1. Background
Worldwide, 4.5 million children die each year because of acute respiratory illnesses (1), and primary pneumonia and bronchiolitis are the most important causes of mortality and morbidity in children under 5 years of age in developing countries (2). The most important clinical signs of these infections are tachypnea and intercostal retraction, and the main involved pathogens are Streptococci, Mycoplasma, Chlamydia, and viruses including respiratory syncytial virus (RSV), influenza and rhinovirus (3-5). The seasonality of the disease hypothesized that a decrease in serum levels of vitamin D following a diminution in sunlight exposure was involved in the occurrence of infections (6, 7). Vitamin D plays a key role in activating the innate immune system, increasing mucociliary clearance, regulating epithelial cell production, and modulating inflammatory pathways (8, 9). Previous studies have suggested that vitamin D deficiency plays a role in increasing the incidence of respiratory infections, bronchitis, pneumonia, tuberculosis and even fever and neutropenia, rickets, osteomalacia, autoimmune diseases, type 1 and even type 2 diabetes, hyperproliferative skin diseases, rheumatoid arthritis, multiple sclerosis and cancer (10-12). Some studies have shown that children who take vitamin D supplements are less likely to develop a respiratory infection. Mortality rates were higher in children with pneumonia who simultaneously had vitamin D deficiency (13). However, in some studies, the serum vitamin D levels in patients with pneumonia were not significantly different from the control group (14, 15). Some of these studies had retrospective cohort designs and had a higher risk of bias. Few of these studies are conducted among Africans and Asians (16). Iran is located in the northern latitude and eastern longitude, and in these areas, between November and March, UV-B radiation is not enough to produce vitamin D (17, 18). Consequently, in some studies in Iran, the prevalence of vitamin D deficiency in children ranged between 81.3% and 37.9% (19, 20). In general, due to this issue and the boom in urbanization, sedentary and apartment living, the amount of sun exposure has decreased. We face vitamin D deficiency in children because children younger than two years take vitamin D supplements, which some mothers do not take completely. There is widespread evidence of vitamin D deficiency in low, middle, and high-income countries. Therefore, the prevalence of vitamin D deficiency among children in different areas of the world is estimated to be between 30% and 90% depending on diet, environmental conditions, and latitude (21, 22). Acute respiratory infections, the most common childhood infection, are a common reason for prescribing antibiotics that are often inappropriate, which in addition to imposing economic costs and drug side effects, has increased antibiotic resistance (23). The framework and strategy will be useful for early diagnosis of the disease and the establishment of appropriate experimental treatment to reduce the burden of disease and prevent high mortality, as well as to prescribe antibiotics more rationally to some extent (23). Vitamin D supplementation is economically feasible and practical. Therefore, supplementation reduces the deficiency of this vitamin and decreases the rate of pneumonia, improves its prognosis, and can be associated with a significant reduction in child mortality (22).
2. Objectives
This study aimed to compare the serum levels of vitamin D in children with acute febrile respiratory infection admitted to the pediatric ward of Allameh Bohlool Gonabadi Hospital as the case group and healthy children referred to the outpatient clinic of this hospital as the control group.
3. Methods
3.1. Participants and Setting
In this case-control study, 50 preschool children (2 - 5 years) in two groups of children with acute febrile respiratory infection hospitalized in Allameh Bohlool Gonabadi Hospital (Gonabad- Iran) as case group (25 participants) and healthy children referred to the outpatient clinic of the hospital for routine care (without respiratory infection) were evaluated as the control group (25 participants) in 2019. The reason for choosing the preschool age was that acute lower respiratory tract infections are the most important causes of mortality and morbidity in children under 5 years of age in developing countries (2), and we considered the minimum age to enter the study to be 2 years; because before the age of 2 years, according to the country's supplement program with vitamin D, this age group receives vitamin D supplement. The inclusion criteria for the case group included obtaining informed consent from parents of the children hospitalized in the hospital with a clinical diagnosis of acute respiratory infection, and the inclusion criteria for the control group included obtaining informed consent from parents of healthy children referred to the outpatient clinic of the hospital for routine care. Exclusion criteria were co-morbidity, using drugs that affect vitamin D metabolism (such as phenobarbital, corticosteroid, sodium valproate, etc.), vitamin D supplementation in the last 4 weeks, severe malnutrition, prematurity and history of hospitalization in neonatal intensive care unit (NICU).
3.2. Data Measurement
The data collection tool was a checklist. This checklist included a number of questions about age, sex, location, height, weight, breastfeeding status, and vaccinations. Since the data collection tool was a checklist, we did not need to check the validity and reliability, and the form was prepared using reliable sources and new articles. After taking the initial history to identify the inclusion and exclusion criteria, children were included in the study. The definitive diagnosis was made based on clinical signs and radiography by a pediatrician. In addition to standard treatment of the disease and without interfering with the treatment process, serum vitamin D levels were determined by 25(OH) vitamin D kit (Ideal Tashkhis Atieh Co. Iran) and ELISA method (Automated ELISA system, Dynex DS2, USA). The Criteria used to define vitamin D deficiency were as follows: <20 ng/mL: Vitamin D deficiency, 20 - 30 ng/mL: Vitamin D insufficiency, 30-150 ng/mL: Vitamin D sufficiency, and >150 ng/mL: Vitamin D toxicity (24).
3.3. Statistical Analysis
Data were analyzed and compared using SPSS software version 16. Descriptive statistics were used to describe the data, and analytical tests were used to analyze the data. The chi-square test was used to compare the variables, and the t-test or Mann-Whitney test was used to compare the quantitative variables of the two groups. In all tests, a significance level of 0.05 was considered.
4. Results
In this study, 50 children in the case and control groups were studied. All the parameters other than age were homogenous (P < 0.001). The mean age of the children in the case group was lower than the children in the control group. Height in the case group was lower than the control group, and the two groups were not significantly different in terms of height variable (P = 0.14). Furthermore, the weight in the case group was lower than the control group, and the difference was significant (P = 0.04) (Table 1). Other variables are listed in Table 2.
| Variables | Case Group (N = 25) | Control Group (N = 25) | P-Value |
|---|---|---|---|
| Age, y | 2.92 ± 1.15 | 3.32 ± 2.92 | 0.21 |
| Height, cm | 89.88 ± 8.34 | 93.16 ± 7.17 | 0.14 |
| Weight, kg | 12.99 ± 2.68 | 14.58 ± 2.78 | 0.04 |
Comparison of Mean Age, Height, and Weight in Two Groups
| Variables | Case Group (N = 25), % | Control Group (N = 25), % | P-Value |
|---|---|---|---|
| Male | 44 | 52 | 0.57 |
| Rural living | 60 | 40 | 0.15 |
| Formula usage | 8 | 4 | 0.55 |
| Care center | 8 | 16 | 0.38 |
| Multiple hospitalizations | 8 | 0 | 0.14 |
Frequency Distribution of Samples in Two Groups Based on Variables
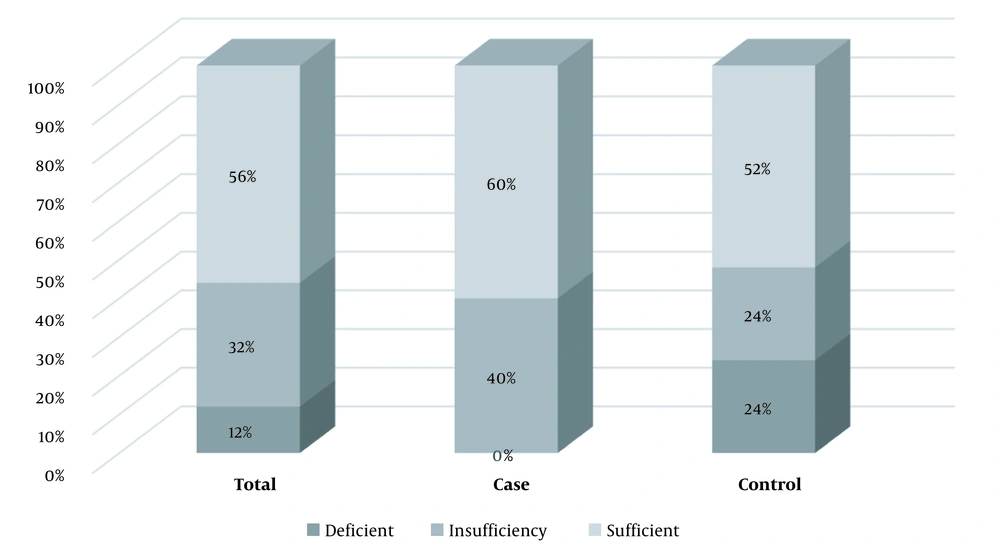
The mean of vitamin D in the case group was 37.50 ± 13.16 ng/mL (min: 23 and max: 75), and the mean of vitamin D in children referred to the clinic was 30.48 ± 11.83 ng/mL (min: 10 and max: 57), and this difference was significant (P = 0.053). Figure 1 shows the prevalence of vitamin D deficiency in children.
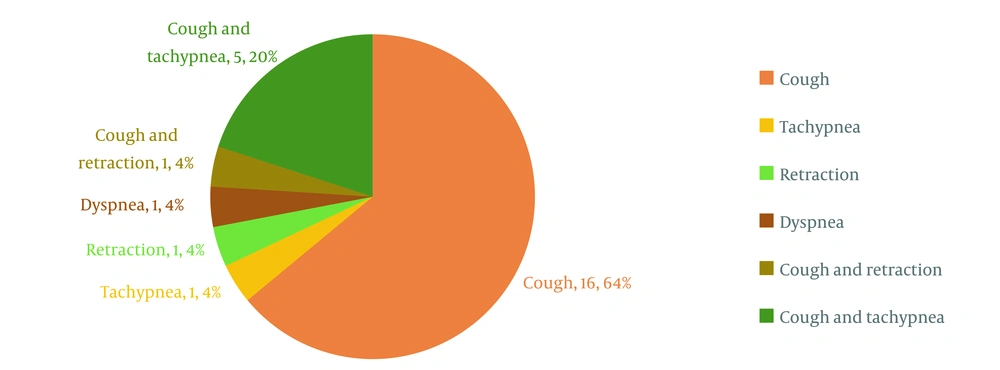
In the case group, the association between vitamin D levels and sex (P = 0.25), place of living (P = 0.48), and attending the care center (P = 0.62) was not significant. Vitamin D levels in the formula group (P = 0.005) and the group with multiple hospitalizations (P = 0.004) was significantly higher (Table 3). According to Figure 2, the cough was the main complaint in the case group.
| Variables | Mean ± SD | P-Value |
|---|---|---|
| Sex | 0.25 | |
| Male | 40.97 ± 15.97 | |
| Female | 34.78 ± 10.27 | |
| Place of living | 0.48 | |
| Village | 39.04 ± 16.06 | |
| City | 35.20 ± 7.13 | |
| Formula usage | 0.005 | |
| Yes | 61.50 ± 19.09 | |
| No | 35.42 ± 10.75 | |
| Care center | 0.62 | |
| Yes | 33.00 ± 5.65 | |
| No | 37.90 ± 13.62 | |
| Multiple hospitalizations | 0.004 | |
| Yes | 62.00 ± 18.38 | |
| No | 35.37 ± 10.69 |
Comparison of Vitamin D Levels in the Case Group
5. Discussion
The aim of this case-control study was to determine the association between vitamin D levels and acute febrile respiratory infections in children referred to Allameh Bohlool Hospital and to compare them with the control group in 2019. In this study, 50 children hospitalized with acute respiratory febrile infections were considered as the cases, and healthy children referred to the outpatient clinic of the hospital were studied as the control group.
In our study, the children were under five years old, similar to other studies such as Garg et al. (25), Wayse et al. (26), Hashemian and Heidarzadeh (10), and Hoseiny-Nejad et al. (15). The mean age of the children in the case group was lower than in the control group. The age range was two to five years. We focused on this age group because acute respiratory infection is the leading cause of mortality in children under five worldwide. We considered the minimum age for enrollment to be two years old because according to the national supplement plan with vitamin D in the age group of 0-24 months, 400 IU/day vitamin D supplement in the form of A + D drops or multivitamin drops are given to them free of charge.
The height of the case group was lower than the control group, but this difference was not significant. Unlike the present study, another survey demonstrated that the mean height of children with pneumonia was significantly shorter than the control group (24). Also, in a study by Wayse et al., a weak positive relationship was observed between short height and acute lower respiratory infection (ALRI), which may be due to some age mismatch in the case and control groups (26).
Consistent with the present study, Kulkarni and Chougule in India found that the relationship between the mean weight of children with pneumonia and the control group was not significant (24). In addition, another study in India, consistent with the results of our study, showed that there was no significant relationship between vitamin D and the location of residence (city or village) (25). On the contrary, in our study, the average vitamin D levels in the urban group were slightly lower than in the rural group.
The mean levels of vitamin D in our case group were 37.50 ± 13.16 ng/mL. In a study conducted by Sismenlar et al. (12) in Turkey, the mean serum levels of vitamin D in children with lower respiratory tract infection (LRTI) were 34.9 ± 22.1 ng/mL, which is almost similar to our study. The mean serum levels of vitamin D in another study in India (24) in children with pneumonia were 12.04 ± 6.015 ng/mL, and in a study in Rasht (10), it was 26.16 ± 15.20 ng/mL. The reason for this difference could be due to environmental factors such as diet, air pollution, amount of sunlight, coverage, height and latitude of the place of residence, season, and length of day.
In our study, vitamin D levels in the group consuming the formula were higher than the other, with a significant difference which may be due to the vitamin D-fortified formulas. Vitamin D levels in children with a history of repeated hospitalization were significantly higher than in the other group. This discrepancy may be due to the fact that serum vitamin D levels were measured in previous hospitalizations, and the treatment was intended for children with a history of recurrent hospitalization. These variables were not evaluated in other studies.
Similar to the findings of McNally et al. (27), we noticed that the difference between the two groups in attending care centers was not statistically significant. Also, in the case group, vitamin D levels in the care center group was lower, but there was no statistically significant difference.
We found that "cough," with a prevalence of 64%, and "cough and tachypnea," with a prevalence of 20%, were the most common chief complaints in the case group. In the study of Sismanlar et al., all children had a cough, and 84% of them had tachypnea (12). In a study by Soleimani et al., cough, fever, tachycardia, and dyspnea were the most common clinical symptoms (3). A study in Brazil reported that tachypnea and intercostal retraction were the most important symptoms of pneumonia in hospitalized patients (28).
In Roth et al. survey (29), a significant relationship was observed between serum vitamin D levels and hospitalization due to ALRI, which was different from our results. The reason for this difference could be the age differences of the chosen groups. In another study, the mean vitamin D levels in children with pneumonia were significantly lower than in the control group (24, 25). In a study in Turkey, no significant difference was observed between the two groups because of using vitamin D supplementation in the first year of life; also, minimum breastfeeding for six months was part of the inclusion criteria (12). Moreover, in the study of Hashemian and Heidarzadeh and Hoseiny-Nejad et al. in Tehran, the serum levels of vitamin D were higher in children with pneumonia, but the difference between the two groups was not significant (10, 15).
In another study, vitamin D levels were measured in hospitalized children. The results showed that one-third of hospitalized children had insufficient vitamin D levels, and children hospitalized due to ALRI had lower levels of vitamin D than hospitalized children with different diagnoses (30). Some studies demonstrated an association between vitamin D deficiency and increased risk of acquiring several infectious diseases, as well as worse outcomes in vitamin D deficient patients with infections (28-30). Even some researchers have found that vitamin D deficiency was associated with an increase in thrombotic episodes and mortality in COVID-19 (28-30). The result of our study indicated that the amount of vitamin D in the case group (37.50 ± 13.16) was higher than in the control group (30.48 ± 11.83), and according to P = 0.053, a significant difference was observed between the two groups. The difference between the present study and mentioned studies was also impressive for us, although this difference can have different reasons. The small sample size of our study could be one of these reasons. We can also point to the age of the children in the case group and the lack of normal distribution of age variables. In the case group, 52% of the children in this study were 2 years old, which was near the age of national supplementation, and this probably influenced the results. In our study, all acute febrile respiratory infections were included, but most studies were performed on a subset of these diseases. For example, in a Canadian study, vitamin D levels were higher in children with bronchitis than in controls, but this difference was not significant (27). The main limitation of our study was its small sample size, which prevented extensive multivariate analysis or detection of an association between acute febrile respiratory infections and possible confounding factors. Also, in sampling, the control and case groups were not matched with each other for other variables. Another important limitation of our study was that we did not evaluate mega dose supplementation in the age group of 2 - 6 years. It is recommended that larger studies with longer follow-up periods should be performed to confirm these results. Considering the fact that in the control group, the consumption of formula and the levels of vitamin D were higher, the frequency of respiratory infections can be justified by the use of formula, which reveals the source of breast milk over other factors involved in the initiation of infection and has a sufficient prevention role. Although some studies have mentioned that vitamin D is important in preventing infections, our study demonstrated that preventing pneumonia with other proven approaches such as vaccinations, hand washing, reducing air pollution, and maybe prophylaxes are more important than just using simple supplements. Identification of the responsible organisms, appropriate and rational use of antibiotics, paying attention to all aspects of children's nutrition, and appropriate and correct use of micronutrients together can be more effective. This study shows the need to conduct more extensive investigations with larger sample sizes and different factors.
5.1. Conclusions
The results of this study demonstrated that the vitamin D serum levels in hospitalized children with acute febrile respiratory infection were higher than in healthy children referred to the outpatient clinic, and the serum levels of vitamin D in the case group were different from the control group.