1. Background
Coronary artery disease (CAD) is symbolized by advancing occlusive atherosclerosis, acute plaque rupture, and atherothrombosis (1). Atherothrombosis is an acute coronary syndrome (ACS) involving one or more chest pain events resulting from acute myocardial ischemia (2). The pain usually lasts for more than ten minutes (2). The World Health Organization states that CAD will be a major cause of mortality globally by 2030 (3).
Approximately 15.4 million Americans over 20 years old had CAD, with a prevalence of 6.4% (4). According to the annual report of national cardiovascular disease (NCVD)-ACS registry 2014 - 2015, a total of 17,771 ACS patients were identified in Malaysia with 8,190 were STEMI (46.1 %), 4,479 NSTEMI (25.2 %) and 5,102 unstable anginas (28.7 %).
Being hospitalized due to an ACS event becomes a highly stressful experience and is mostly linked with the long-term risk of unfavorable cardiac outcomes among ACS patients (5). Besides, sleeping difficulties, fear of the unknown, feeling out of control, noise, scarcity of information regarding ACS, and the newness of hospital surroundings also increase the chances of high levels of stress (6). Besides recovering from their illness, ACS patients recover from the extra burden of psychologically and physiologically stressful hospitalization experiences during hospital discharge (7).
Additionally, various life stressors such as socio-economic, financial, marital, and work stress can also result in chronic stress states (8). Continued stress at work or home was reported to lead to the onset of the disease and linked with a higher incidence of myocardial infarction (8).
The current study was conducted to identify the associated factors of stress among ACS patients. This article is derived from a study by Wan-Nor-Asyikeen et al., a part of which was previously published (9). However, both studies identified different outcomes, whereas the previous study was published on anxiety-related factors among ACS patients.
Various research on this issue has been conducted in developed countries; however, limited studies in Malaysia have been published. Determining the associated factors of stress among ACS patients can modify those factors through environmental or behavioral changes and thus can avert the occurrence of stress.
2. Objectives
The current study was designed to determine the associated factors of stress among ACS patients. Through understanding these factors, appropriate interventions, and preventative strategies could be formulated to support individuals and groups at higher risk of developing stress.
3. Methods
3.1. Study Design
The current study involved a cross-sectional study conducted in two selected hospitals in Kelantan and Terengganu, Malaysia (9). All ACS patients admitted to the medical wards, including general wards, cardiac rehabilitation ward (CRW), and coronary care unit (CCU) in both hospitals participated in the study (9).
Human Research Ethics Committee of University Sains Malaysia and the Medical Research & Ethics Committee (MREC), Ministry of Health (reference number: NMRR-13-1469-1886) approved the study on 4th August 2014 and 10th July 2014, respectively. Consent was obtained from the Hospital Directors of both hospitals.
3.2. Participants
The study included patients aged above 18 years old, can read, speak and understand the Malay language and were obtained informed consent. Those patients with any altered mental status, had psychological problems, were intubated, and mentally retarded patients were excluded from the study.
Power and sample size calculation (PS) software was used to identify the sample size. Single and two-proportion formulas were used with α of 0.05 and a power of 0.8. Those p0 and p1 were based on previous studies. According to the calculation, the sample size was 400 patients, with a 10% drop-out rate. Therefore, 200 questionnaires were distributed to ACS patients at each hospital using a convenient sampling method.
3.3. Data Collection
The questionnaire consists of two parts. The first part was designed to provide details on socio-demographic profiles such as age, gender, ethnicity, marital status, occupation, education level, and co-morbidities. The second part evaluated the stress level using the Depression, Anxiety, and Stress Scale 21 (DASS-21).
The stress scale in DASS-21 measured the difficulty of relaxing, nervous arousal, easily upset or agitated, irritable or over-reactive, and impatient. Acute coronary syndrome patients were required to answer every question between 0 (which did not apply to me at all) and 3 (which applied to me very much). The score was determined by adding the scores for the relevant items and multiplying them by 2. Then, the score was divided into their category. Normal stress scored between 0 and 14; mild stress scored between 15 and 18; moderate stress scored between 19 and 25; severe stress scored between 26 and 33; and extremely severe stress scored above 34. However, the current study classified into two categories which were normal and abnormal. Normal includes normal only, while abnormal includes mild, moderate, severe, and extremely severe.
The content validity of DASS-21 has been completed by Musa et al. (10). They translated, validated, and measured the psychometric properties of DASS-21 in the Malay version. The reliability coefficient (Cronbach's alpha) of stress was 0.79 (10).
The questionnaire was distributed to ACS patients and given by hand during ward admission. The patients were explained thoroughly about the research and asked for their consent before the answering session. Then, they were given about 10 to 15 minutes to answer all the questions. The researcher explained to the patients to consider the questions after the ACS event, not prior to the ACS event. The complete questionnaire was returned to the researcher by hand.
3.4. Statistical Analysis
Statistical package for social sciences (SPSS) software version 22.0 for Windows (11) was used to enter and analyze the data collected. For continuous variables, mean with standard deviation (SD) and median with interquartile range (IQR) were used, depending upon the normality of the distribution. Frequency (n) and percentage (%) were used for categorical variables. Simple and multiple logistic regression was used to determine the associated factors of stress among ACS patients. Results were presented as the crude odds ratio (OR) for simple logistic regression, adjusted OR for multiple logistic regression, 95% confidence interval (CI), and P-value. The P < 0.05 was considered statistical significance.
4. Results
4.1. Prevalence of Stress
The results showed that out of 400 respondents, 234 (58.5%) were considered to have positive screening for stress. Of these, 68 (29.2%) had mild stress, 97 (41.6%) had moderate stress, 61 (26.2%) had severe stress, and 7 (3.0%) had extremely severe stress based on the DASS-21.
4.2. Socio-demographic Profile of Stress-ACS Patient
Table 1 shows the socio-demographic profile among ACS patients with stress. The mean (SD) age of patients with stress was 60.6 (10.7) years. Among them, a higher percentage of males (60.1%), Malay ethnicity (59.1%), and married patients (56.9%) were found to have possible stress.
| Variables | Stress, No. (%) | P-Value a | |
|---|---|---|---|
| Normal | Abnormal | ||
| Gender | 0.412 | ||
| Female | 67 (44.1) | 85 (55.9) | |
| Male | 99 (39.9) | 149 (60.1) | |
| Race | 0.757 | ||
| Malay | 133 (40.9) | 192 (59.1) | |
| Non-Malay | 33 (44.0) | 42 (56.0) | |
| Marital status | 0.619 | ||
| Single/divorced | 47 (37.9) | 77 (62.1) | |
| Married | 119 (43.1) | 157 (56.9) | |
| Occupation | 0.350 | ||
| Unemployed | 62 (44.0) | 79 (56.0) | |
| Government/private | 41 (39.8) | 62 (60.2) | |
| Others | 63 (40.4) | 93 (59.6) | |
| Comorbid | |||
| Diabetes mellitus | 100 (41.3) | 142 (58.7) | 0.929 |
| Hypertension | 124 (41.3) | 176 (58.7) | 0.907 |
| Hyperlipidemia | 76 (40.6) | 111 (59.4) | 0.744 |
| Stroke | 34 (48.6) | 36 (51.4) | 0.186 |
| Ischemic heart disease | 58 (33.9) | 113 (66.1) | 0.008 |
a Chi-square test.
Among those ACS patients experiencing stress, 66.1% had ischemic heart diseases, 59.4% had hyperlipidaemia, 58.7% had hypertension and diabetes mellitus, and 51.4% had a stroke. Patients with other comorbidities, including chronic kidney disease, gastritis, peptic ulcer, and chronic lung disease, were 64.0%.
4.3. Factors Associated with Stress
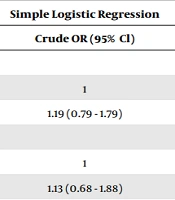
In simple logistic regression, ACS patients who worked in governmental sector (crude OR: 1.57; 95% CI: 0.79, 3.12; P = 0.198), had comorbid of stroke (crude OR: 0.71; 95% CI: 0.42, 1.19; P = 0.187), ischemic heart disease (crude OR: 1.73; 95% CI: 1.16, 2.62; P = 0.008), and others (crude OR: 1.34; 95% CI: 0.82, 2.19; P = 0.248), were the factors associated with stress as in (Table 2). Acute coronary syndrome patients with comorbid of ischemic heart disease were a strong and independent factor associated with stress (adjusted OR: 1.73, 95% CI: 1.14, 2.63, P = 0.010) as in Table 3.
| Variables | Simple Logistic Regression | ||
|---|---|---|---|
| b | Crude OR (95% Cl) | P-Value | |
| Gender | |||
| Male | 0 | 1 | - |
| Female | 0.17 | 1.19 (0.79 - 1.79) | 0.413 |
| Race | |||
| Non-Malay | 0 | 1 | - |
| Malay | 0.13 | 1.13 (0.68 - 1.88) | 0.626 |
| Marital status | |||
| Single | 0 | 1 | - |
| Married | -0.19 | 0.83 (0.26 - 2.59) | 0.741 |
| Divorce/Widow | 0.03 | 1.03 (0.32 - 3.35) | 0.965 |
| Occupation | |||
| Unemployed | 0 | 1 | - |
| Freelance | 0.26 | 1.30 (0.80 - 2.11) | 0.294 |
| Government | 0.45 | 1.57 (0.79 - 3.12) | 0.198 a |
| Private | -0.06 | 0.94 (0.50 - 1.76) | 0.851 |
| Others | -3.96 | 0.67 (0.29 - 1.56) | 0.355 |
| Level of education | |||
| Non | 0 | 1 | - |
| Primary | -0.002 | 0.10 (0.52 - 1.91) | 0.996 |
| Secondary | -0.31 | 0.73 (0.38 - 1.40) | 0.349 |
| Tertiary | -0.04 | 0.96 (0.48 - 1.93) | 0.917 |
| Household income | |||
| Low | 0 | 1 | - |
| Middle | 0.14 | 1.15 (0.75 - 1.75) | 0.503 |
| High | -0.003 | 0.10 (0.51 - 1.95) | 0.993 |
| Comorbid | |||
| Diabetes mellitus | 0.02 | 1.09 (0.68 - 1.53) | 0.929 |
| Hypertension | 0.03 | 1.03 (0.61 - 1.63) | 0.907 |
| Hyperlipidemia | 0.07 | 1.07 (0.72 - 1.59) | 0.744 |
| Stroke | -0.35 | 0.71 (0.42 - 1.19) | 0.187 a |
| IHD | 0.55 | 1.73 (1.16 - 2.62) | 0.008 a |
| Others | 0.29 | 1.34 (0.82 - 2.19) | 0.248 a |
Abbreviations: OR, odds ratio; CI, confidence interval.
a P < 0.25.
| Variables | Multiple Logistic Regression | ||
|---|---|---|---|
| b | Adjusted OR (95% Cl) | P-Value | |
| Ischemic heart disease | |||
| No | 0 | 1 | - |
| Yes | 0.55 | 1.73 (1.14 - 2.63) | 0.010 |
Abbreviations: OR, odds ratio; CI, confidence interval.
a Backward and forward LR variable selections were applied. No need for Multicollinearity and interaction checking. Hosmer Lemeshow test P-value 0.190 (models were fit). Overall correctly classified percentage = 58.5% and area under the ROC curve 60.6%.
5. Discussion
This study involved ACS patients admitted to only two selected hospitals. These hospitals were chosen as study locations as both are tertiary centers in the east coast region of Malaysia. Owing to the increasing number of ACS patients treated in the hospitals, it was suggested that the researcher examine and generate data concerning the prevalence of stress among ACS patients to maximize the role of cardiac rehabilitation.
The prevalence of stress among ACS patients in both hospitals was 58.5%. This is considered a high prevalence due to these psychological conditions being under-recognized or under-reported and hence untreated among the Malaysian population.
5.1. Factors Associated with Stress Among ACS Patients
Patients with comorbid of ischemic heart disease were significantly associated with stress. The results showed that patients with comorbid of ischemic heart disease were 1.73 times more likely to have stress than those who reported that they did not have comorbid of ischemic heart disease.
Among patients who already had comorbid of ischemic heart disease, stress-related mechanisms triggered the occurrence of cardiac events (12). The common pathology in cardiac events is the disturbance of the atherosclerotic plaque's fibrous cap and active inflammation and hypercoagulability, which result from multiple processes (12, 13). The physiological responses, which include a rise in the level of pro-inflammatory cytokines and adhesion molecules, could be the factors of atherosclerotic plaque deterioration and monocyte chemotaxis, the release of tissue factors, increase in blood viscosity, activation of platelets, and rises in the coagulation levels and fibrinolytic factors and in the hepatic production of fibrinogen (an acute-phase protein important in both coagulation and whole blood viscosity), systemic vasoconstriction and an increase in arterial blood-pressure levels, increases in sinus node firing rates and atrioventricular conduction velocity, thus increasing the heart rate; changes in the balance between sympathetic and parasympathetic cardiac control in favor of the former; and increases in myocardial oxygen consumption and myocardial work (14).
These physiological changes act together; for example, reduced parasympathetic activity associated with systemic inflammation and catecholamine release promotes cardiac repolarization abnormalities, while heightened hemodynamic responses are correlated with increased plasma viscosity (15, 16). These responses, in turn, stimulated the pathophysiological effects, such as electrical instability of the heart, transient myocardial ischemia, plaque disruption, and thrombus formation. Acute clinical events such as ventricular fibrillation, myocardial infarction, or stroke can occur.
A meta-analysis study by Edmondson et al. showed that the younger adult had a higher risk of developing stress after the ACS (17). A younger adult with ACS would deal with the event differently than an older adult because of their immaturity in coping mechanisms. Older adults have had more experience dealing with many stressful events, including ACS, so they tend to cope positively with the event, whereby the younger adults were otherwise. The coping ability would allow the patient to manage the stressor by enhancing the recovery rate from the stressful occurrence and reducing the experience of intense symptoms (17).
Besides, stress during hospitalization can occur due to sleep disturbance, unfamiliarity with the surrounding of the hospital, physical deconditioning, fear of the unknown, and/or weight loss both during hospitalization and in the days after discharge. Also, stress during hospitalization may boost the inflammation and risk for arrhythmia and cognitive dysfunction, leading to unfavorable outcomes.
A few noteworthy limitations have been found in the current study. First, this study was only carried out over a short period: 10 months period. A longer period and a larger geographical area, including many districts in the study location, were required to employ more patients. Besides, this study did not emphasize the presence of stress before ACS events as the exclusion criteria.
The authors recommended conducting large, multi-centered research within Malaysia to produce precise and referable data to represent Malaysian's ACS population. Besides, prospective cohort studies should be done with a long-term follow-up of the ACS patients. The psychological status of patients should be followed up again, maybe at 30 days, 3 months, or 6 months, to evaluate any persistent symptoms after hospital discharge.
Instead of using logistic regression, the authors should analyze using ordinal logistic regression due to the five categories in the DASS questionnaire, which was normal, mild, moderate, severe, and extremely severe. However, the authors cannot proceed with this ordinal logistic regression due to the small number of cases in each category. Therefore, the authors re-categorize those categories into normal and abnormal. Normal includes normal, while abnormal includes mild, moderate, severe, and severe.
5.2. Conclusions
The prevalence of stress in the study population was high and significantly associated with comorbid of ischemic heart disease. The effects of stress on health-promoting behavior play a significant role in poor cardiac outcomes. Creating awareness regarding the risk factors of stress is recommended. In addition, policies should be implemented to reduce the risk of stress among patients. Therefore, the authors suggest creating a screening tool to improve and determine the psychological status of ACS patients so that early treatment can be given. Besides, more emphasis should be given to ACS patients with the abovementioned risk factors.