Introduction
Systemic lupus erythematous (SLE) is a multisystem autoimmune inflammatory disease. The pathological hallmark of SLE is diverse vascular injury including inflammatory vasculopathy. Gastrointestinal (GI) symptoms are common in the course of SLE and occur in up to 50% of cases [1]. The most serious GI manifestation of SLE is ischemia secondary to vacuities. The reported incidence of lupus enteritis or mesenteric vacuities ranged from 0.2% to 53% [2] and with mortality rate as high as 53% if complicated with hemorrhage, ulceration, infarction, or perforation, or if treatment is delayed [3]. In this paper, we describe 2 cases of severe, recurrent lupus mesenteric vacuities accompanied with significant hypocomplementemia as the initial presentation of SLE.
Case Presentation
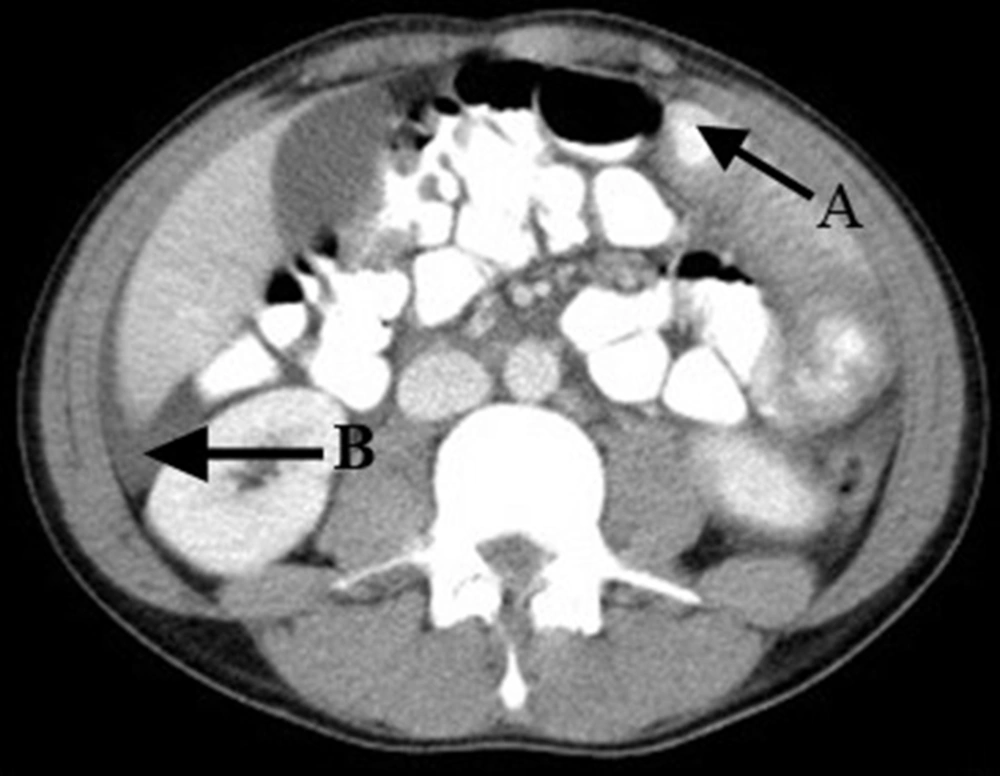
Case 1: In January 2012, a 30 years old man referred to emergency department of Shahid Beheshti hospital of Qom with acute onset of diffuse abdominal pain associated with nausea and vomiting. He had 3 episodes of abdominal pain within 3 past months. CT scan with contrast showed marked bowel wall thickening involving the jejunum with mild ascites, findings most compatible with intestinal ischemia (Fig. 1). The patient underwent exploratory laparoscopic surgery which ruled out necrotic bowel but there was only significant edema of small bowel.
After excluding other causes of ischemic enteritis, the autoimmune profile was checked: a low serum complement level (C3/C4: 29/9 mg/dL, normal range: 80-180/15-40 mg/dL), positive antinuclear antibody (1:320), and anti-ds-DNA antibody: 1:160. Anti-cardiolipin antibodies (IgG and IgM), lupus anticoagulant, c,p-ANCA and anti-β2-glycoprotein antibody were negative.
Diagnosis of lupus vacuities involving the small bowel was done and his abdominal symptom resolved 2 weeks after steroid therapy. Repeat CT scan of abdomen 3 months later showed resolution of the small bowel edema. One year follow up of the patient was with no recurrent abdominal pain.
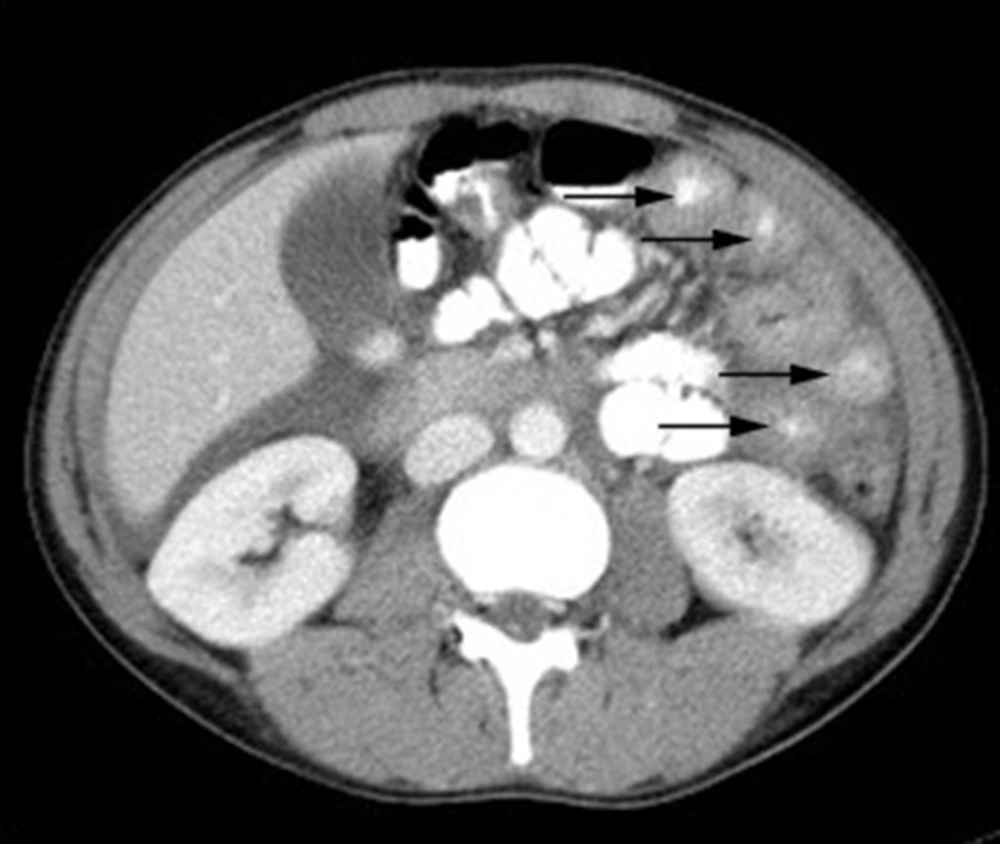
Case 2: In September 2012, a 22 years old woman was admitted with recurrent abdominal pain with poor intake for 2 months to our GI ward of 5-Azar hospital of Goletan. Physical examination revealed whole abdominal tenderness, but no obvious rebounding pain or muscle guarding was noted. Upper GI endoscopy revealed hyperemia in the tantrum with no ulceration or other abnormalities. CT scan showed extensive small bowel mural thickening demonstrating a target sign enhancement appearance with as cites (Fig. 2).
Ischemic enteritis was suspected and after excluding other causes of ischemic enteritis, the patient’s autoimmune profile was checked and revealed a low serum complement level (C3/C4: 38/6 mg/dL, normal range: 80-180/15-40 mg/dL), positive antinuclear antibody (1:320), and anti-ds-DNA antibody: 1:80. Lupus enteritis was diagnosed and she was discharged with no abdominal discomfort after oral intake on 16th day hospitalization without any surgical intervention after steroid therapy. Six months follow up of this patient was with no recurrent mesenteric vacuities.
Discussion
Lupus mesenteric vacuities (LMV) is an uncommon cause of acute abdominal pain in SLE patients.
In Asia, the reported overall prevalence of LMV in patients with SLE is 2.2-9.7% but the prevalence of LMV in America seems to be much lower (0.9%) [4, 5]. Both the inflammatory and thrombotic mesenteric vasculopathy of LMV can cause mesenteric ischemia. Accurate diagnosis of LMV is critical to allow prompt treatment to avoid unnecessary surgical intervention. The diagnosis of LMV relies on abdominal CT scan.
Immediate, high dose, intravenous steroid therapy can lead to a favorable outcome and prevent serious complications such as bowel ischemia, necrosis and perforation [6]. Medina et al. report that the mortality of LMV could be as high as 50% [7]. The prognosis of LMV can be improved if abdominal CT is used to aid the diagnosis and if prompt immunosuppressive therapy is implemented [6].
Medina et al. [7] reported that lupus enteritis occurs when patients have laboratory markers of active disease and a raised SLE disease activity index (SLEDAI) score but Lee et al. [7] demonstrated that the SLEDAI score was similar at the time of acute abdominal pain in both patients with mesenteric vacuities and those with other causes of acute abdominal pain. Because GI symptoms are not considered in the SLEDAI score and hypocomplementemia was found in Lin et al.'s study and in our patients, the serum C3/C4 level rather than the SLEDAI score may able to predict whether the GI symptoms in lupus patients are related to SLE itself or other non-lupus causes [1]. Recurrent lupus mesenteric vacuities may be the initial presentation of SLE; early diagnosis and appropriate intervention can avoid potentially fatal complications of LMV. SLE should be suspected in all patients with CT findings of ischemic enteritis, even without lupus-related symptoms or signs and C3/C4 levels may be helpful in the differential diagnosis.