1. Background
Dyspepsia is a set of gastrointestinal symptoms manifested by pain and discomfort, burning in the upper abdomen, and a feeling of satiety. In some cases, people experience nausea and weight loss (1). Dyspepsia is a common disorder in the community with a 14 - 48% prevalence. Dyspepsia is not a life-threatening disorder, but its high prevalence imposes much socio-economic pressure on individuals (2). A study by Talley et al. in 864 patients with a mean age of 44 years showed that dyspepsia could affect the quality of life, a finding that could not be justified by slowing gastric emptying (3). The Rome III Committee defines functional dyspepsia as the presence of these symptoms in the stomach and duodenum, which are not caused by organic, systemic, or metabolic disease (4, 5). About a quarter of cases of dyspepsia are caused by organic causes such as peptic ulcer, gastric malignancies, gastroesophageal reflux, NSAIDs, and colic biliary. In 75% of cases, diagnostic evaluations do not determine the underlying cause of dyspepsia, which, as mentioned, is called functional dyspepsia (6, 7).
Although the pathophysiology of this disorder is not well defined and has a complex pathophysiology, many of these patients complain of eating-related symptoms (8). Recent studies have shown that variation in dyspepsia symptoms can be due to several pathophysiological mechanisms (9). A study conducted in Iran to investigate the relationship between functional dyspepsia and personality traits showed that extraversion, openness, conscientiousness, and agreeableness were independently associated with a reduced risk of functional dyspepsia while increasing neuroticism increased the risk of functional dyspepsia (10). Another study found that personality traits in people with functional dyspepsia include introversion, neuroticism, and psychoticism. It also showed that functional dyspepsia is associated with anxiety and depression and that psychiatric interventions can help improve some symptoms of functional dyspepsia. Delayed gastric emptying may occur in 25% to 50% of patients with functional dyspepsia (11). A study also showed that patients with functional dyspepsia in Indonesia experience significant quality-of-life disorders. The study also revealed that factors such as anxiety, depression, aging, female gender, higher severity of symptoms, and low to moderate levels of education are important factors that affect the quality of life (12).
A delay in gastric emptying is associated with decreased anterior gastric motility, while the underlying cause of anterior gastric inactivity has not been identified (13). Other causes of dyspepsia include fundus movement disorders, visceral hypersensitivity, genetics, Helicobacter pylori infection, and psychosocial problems (14, 15). Psychological factors are also associated with dyspepsia. In general, functional dyspepsia has been described as a multifactorial disease that can be caused by the involvement of the intestinal nervous system (ENS), sensory afferent neurons, and the central nervous system (CNS) (4). A study of 400 patients with dyspepsia found that functional dyspepsia significantly affects individuals' emotional, physical, and mental health and leads to impaired quality of life (16). Complex neural interactions and emotional and psychological indicators have been suggested to play an effective role in developing symptoms of functional dyspepsia, so emotional stress, and psychological stimulation have been accepted as important and fundamental factors in the pathogenesis of functional dyspepsia (17, 18).
Studies have shown that the anxiety and stress levels in patients with dyspepsia are directly related to the severity of dyspepsia (19). In further studies, about 87% of patients with dyspepsia also had a psychiatric diagnosis (20). Studies have reported a higher prevalence of personality and sleep disorders in people with dyspepsia (21, 22). Previous studies have offered different explanations for the relationship between mental state and functional dyspepsia, which are classified into two groups: (1) Mental state can lead to functional dyspepsia; and (2) functional dyspepsia can affect mental state.
In the past, psychological factors were thought to trigger dyspepsia or dyspepsia as a clinical manifestation of a psychiatric disorder (23). Years later, some researchers tried to use the brain-gut axis (brain-gastrointestinal axis) to explain the relationship between psychiatric status and functional dyspepsia (24). After exposure to stress, the hypothalamic-pituitary-adrenal (HPA) axis and autonomic nervous system (ANS) are fully activated. This activation is associated with the secretion of corticotropin-releasing hormone (CRH), which explains the functioning of this axis. Some physical and psychological symptoms are associated with the activation process, including dyspepsia and other gastrointestinal disorders (17, 25).
2. Objectives
In this study, we investigated the relationship between dyspepsia and individuals' quality of life and personality traits to reduce the prevalence of dyspepsia in society by introducing appropriate strategies.
3. Methods
In this case-control study, we selected patients with dyspepsia or its symptoms using a convenience sampling method among those referred to Fajr Clinic of Mostafa Khomeini Hospital from May 2020 to September 2021. The Helsinki Declaration was observed during the study, and no costs were imposed on the patients. Considering the mean and standard deviation of the openness to experience score in the study of Faramarzi et al. (26), 50 people were calculated for each group.
Z = 1.96, α = 0.05, β = 0.2, S1 = 3.86, S2 = 4.71, µ1 = 23.90, µ2 = 26.32.
It should be noted that the participants in the study were randomly selected from patients referred to the Fajr Clinic of Mostafa Khomeini Hospital in Ilam. First, the patients' demographics, including age, gender, employment status, marital status, and level of education, were collected using a researcher-made checklist. Single evidence in Iran by Nedjat et al. produced acceptable reliability (0.55 - 0.84) and discriminant validity for the interview version of the WHOQOL-BREF (27). Then, the quality of life, including physical, mental, social, environmental, and total health, was determined using the WHOQOL-BREF questionnaire. Personality traits, including anger, extraversion, acceptance of new experiences, compliance, and conscientiousness, were recorded using the NEO-FFI-60 questionnaire. The questionnaire's validity coefficients ranged from 0.53 to 0.64, which were significant at P ≥ 0.01. Its reliability coefficients were 0.81, 0.73, 0.75, 0.79, and 0.83 by test-retest on neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness domains, respectively (28).
After conducting a clinical examination and considering the opinions of internal medicine and gastroenterology specialists, the study objectives were explained to patients with dyspeptic symptoms. A simple random method was used to select participants from those referred to the internal medicine clinic. Once the patients agreed to participate, informed consent was obtained from them.
3.1. Data Analysis
After collecting research data, the Kolmogorov-Smirnov test was used to examine the normal distribution of data. In addition, chi-square tests, linear regression, t-student, and multiple logistic regression were used for prediction. The significance level was considered 0.05. All analyses were performed using SPSS version 19 software.
4. Results
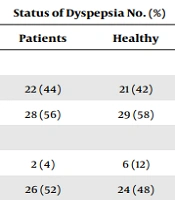
In this study, the mean age of the patients with dyspepsia was 37.42 ± 11.32 years, and the mean age of healthy individuals was 37.14 ± 12.86 years. The mean age did not significantly differ between the two groups (P = 0.809). Also, 43 men (43%) and 57 women (57%) participated in this study. There were 22 men (44%) and 28 women (56%) in the dyspepsia group and 21 men (42%) and 29 women (58%) in the healthy group. According to the chi-square test, no significant relationship was observed between gender and dyspepsia (P = 0.840) (Table 1).
| Variables | Status of Dyspepsia No. (%) | P Value | |
|---|---|---|---|
| Patients | Healthy | ||
| Gender | |||
| Men | 22 (44) | 21 (42) | |
| Women | 28 (56) | 29 (58) | 0.840 |
| Occupation | |||
| Student | 2 (4) | 6 (12) | |
| Employee | 26 (52) | 24 (48) | |
| Housewife | 5 (10) | 7 (14) | |
| Unemployed | 3 (6) | 1 (2) | 0.427 |
| Retired | 6 (12) | 5 (10) | |
| Freelance | 8 (16) | 7 (14) | |
| Marital status | |||
| Single | 20 (40) | 17 (34) | |
| Married | 30 (60) | 33 (66) | 0.534 |
| Education | |||
| Diploma | 8 (16) | 14 (28) | |
| Associate of arts | 9 (18) | 7 (14) | |
| Master's degree | 7 (14) | 8 (16) | 0.495 |
| Ph.D. | 7 (14) | 7 (14) | |
Demographic Variables in Two Groups
According to Table 1, most people with dyspepsia (52%) were employed. Also, 60% of people with dyspepsia were married, and 18% had a bachelor's degree. Finally, none of the demographic variables were statistically significant according to the chi-square test (P > 0.05).
Table 2 compares the two groups' health dimension scores and personality traits. It is concluded that the incidence of dyspepsia was higher, and this difference was statistically confirmed using an independent t-test (P = 0.000). Table 3 shows the multivariate regression analysis of personality traits and quality of life. It was found that anger affected participants' quality of life (P = 0.000, β = -0.408). On the other hand, acceptance of new experiences and conscientiousness had an effect on the quality of life (P = 0.006, β = 0.233 and P = 0.006, β = 0.269, respectively). In contrast, extraversion (P = 0.515, β = 0.068), conformity (P = 0.653, β = -0.041), gender (P = 0.499, β = 0.054), and age (P = 0.171, β = -0.114) had no effect on the quality of life.
| Variables | Disease Status | Test Value | P Value | |
|---|---|---|---|---|
| Patients | Healthy | |||
| Physical health | 56.72 ± 15.40 | 74.94 ± 12.58 | -6.48 | < 0.001 |
| Mental health | 57.17 ± 16.33 | 73.19 ± 12.53 | -5.50 | < 0.001 |
| Social health | 57.48 ± 15.06 | 70.28 ± 16.27 | -4.08 | < 0.001 |
| Environmental health | 49.38 ± 12.13 | 67.31 ± 16.29 | -6.24 | < 0.001 |
| Total health | 54.87 ± 11.83 | 73.62 ± 13.22 | -7.47 | < 0.001 |
| Anger | 37.82 ± 6.17 | 27.12 ± 8.56 | 7.17 | < 0.001 |
| Extraversion | 38.38 ± 7.88 | 44.58 ± 7.06 | -4.14 | < 0.001 |
| Acceptance of new experiences | 37.70 ± 6.36 | 41.74 ± 6.16 | -3.22 | 0.002 |
| Matching | 42.36 ± 5.65 | 45.74 ± 6.03 | -2.89 | 0.005 |
| Conscientiousness | 45.40 ± 8.68 | 49.86 ± 6.74 | -2.86 | 0.005 |
Comparison of Mean Scores of Physical, Mental, Social, Environmental, and Total Health (Quality of Life) in Study Participants According to Dyspepsia Incidence
| Variables | Non-standard Coefficients | Standard Coefficients (β) | t | P-Value | |
|---|---|---|---|---|---|
| B | Std. Error | ||||
| Anger | -0.69 | 0.18 | -0.40 | -3.85 | 0.000 |
| Extraversion | 0.13 | 0.20 | 0.06 | 0.65 | 0.51 |
| Acceptance of new experiences | 0.55 | 0.19 | 0.23 | 2.80 | 0.006 |
| Matching | -0.10 | 0.23 | -0.04 | -0.45 | 0.65 |
| Conscientiousness | 0.52 | 0.187 | 0.26 | 2.79 | 0.006 |
| Gender | 1.68 | 2.48 | 0.05 | 0.67 | 0.49 |
| Age | -0.14 | 0.10 | -0.11 | -1.37 | 0.17 |
| Constant | 41.97 | 19.69 | 0.53 | 2.13 | 0.03 |
Relationship Between Personality Traits and Quality of Life in Participants Using Multivariate Regression Analysis
Following the analysis, multiple logistic regression was performed. The results of the Omnibus test to evaluate the whole logistic regression model showed that the model's fit was acceptable and significant (P = 0.000, χ2 = 61.87) and the predictor variables were related to the criterion variable. This means that the predictor variable could significantly differentiate people with dyspepsia from people without.
The results of the Hosmer and Lemeshow test and logistic regression showed that the present model had a good fit (P = 0.891, χ2 = 0.87). Also, the study of predictor variables showed that the parent test for anger variables and low quality of life is significant (P = 0.02), but other variables included in the model were not statistically significant (R2 = 0.46) (Table 4). The results of the present study showed that the effect of anger and low quality of life on the likelihood of dyspepsia was positive and increased the odds of the disease by 3 in these people.
| Variables | Odds Ratio | Sig. | Confidence Interval 95% |
|---|---|---|---|
| Anger | 0.89 | 0.04 | 0.80 - 0.99 |
| Quality of life | 1.11 | 0.006 | 1.03 - 1.20 |
Logistic Regression Model of Predictor of Dyspepsia
5. Discussion
This study investigated the relationship between quality of life and personality traits with the incidence of dyspepsia in patients referred to Mostafa Khomeini Hospital in Ilam. This study showed that the number of women with dyspepsia was higher than that of men with dyspepsia. However, no significant relationship was observed between gender and dyspepsia, which is consistent with the results of a study conducted by Jang et al. (29). The reason may be due to racial differences, eating habits, and the prevailing customs of society.
Our study observed that most participants were employees, and the lowest number of participants were unemployed, but no significant relationship was observed between occupations and dyspepsia. It can be caused by examining people with different jobs and stress levels, aligning with the study of Nam et al. (30). It was found that working conditions and job stress are influential factors in the onset of dyspeptic symptoms.
On the other hand, according to the present study, most people with dyspepsia were married, but no significant relationship was observed between the marital status of people and dyspepsia. Chen et al. (31) observed that inappropriate marriage conditions and disputes between two people could be directly related to the occurrence and exacerbation of dyspeptic symptoms. It should be noted that based on the social conditions of our society and the way people are educated in different countries, there are huge differences that can justify this phenomenon.
It was also found that most participants had a bachelor's degree, and about 68% had a university degree. However, there was no significant relationship between the level of education and the incidence of dyspepsia, which is inconsistent with the results of a study conducted by Hantoro et al. (12). The reason for this difference could be due to the young population of the country and the psychosocial conditions prevailing in society.
Concerning the quality of life, it was found that the physical health of healthy individuals was significantly higher than that of people with dyspepsia, consistent with the results of Heidari et al. (32) and Aziz et al. (33). There are more complaints about physical disorders in people with dyspepsia. However, mental health, social health, and environmental health were significantly lower in people with dyspepsia, which indicates a decrease in quality of life in people with dyspepsia, which align with studies by Hantoro et al. (12) and Heidari et al. (32).
However, this study found that anger was higher in people with dyspepsia than in healthy people, consistent with the studies by Heidari et al. (32) and Bulut Cakmak et al. (34). In the study by Bulut Cakmak et al., (34) dyspepsia increased the level of anger in patients, aggravating the symptoms of dyspepsia. It was also found that the rates of extraversion, acceptance of new experiences, flexibility, adaptation, and conscientiousness were significantly lower in people with dyspepsia than in healthy people, consistent with studies by Sharbafchi et al. (10) and Chen et al. (31). This can be due to increased anxiety in patients with dyspepsia, increased risk of depression, and decreased self-esteem in these patients (7, 11, 12).
5.1. Limitations
Using questionnaires to collect data can be one of the limitations of the present study, as it may result in shallow results. Using qualitative research methods to identify additional primary and underlying factors that can significantly influence the prediction of patients' quality of life can enhance the depth and richness of research findings.
5.2. Conclusions
Based on the multivariate regression model, anger, acceptance of new experiences, flexibility, and conscientiousness of personality traits are effective on quality of life in people with dyspepsia. Therefore, by changing the personality traits of patients with dyspepsia and providing appropriate training, it is possible to improve people's health and living conditions and reduce the symptoms of dyspepsia.
Due to the increasing prevalence of depression and anxiety, it is suggested that future studies examine the impact of these indicators on the quality of life. In the present study, only a group of patients with dyspepsia was studied, so future studies may examine the variables studied in this study in people with IBS and abdominal migraine and compare the results with ours. It is also recommended that future studies use new indicators such as serotonin levels and education for improving personality traits and quality of life to evaluate patients with dyspepsia and treat them. In future studies, quality of life and outcomes should be evaluated before and after dyspepsia treatment.