Introduction
Pustulotic arthro-osteitis (PAO), first described by Sonozaki, is a relatively rare disorder which occurs in about 10-30% of patients with palmoplantar pustulosis [1]. This syndrome was previously considered to be a manifestation of psoriatic arthritis and was then classified by rheumatologists in the SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome [2]. Palmoplantar pustulosis are common manifestations of Sonozaki syndrome which is characterized by recurrent eruptions of sterile pustules situated symmetrically, on the palms and/or soles. PAO is now classified as a seronegative spondyloarthritis which includes ankylosing spondylitis, Reiter's syndrome, and psoriatic arthritis; however, it is not associated with HLA-B27 [3]. The principal lesion in PAO is sternoclavicular involvement but spinal column, sacroiliac and peripheral joints might also be affected.
The disease has always a chronic course with exacerbations and remissions over many years. Treatment is usually symptomatic and consists of analgesics and nonsteroidal anti-inflammatory drugs. Corticosteroids, sulfasalazine, colchicine, methotrexate, and cyclosporine have been used with variable success [2, 4].
Case Presentation
A 51 years old woman was admitted to the department of infectious diseases (Bu-Ali hospital, Zahedan, south-eastern Iran) in April 2012. The patient experienced a swelling and severe pain on the right knee approximately 2 months before her admission for which paracentensis was performed. There is no information about the results of the procedure but the patient received cephalexin, diclofenac and acetaminophen with relative improvement. The patient complained of a dull pain, tenderness and swelling on the right sternoclavicular joint for approximately 1 year before admission. During hospitalization pain and swelling occurred in the right ankle with symmetrical pustular lesions on the palms of her both hands. The patient had no history of rheumatological diseases or psoriasis and there was no history or clinical evidence of these diseases in her family. She had no history of eating unpasteurized milk or dairy product. On physical examination, swelling and erythema were observed over the right sternoclavicular joint and ankle with tenderness on palpation.
Sharply demarcated erythematosquamous lesions with pustules were seen on the palms of both hands. While there was pain on palpation of the right ankle, the range of motion was normal. The findings of the remainder of the physical examinations were normal. In laboratory findings the patient's white blood cell count was 11200/mm3 with normal differentiation. The hemoglobin and platelet count level were 10.8 g/dL and 350,000/mm3, respectively. The erythrocyte sedimentation rate (ESR) was 115 mm/h (normal <20 mm/h) and C-reactive protein (CRP) was reported 7.45 mg/dL (normal<0.8 mg/dL).
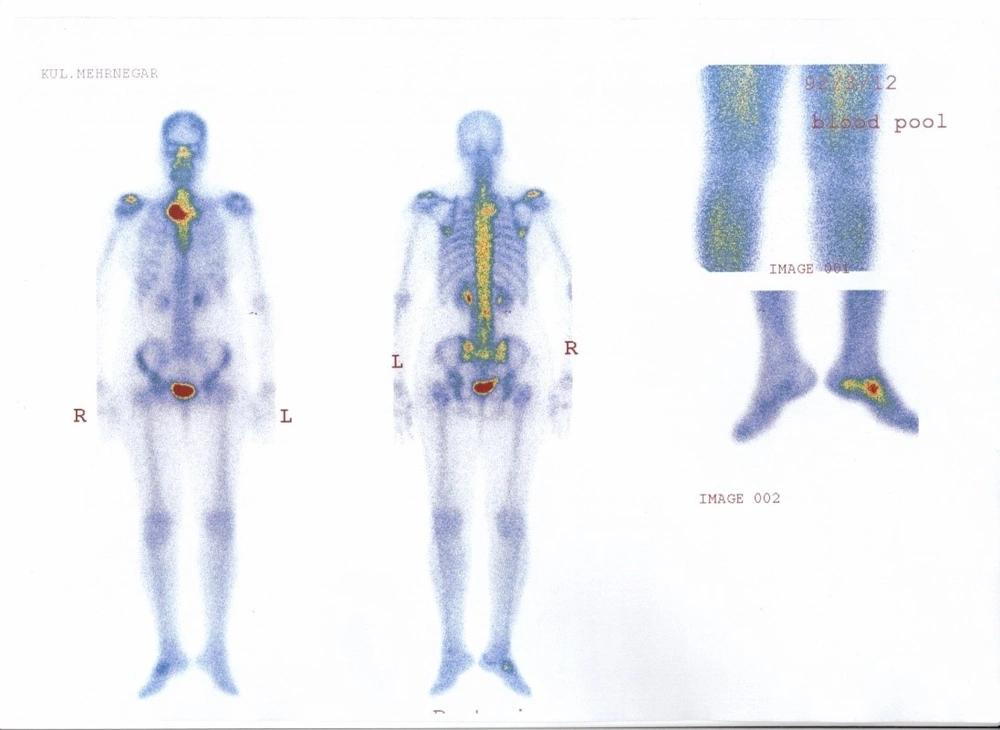
Serum was negative for rheumatoid factor, antinuclear factor, anti-dsDNA, and anti-Sm antibodies. Wright, coombs wright and anti-Brucella ELISA were negative. C3 and CH50 were reported slightly above the normal range but C4 was in the normal range. HLA-B27 was negative. Other laboratory values, including the results of biochemical tests were within normal limits. X-ray and computed tomography scan of the right ankle and the sternocostoclavicular region revealed soft tissue swelling. A technetium-99 m diphosphonate-labeled scintigram of bones revealed severe increased radiotracer uptake in the right sternoclavicular joint and slightly increased radiotracer uptake in the right acromyion process and right cuboid bone (Fig. 1).
Skin biopsy from pustular and skin lesions showed spongiosis and dyskeratotic cells in the basal layer and infiltration of polymorphonuclear cells. The culture of pustular aspirate was negative. The patient was started on prednisolone 1 mg/kg/day with dramatic improvement after one week of treatment.
Discussion
Sonozaki syndrome is a rheumatic syndrome of unknown etiology and is considered as a member of the seronegative spondylo-arthritis group. The diagnosis of Sonozaki syndrome in our patient was made according to the clinical manifestations, scintigram findings and histopathologic features. However, response to corticosteroid therapy was another clue for the diagnosis. Sternoclavicular joints are the most common joint affected in PAO. Among the peripheral joints, metacarpophalangeal joints, the proximal interphalangeal joints of fingers, the elbow and knee joints are most commonly affected. Involvement of other joints such as the hip, the ankle, and the wrist joints have also been reported [5].
Hyodoh and Sugimoto include Sonozaki syndrome in the group of the seronegative arthropathies of unknown basis [6]. Nagel et al. reported 11 cases of the Sonozaki syndrome in which the maximal period between appearance of skin and arthro-osteitis was approximately 6 years [3]. In a recent case record a woman aged 55 with a diagnosis of Sonozaki syndrome and hyperthyroidism was reported [2]. Su et al. described a Turkish patient who presented with palmoplantar pustulosis and involvement of the sternoclavicular joint and peripheral oligoarthritis with good response to prednisolone and dapsone [5]. Jang et al. described four cases of pustulotic arthro-osteitis. All of the patients suffered from anterior chest wall symptoms including swelling and pain on the sternoclavicular joint, sternal angle area, sternocostal joint, and costochondral junction. Moderate improvement of the skin lesions on the palms and soles and the arthro-osteitis was observed after treatment with non-steroidal anti-inflammatory drugs and etretinate [7]. Successful treatment of pustulotic arthro-osteitis (Sonozaki syndrome) with systemic cyclosporine was reported by Vaccaro et al. [4]. Early and correct diagnosis of the disease decreases the risk of potential complications, such as systemic amyloidosis [2].
In our patient, the sternoclavicular joint arthritis was preceded by pustular skin eruption and elevated CRP and ESR were the only significant laboratory abnormalities. Increased radiotracer uptake in the right sternoclavicular joint and clinical improvement after corticosteroid therapy was both helpful to make the diagnosis of Sonozaki syndrome in our patient.