1. Background
Coronavirus disease (COVID-19), which originated in late December 2019 in Wuhan, located in the Hubei province of central China, rapidly spread worldwide (1). There is solid evidence that peoples’ lifestyles were dramatically affected by the lockdown, with a high potential risk of sedentary behaviors, harmful eating habits, and psychological distress (2, 3). At the same time, athletes were not exempted from the pandemic-control measures and faced limitations for training, competing, or participating in international competitions (4). Many athletes preparing for the Olympic Games in Tokyo, due to the COVID-19 home confinement, had to continue their training sessions on their own, naturally in basic environments with limited resources. Consequently, elite athletes were seriously exposed to some levels of unpreparedness because of the COVID-19 pandemic, which seriously adversely affected their physical and physiological performance and had a negative impact on their sports performance (5).
Physical activity is essential in a healthy lifestyle and immensely correlates with mental health (mood state, anxiety, and health-related quality of life) (6-11). However, although a strong correlation has been observed between mood and physical activity, this is highly dependent on the intensity and duration of the exercise (12).
In the COVID-19 pandemic, resilience is frequently referred to as a significant determinant of mental health when confronting such problems. Evidence supports the hypothesis that athletes can be more resilient than non-athletes (13, 14). Considering this, it could be stated that athletes may have better mental health in stressful situations than non-athletes, and this can be strengthened in challenging situations. Numerous studies have examined the psychological resilience of elite athletes; however, no study has been conducted in this regard during the COVID-19 pandemic. Therefore, further studies on this topic are needed.
Moderate-intensity physical activity increases the levels of stress hormones and reduces inflammation, and improved immunity to viral infections through cellular response changes. 20 - 30% reduced infection in the upper respiratory tract in people with moderate physical activity levels was observed (15). However, long-term high-intensity physical activity compromises the immune system for several hours after exercise and increases the risk of respiratory tract infection during this period (16). These factors may significantly affect a person's mood, eating habits, and physical activity. On the other hand, the interaction between nutrition and the immune system is well known; therefore, any nutritional imbalance can affect the competence and integrity of the physical performance, mood, and immune system. Healthy nutrition and lifestyle are among the most critical measures in maintaining health and preventing infectious diseases. Research has demonstrated that one of the main strategies to strengthen the immune system and to avoid disease is to consume adequate calories and high-quality proteins (17). Eating disorders can have devastating effects on both the health and performance of athletes (18, 19).
2. Objectives
Due to the obscure nature of the COVID-19 pandemic, different sectors of the society, including athletes and non-athletes, were confined in quarantine, which caused changes in their lifestyle and affected their physical and mental health, as well as other aspects of their lives, such as eating habits, mood, and level of physical activity. The question is whether or not athletes who are likely to have a higher level of physical activity than non-athletes had more healthy eating habits and better moods during the COVID-19 pandemic compared with non-athletes, and whether COVID-19 home confinement had similar effects on athletes and non-athletes.
3. Methods
3.1. Study Design
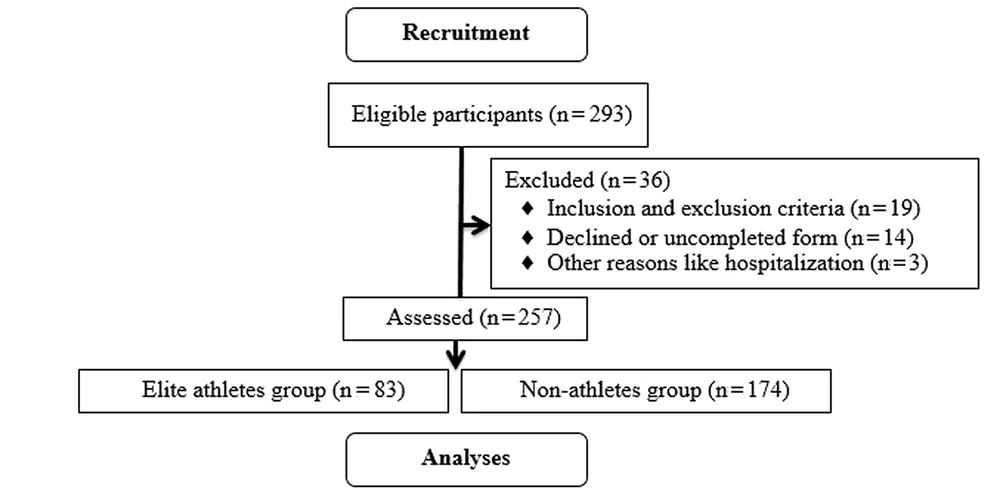
This cross-sectional multicenter study was conducted through an online survey between March 22 and May 4, 2020. This period was the early phase of the COVID-19 outbreak in Iran when the Iranian government declared a national quarantine. In addition, at that time, all sports facilities and clubs were closed, and all sporting events were canceled. Participants were clustered from all five regions of the country (north, south, west, east, and center) affected by the widespread pandemic. The eligible participants ranged from 20 to 40 years old, and both athletes and non-athletes lived in Iran. The criterion for the elite athlete was competition at the Super League and national and international levels in the team and individual sports. The recruitment process flow chart is shown in Figure 1.
3.2. Participants and Data Collection
In this descriptive cross-sectional and comparative study, a total of 257 elite athletes (n = 82, male = 38%, female = 62%) and non-athletes (n = 175, male = 44%, female = 56%) [Age: 29.95 ± 9.1 y; BMI: 23.8 ± 3.6 kg/m2] participated voluntarily. A total of 293 questionnaires were received (response rate: 87.7%), with 257 having completed and provided valid demographic information, IPAQ/eating attitudes, and mood state. No statistical method was used to predetermine the sample size, and as many participants as possible were included voluntarily during the early phase of the outbreak in Iran. The study was conducted through a web-based questionnaire inquiring about demographic information (ie, age, gender, town or village of residence, current employment); anthropometric data (weight, height, and BMI); dietary habits; physical activity levels; mood states. Inclusion criteria included Iranians aging from 20 to 40 years, athletes and non-athletes were included, and all participated in the survey without any restrictions. Exclusion criteria included incomplete questionnaires. On the first page of the online survey, participants were briefed about the study’s aims, its anonymous data collection, the confidentiality of data handling, and the study’s ethical approval. Subsequently, the participants ticked a box for their consent. The questionnaire was designed at porsline.ir. The questionnaires were distributed amongst the participants through social networks (WhatsApp, Telegram, Instagram, and E-mail) for two weeks. The participants were required to complete the Persian version of the physical activity (20), mood (21), and nutrition (22) questionnaires were asked for one week before completing the questionnaire. The validity and reliability of the Persian version of these questionnaires were reported as acceptable.
Eating disorder symptoms and physical activity levels were evaluated using the Eating Attitudes Test-26 (EAT-26) and the International Physical Activity Questionnaire short form (IPAQ-SF), respectively. Brunel Mood Scale (BRUMS) was used to evaluate the mood status of the participants. The International Physical Activity Questionnaire (IPAQ-SF), which consists of 7 questions, was used to measure the levels of physical activity. The validity and reliability of the IPAQ questionnaire were confirmed in other studies (2, 20). Physical activity data were obtained from IPAQ-SF for metabolic equivalent (MET) - minutes per week, calculated as MET intensity multiplied per minute for each activity over seven days (23, 24).
The Eating Attitudes Test (EAT-26; Garner et al., (25)) is the most widely used measure of anorexia nervosa, bulimia nervosa, and binge eating disorder. EAT-26 is a 26-item self-report questionnaire that is presented on a 6-point forced-choice Likert scale ranging from 0 (“never,” “rarely,” and “sometimes”) to 3 (“always”). Item 26 is scored in reverse: from 3 (“always,” “usually,” and “often”) to 3 (“ever”). The total score (between 0 and 78) provides an overall risk score, where higher scores indicate a greater risk of an eating disorder. Full scores 20 or above are considered to be in the clinical range. The reliability of the Persian form of the EAT-26 using Cronbach’s alpha coefficient was acceptable in the range of 0.69 to 0.73 (22).
BRUMS was used to measure positive and negative mood states. BRUMS is a 24-item self-report questionnaire that is presented on a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”); higher scores reflect a more negativé mood state. BRUMS has six subscales (ie, tension, depression, anger, vigor, fatigue, and confusion) of four items, each with total possible subscale scores ranging from 0–16. The internal consistency values (Cronbach’s alpha) of all dimensions and the total scale ranged from 0.74 to 0.90 (21), while in the present study, the total scale was 0.81.
3.3. Statistical Methods
The statistical analysis was performed using the SPSS v21.0 (SPSS Inc., Chicago, IL, USA). Data were presented as mean ± SD and mean rank in the tables and the text. The Kolmogorov-Smirnov (KS) was used to determine if a sample comes from a population with a specific distribution. To analyze the differences between social characteristics of athletes and non-athlete, we used independent models t-test and chi-square test. The U Mann-Whitney test was used to compare the differences between the two separate groups for the research variables. The significance was set at P ≤ 0.05.
3.4. Ethical Approval
The research was approved by the local ethics committee of Imam Khomeini International University (ref. no. 17628), and was performed in compliance with the seventh and current revision (World Medical Association, 2014) of the Declaration of Helsinki. This web-based questionnaire was non-commercial, and participation was completely voluntary.
4. Results
KS test was used to determine the normality of data distribution. The results indicated that the research variables had no normal distribution (P < 0.05), so non-parametric methods were applied. The characteristics of the participant’s Socio-demographic are shown in Table 1.
| Variables | Athlete | Non-athlete | Total | P-value |
|---|---|---|---|---|
| Number | 82 (31.9) | 175 (68.1) | 257 (100) | |
| Gender | ||||
| Male | 31 (38) | 77 (44) | 108 (42) | < 0.001 |
| Female | 51 (62) | 98 (56) | 149 (58) | < 0.001 |
| Age (y) | 28.9 | 30.5 | - | 0.460 |
| Height (cm) | 167.4 | 166.2 | - | 0.651 |
| Weight (kg) | 64.2 | 67.5 | - | 0.345 |
| BMI (kg/m2) | 22.9 | 24.3 | - | 0.210 |
| Occupation | < 0.001 | |||
| Employed | 59 (72) | 129 (74) | 188 (73) | |
| Not employed | 23 (28) | 46 (26) | 69 (27) | |
| Education | < 0.001 | |||
| Holding a university degree | 21 (26) | 51 (29) | 72 (28) | |
| Not holding a university degree | 61 (74) | 124 (71) | 185 (72) | |
| Smoker | < 0.001 | |||
| No | 59 (71) | 94 (54) | 153 (60) | |
| Yes | 23 (29) | 81 (46) | 104 (40) | |
| Marital status | < 0.001 | |||
| Married or having a partner | 58 (71) | 101 (58) | 159 (62) | |
| Not married or no partner | 24 (29) | 74 (42) | 98 (38) | |
| Economic state | < 0.001 | |||
| Dependent | 43 (52) | 94 (53) | 137 (53.3) | |
| Independent | 39 (48) | 81 (46) | 120 (46.7) | |
| History of COVID-19 | < 0.001 | |||
| No | 74 (90) | 149 (95) | 223 (87) | |
| Yes | 8 (9) | 26 (15) | 34 (13) |
a Values are expressed as No. (%).
As seen in Table 2, the Mann-Whitney test indicated that the physical activity level was higher in the athletes (median = 3884) in comparison with the non-athletes (median = 808.5), U = 3826.5, P < 0.001. There was no significant differences between mood of the athletes (median = 46) and non-athletes (median = 47) groups (U = 6975, P = 0.719). Eating habits were healthier in athletes (median = 11.5) than in non-athlete (median = 10), U = 6088.5, P = 0.049; the non-athletes had healthier dietary habits than the athletes.
| Variables | Mean ± SD | No. | Mean Rank | Sum of Ranks | U-Man Whitney | Z-Score | P-Value |
|---|---|---|---|---|---|---|---|
| Physical activity | 3826.5 | -6.04 | < 0.001 a | ||||
| Athlete | 5917.5 ± 7885.6 | 82 | 169.8 | 13926.5 | |||
| Non-athlete | 2316.1 ± 4509.5 | 175 | 109.9 | 19226.5 | |||
| Mood | 6975 | -0.36 | 0.719 | ||||
| Athlete | 49.4 ± 10.3 | 82 | 126.6 | 10378 | |||
| Non-athlete | 48.9 ± 9.1 | 175 | 130.1 | 22775 | |||
| Eating habits | 6088.5 | -1.96 | 0.049 a | ||||
| Athlete | 14.3 ± 10.5 | 82 | 142.3 | 11664.5 | |||
| Non-athlete | 11.6 ± 8.7 | 175 | 122.8 | 21488.8 |
a Significant difference (P < 0.05)
5. Discussion
In the current study, the athletes had higher physical activity levels than non-athletes during the COVID-19 pandemic; nonetheless, they developed poor and unhealthier habits than non-athletes. It was also demonstrated that the athlete's mood was not different from that of non-athletes under lock-down conditions. In this regard, we assumed that the athletes had higher levels of physical activity than non-athletes during the pandemic, which could justify the significant difference in the mood of the two groups. However, the study findings did not confirm this, as no considerable mood differences were found between the two groups. Confinement strategies were associated with a higher incidence of mental disorders during the first peek of the pandemic. Although increased mental distress has been found tremendously among people during the pandemic, it was inevitable to control the pandemic. Meanwhile, the confinement seriously affected the elite athletes preparing for the 2020 Olympic Games in Japan. The beneficial effects of regular exercises on mental health have been well-documented based on psychological theories such as self-efficacy and social interaction (12).
On the other hand, the pandemic had a great role in the intensification of the symptoms of depression, anxiety, and stress (26). Exercise can't cure severe mental disorders (27). In their study, Batalla-Gavalda et al. reported that home confinement negatively affected the moods of young athletes (28). Moreover, Leguizamo et al. observed that the harmful effects of the COVID-19 lockdown were similar to those of the recovery period after a sports injury. According to the literature, adverse mood states and emotional distresses may appear after a sports injury due to the injury itself and the ensuing rehabilitation processes (29). There is evidence that physical activity levels can influence mood states. Chekroud et al. observed a negative relationship between exercise intensity and exercise volumes and stress, depression, mood, and emotional distress in American adults (30). Numerous studies have revealed a negative relationship between anabolic hormone levels and mood, showing that a decrease in the levels of anabolic hormones can adversely influence mood. When the exercise intensity is excessive, an anabolic process develops, and negative mood symptoms are intensified. When the exercise pressure is moderate, a catabolic state develops, which is directly related to mood fluctuations (26, 29, 31).
As discussed, the athletes showed higher levels of intense physical activity compared to the non-athletes. Izzicupo et al. observed that athlete students had higher levels of high-intensity physical activity compared to their non-athlete counterparts, which is consistent with our findings. This could be attributed to the commitment and perseverance of the elite athletes, which allowed them to continue training even in confinement, and psychological and physical constraints did not lead to temporary cessation or termination of the regular workout (32). Research has shown that people who exercise high-intensity physical activity were less likely to have lower levels of physical activity during the COVID-19 lockdown than those with moderate or low-intensity physical activity. Many elite athletes pursue sports professionally, and even confinement of such restrictions try to follow their professional and career processes (4, 32). Research findings have shown that the psychological state plays a crucial role in several daily habits, mainly eating patterns (33). Findings of a study demonstrated that athletes experienced more disordered eating habits than non-athletes during the COVID-19 lockdown. Several studies have reported that moderate physical activity and healthy eating patterns are correlated with positive mood states and overall participants' health (34-36).
In this study, it was found that during the COVID-19 confinement, athletes adopted more objectionable and unhealthy habits than non-athletes. The COVID-19 home confinement also negatively impacted the quality of the physical activity. Additionally, it was observed that daily sitting time was increased from 5 to 8 hours per day, and food consumption and daily meal patterns (food types, uncontrollable eating bouts, snacks, and the number of meals) were unhealthier during confinement. Unhealthy eating during the quarantine can be attributed to anxiety and mood changes (33). Under normal circumstances and before the pandemic, athletes endeavored to seek more social support when faced with stressful situations. Unfortunately, this was impossible during the pandemic due to the social restrictions. Most coping strategies were affected during the pandemic, and it seems that coping strategies would involve symptoms of eating disorders for many individuals (37). In this regard, athletes seem to face losing control over their eating behavior, which leads to different psychological consequences (such as guilt feeling, stress, and mood changes).
One limitation of the current study was the lower number of athletes compared to non-athletes, which made the comparison difficult. Moreover, accurate calculation of the exercise intensity and volume and the amount of consumed energy was not possible due to the online quality of the survey. Future studies should aim to recruit more participants and define the precise type and intensity of the training. Another limitation was the low levels of awareness of the participants about different mental states, which should be considered in future studies. Besides, one of the other limitations of the research was that the investigation had a cross-sectional design; if the design was longitudinal, more accurate results could be obtained. Moreover, it was better to consider the differences between gender, age, individual and team sports, and the competitiveness of the field should have been taken into account for better illumination of the consequences of the quarantine.
5.1. Conclusions
The findings of the present study demonstrated athletes had higher levels of physical activity during the pandemic compared to their fellow non-athletes, but this had no favorable effects on their moods. At the same time, non-athletes adopted healthier dietary habits than non-athletes. Given the complex psychosocial consequences of COVID-19 confinement, it appears that the sport authorities and trainers should consider the mental and nutritional health of elite athletes.