 106 (60.2%) neonates were male, and 70 (39.8%) were female. The successful birth rate was 92% (162 cases), and the unsuccessful birth rate was 8% (14 cases).
3.1. Objective 1: Determining Maternal Complications of Vaginal Birth After One Cesarean Section
In this study, four patients needed blood transfusion (2.3%), three people had cervical rupture (1.7%), three cases (1.7%) of neonatal death were observed, and one case (0.6%) of uterine rupture was reported (Table 1).
| Complications | No. (%) |
|---|---|
| Uterine rupture | 1 (0.6) |
| Blood transfusion | 4 (2.3) |
| Infant death | 3 (1.7) |
| Cervical rupture | 3 (1.7) |
| All uncomplicated cases | 165 (93.7) |
| Total | 176 (100) |
Frequency of Complications of Vaginal Birth After One Cesarean Section in Participants
3.2. Objective 2: Determining the Relationship Between Maternal Age and Success Rate and Complications of Vaginal Birth After One Cesarean Section
There was no significant relationship between maternal age and success rate (P = 0.98). There was no significant relationship between the complications of vaginal birth after one cesarean section and maternal age (P = 0.569).
3.3. Objective 3: Determining the Relationship Between the Number of Normal Vaginal Deliveries (Before or After one Cesarean Section) and the Success Rate of Vaginal Birth After One Cesarean Section
There was no significant relationship between the number of vaginal births and the success rate of vaginal birth after one cesarean section (P = 0.83).
3.4. Objective 4: Determining the Relationship Between the Number of Normal Vaginal Deliveries (Before or After One Cesarean Section) and Complications of Vaginal Birth After One Cesarean Section
There was no significant relationship between the number of normal vaginal deliveries and complications of vaginal birth after one cesarean section (P = 0.0).
3.5. Objective 5: Determining the Relationship Between Neonatal Apgar and the Success Rate of Vaginal Birth After One Cesarean Section
No significant relationship was observed between neonatal Apgar and the success rate of vaginal delivery after one cesarean section (P < 0.001).
3.6. Objective 6: Determining the Relationship Between Neonatal Apgar and Maternal Complications After Vaginal Birth
The mean Apgar score in patients with complications was 9.78 ± 0.69, while it was 6.27 ± 3.84 in patients without complications, showing a statistically significant difference (P < 0.001).
There was no significant relationship between gender and the success rate of vaginal birth. As seen, 4.7% of male infants and 12.9% of female infants were successful, while 95.3% of male infants and 87.1% of female infants were unsuccessful; the difference between them was insignificant (P = 0.051).
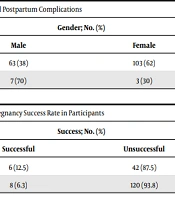
There was a significant relationship between the gender of neonates and maternal complications after birth. The results are shown in Table 2 as percentages by infant gender. The percentage of complications was higher in female infants than in males, which was statistically significant (P = 0.044) (Table 2).
| Complications | Gender; No. (%) | P-Value (Pearson Chi-Square) | |
|---|---|---|---|
| Male | Female | ||
| Yes | 63 (38) | 103 (62) | 0.044 |
| No | 7 (70) | 3 (30) | |
Relationship Between the Gender of Neonates and Postpartum Complications
There was no significant relationship between maternal education and childbirth success. The results showed no significant relationship between the two variables, maternal education and childbirth success (P = 0.17) (Table 3).
| Literacy | Success; No. (%) | P-Value (Pearson Chi-Square) | |
|---|---|---|---|
| Successful | Unsuccessful | ||
| Literate | 6 (12.5) | 42 (87.5) | 0.17 |
| Illiterate | 8 (6.3) | 120 (93.8) | |
Relationship Between Maternal Education and Pregnancy Success Rate in Participants
4. Discussion
In the present study, the success rate of vaginal birth after one cesarean section was 92% (162 patients), and the failure rate was 8% (14 patients). The success rate of post-cesarean normal birth in selective patients is approximately 60% to 80%. one study reported the success rate of natural childbirth after one cesarean section to be 61%. Meanwhile, in a study on post-cesarean vaginal births, Bengal et al. showed that the success rate of post-cesarean normal delivery was 85%, and the failure rate was 15% (11, 12). If there is a successful birth after cesarean section, complications such as the length of hospital stay, maternal fever, and recurrent cesarean section will be reduced (13). The prevalence of vaginal birth after a cesarean section has varied in different studies, but the most critical point is the high success rate observed in our study. Considering the high number of pregnancies observed in our study, perhaps one of the most critical factors affecting the success rate is the number of pregnancies.
In the present study, the complications of vaginal birth after cesarean section were blood transfusion (n = 4, 2.3%), cervical rupture (1.7%), neonatal death (1.7%), and uterine rupture (6%) (observed in one person). In a comprehensive study, the risk of uterine rupture following VBAC was reported to be 0.3% (14, 15). In this study, the risk of blood transfusion was reported in the range of 0.2% to 1.2%, but the most critical point is that these studies did not use similar definitions for the diagnosis of bleeding and the number of blood products used, which can justify the different results (14). As can be seen, the side effects observed in all studies show a low rate, but little difference is observed. This difference is mainly due to the type of cesarean section in different locations and the use of misoprostol and other drugs, as well as different definitions for bleeding and blood reception. The most crucial factor that needs to be further studied is the high rate of neonatal mortality in this study compared to other studies.
In this study, age, sex, neonatal Apgar score, and other components were studied in the study groups, none showing a significant relationship. Similar articles also studied these components between cesarean section and the normal birth after cesarean section, and all differences were insignificant.
In the present study, the success rate of vaginal birth after one cesarean section was 92% (162 people), and the failure rate was 8% (14 people). Complications included blood transfusion (2.3%), cervical rupture (1.7%), infant mortality (1.7%), and uterine rupture (6%).