1. Introduction
The novel coronavirus disease 2019 (COVID-19), recognized as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is regarded as a critical public health issue. Severe pneumonia and acute respiratory distress syndrome are distinct features of COVID-19, causing a remarkably high rate of mortality (1).
Amid the COVID-19 pandemic, physicians, due to their leading role in health provision, were exposed to high work burdens. During the pandemic, physical exhaustion and mental distress due to the fear of contracting the infection led most clinicians to spend the least possible time with patients (2). Furthermore, several factors, such as the prolonged wearing of personal protective clothing with extreme heat, insufficient hydration, poor nutrition, sleep deprivation, and extra work shifts, all at once made tiredness and burnout inevitable consequences. On the other hand, physician burnout compromises patient safety and the quality of care and increases the rate of misdiagnosis (3).
During the COVID-19 pandemic, physicians should closely monitor all possible scenarios in patients to minimize the possibility of medical errors. Misdiagnosis is defined as failing to precisely or promptly diagnose a clinical condition (4, 5). Herein, we report the case of an old woman presenting with fever, cough, and shortness of breath initially misdiagnosed as COVID-19, which resulted in a delayed diagnosis of lymphoma and the demise of the patient.
2. Case Presentation
We report a 73-year-old married female who was brought to our emergency department by her son during the early phase of the COVID-19 pandemic in Iran (March 24, 2020). The patient was fully conscious and complained of cough, shortness of breath, fatigue, myalgia, chills, and fever. She reported contact with her family members who tested positive for COVID-19 (i.e., her husband and her son). The medical history included diabetes mellitus, hypertension, asthma, and chronic renal disease. Her clinical examination was unremarkable except for splenomegaly.
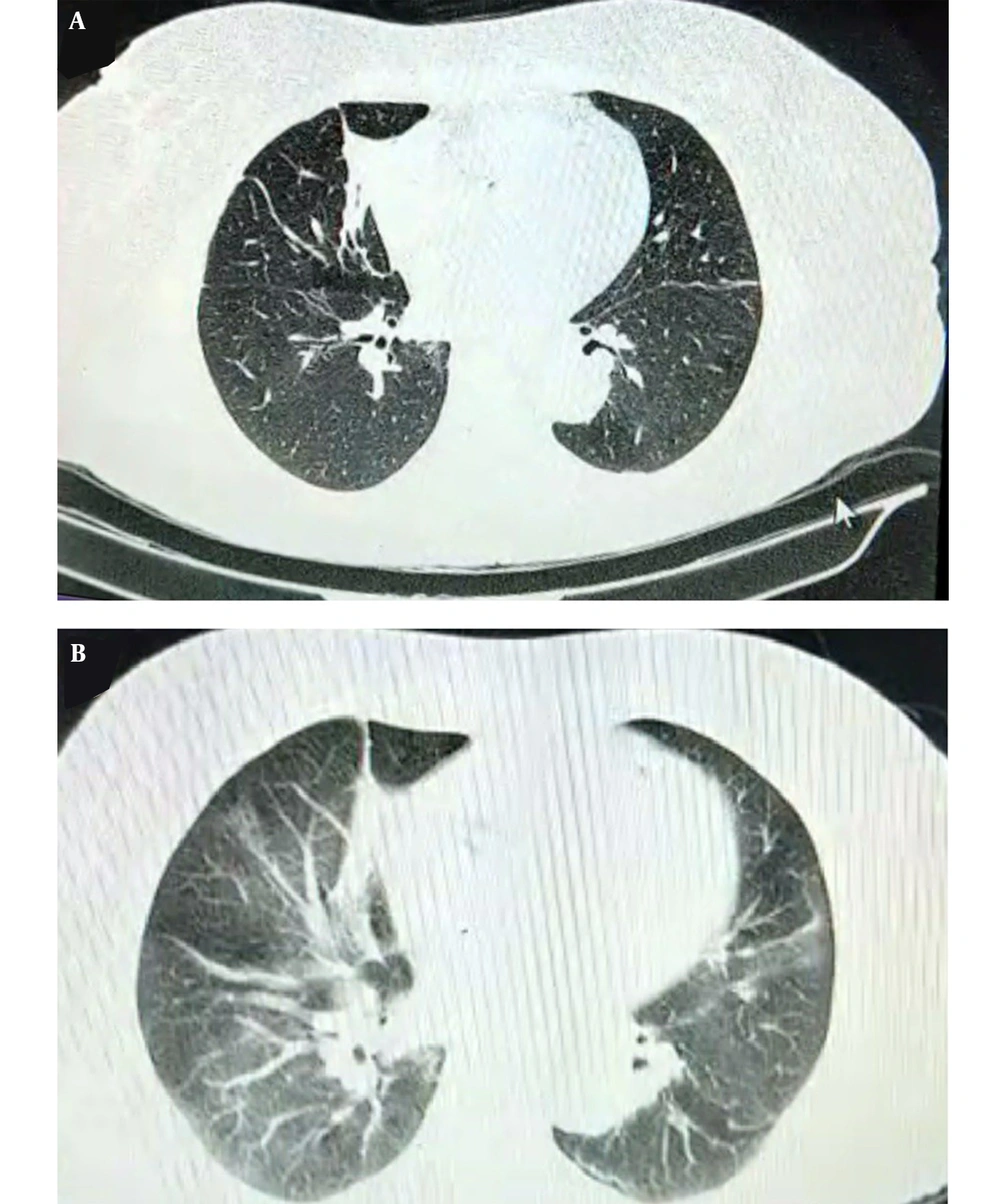
On admission to the emergency department, fever (38°C), dyspnea (a respiratory rate of 28 breaths/min), and oxygen saturation of 90% in room air were recorded for the patient. Bilateral inspiratory crackles were also reported for the patient. Moreover, the chest X-ray and computed tomographic (CT) scan of the lung revealed bilateral interstitial markings and bilateral hilar lymphadenopathy with lower bilateral interstitial lung densities (Figure 1A). Laboratory investigations were prominent regarding elevated C-reactive protein (26.8 mg/dL, normal range: < 6) and lactate dehydrogenase (1705 U/L, normal range: 230 - 480), as well as thrombocytopenia (platelet count: 90 × 1000/μL, normal range: 140 - 450). No evidence of myeloproliferative neoplasms was observed in bone marrow aspiration.
Echocardiography showed an ejection fraction of 55% and mild left ventricle hypertrophy. Hepatosplenomegaly and lymphadenopathy in the porta hepatis and coeliac axis were detected in abdominal ultrasound. The results of nasopharyngeal swab testing for multiple respiratory pathogens, including SARS-CoV-2, were negative using multiplex polymerase chain reaction on admission. However, the initial diagnosis was COVID-19 infection. She stayed at home for two weeks and did not appear in any public place. Her condition improved with hydration, analgesics (acetaminophen), and antibiotics (azithromycin).
Four months later, the patient was readmitted to the hospital for upper gastrointestinal (GI) bleeding. Various symptoms and signs not detected during her initial admission, including cervical lymphadenopathy and weight loss of about 20 kg in the last month, were evident upon careful examination. Upper GI endoscopy revealed mild pangastritis and duodenal erosion. Table 1 shows basic clinical parameters after visiting a specialist.
| Tests (Unit) | Result | Reference Value |
|---|---|---|
| Hematology | ||
| WBC × 103/mm3 | 5.1 | 4000 - 10000 |
| Neutrophils (%) | 62 | 36 - 80 |
| Lymphocytes (%) | 36 | 16 - 51 |
| RBC × 106/mm3 | 3.27 | 4.5 - 6.3 |
| Hb (mg/dL) | 10.4 | 14 - 18 |
| HCT (%) | 28.8 | 39 - 52 |
| MCV (fL) | 88.07 | 80.0 - 100 |
| MCH (pg) | 31.8 | 27 - 32 |
| MCHC (g/dL) | 36.11 | 31 - 36 |
| ESR (mm/hr) | 98 | Up to 15 |
| PT (Sec) | 14.1 | 10 - 13 |
| PT control (Sec) | 11.5 | 70 - 100 |
| INR (%) | 1.3 | 0.9 - 1.0 |
| PTT (Sec) | 27 | 24 - 42 |
| CRP | 48 | < 6 |
| TIBC (μg/dL) | 270 | 250 - 450 |
| Biochemistry | ||
| BUN (mg/dL) | 63 | 7 - 23 |
| Creatinine (mg/dL) | 5.5 | 0.6 - 1.1 |
| Serum Na (mEq/L) | 135 | 135 - 145 |
| Serum Ca (mg/dL) | 6.2 | 8 - 10 |
| Serum K (mEq/L) | 3.5 | 3.5 - 5.2 |
| Serum Mg (mg/dL) | 2.3 | 1.5 - 2.5 |
| AST (IU/L) | 57 | Up to 31 |
| ALT (IU/L) | 28 | Up to 32 |
| ALP (IU/L) | 60 | 64 - 306 |
| LDH (IU/L) | 2100 | 225 - 500 |
| Total bilirubin (mg/dL) | 0.5 | 0.2 - 1.2 |
| Direct bilirubin (mg/dL) | 0.21 | 0 - 0.3 |
| Amylase (U/L) | 150 | < 100 |
| Fe (μg/dL) | 152 | 35 - 155 |
| CPK (IU/L) | 40 | Up to 170 |
| ALB (g/dL) | 3.9 | 3.5 - 5 |
| ACE (ng/dL) | 92 | 13.3 - 63.9 |
| ANA (U) | 0.62 | Negative < 0.9; borderline 0.9 - 1.1; positive > 1.1 |
| P-ANCA (U) | < 1/10 | Negative < 1/10; positive > 1/10 |
| C-ANCA (U) | < 1/10 | Negative < 1/10; positive ≥ 1/10 |
| Blood gas analysis (VBG) | ||
| pH | 7.34 | 7.31 - 7.41 |
| PCO2 (mmHg) | 42.2 | 35 - 40 |
| HCO3(mEq/L) | 22.5 | 22 - 26 |
| PO2 (mmHg) | 36.7 | 41 - 51 |
| Urine analysis | ||
| Color | Yellow | - |
| pH | 5 | 4.5 - 8.0 |
| Protein | Negative | Negative |
| Glucose | Negative | Negative |
| Blood | Positive (+++) | Negative |
| Urobilinogen | Normal | Negative |
| Bilirubin | Negative | Negative |
| Keton | Negative | Negative |
| Nitrite | Negative | Negative |
| WBC/h.p.f | 10 - 12 | 0 - 5 |
| RBC/h.p.f | Many | 0 - 3 |
| Epithelial cells/h.p.f | 32 - 40 | 1 - 5 |
| Bacteria | Moderate | 0 - 1 |
Basic Clinical Parameters
Table 2 shows the results of blood tests on readmission. Lymph node biopsy revealed diffuse large B-cell lymphoma (CD45 and CD20, positive diffuse; CD5, positive a few; Ki67, positive about 50%; MNF116, CD56, and S100, negative). Unfortunately, the patient passed away a week after readmission. Figure 1B shows a section of the lung CT scan on rehospitalization.
| Test (Unit) | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Reference Value |
|---|---|---|---|---|---|---|---|---|
| WBC × 103/mm3 | 13.9 | 9.3 | 7.9 | 5.4 | 3.7 | 4.4 | 4.1 | 4 - 11 |
| RBC × 106/mm3 | 3.1 | 2.86 | 3.2 | 3.1 | 3.1 | 3.5 | 3.06 | 4.5 - 6.3 |
| Hb (mg/dL) | 8.6 | 7.8 | 9.5 | 9.2 | 8.9 | 10.3 | 8.7 | 14 - 18 |
| HCT (%) | 27.5 | 25.6 | 28 | 27.5 | 26.9 | 31.4 | 27.5 | 39 - 52 |
| PLT × 103/μL | 35 | 25 | 24 | 27 | 25 | 28 | 25 | 140 - 450 |
| Neutrophils (%) | 78 | 45 | 64 | 53 | 58 | 60 | 65 | 4000 - 10000 |
| Lymphocytes (%) | 20 | 53 | 64 | 45 | 40 | 38 | 32 | 25 - 45 |
| MCV (fL) | 88.4 | 89.51 | 87.5 | 87.6 | 86.77 | 86.9 | 89.87 | 80.0 - 100 |
| MCH (pg) | 27.7 | 27.27 | 29.69 | 29.3 | 28.71 | 28.2 | 28.43 | 27 - 32 |
| MCHC (g/dL) | 31.3 | 30.47 | 33.93 | 33.5 | 33.1 | 32.5 | 31.64 | 31 - 36 |
Hematologic Parameters on Rehospitalization
3. Discussion
We reported the case of a patient with a delayed diagnosis of lymphoma and, therefore, delayed onset of treatment during the COVID-19 pandemic. Similarly, Yousefzai and Bhimaraj reported a failure to diagnose ST-segment elevation due to myocardial infarction during the COVID-19 pandemic (5). During the pandemic, most diagnostic orientations were focused on COVID-19, driving out of mind many diseases with overlapped symptoms. Besides, retrospectively identifying the cases of missed or delayed diagnosis by reviewing medical records is a complicated task unless patients keep receiving similar care services. Therefore, most misdiagnoses remain undetected.
Based on the literature, individuals with a delayed onset of cancer therapy, even for one month, bear a 6 - 13% higher risk of mortality (6). Patient delay and health care system delay refer to the two-step interval from the onset of patient symptoms to therapy initiation. In line with the results of the current study, Dang-Tan et al. reported that the cancer subtype was associated with patient delay in those with leukemia, while the healthcare system delay was more related to lymphoma (7).
Even prior to the global outbreak of COVID-19, some studies in developed countries had noted delayed diagnosis of lymphoma as a serious concern (8, 9). Multiple barriers to diagnosis have been detected, namely non-specific symptoms, the lack of a distinct referral pathway for lymphadenopathy, and insufficient tissue biopsies for diagnosis (i.e., fine needle aspirates for cytology examinations have a low diagnostic yield for lymphoma) (10). Several studies have emphasized that lymphoma can be misdiagnosed as tuberculosis (TB), and in TB endemic regions, up to 85% of lymphoma cases may be at first misdiagnosed as TB (11, 12).
Moreover, major clinical symptoms (e.g., lymphadenopathy or splenomegaly) can be easily missed in emergency departments during the COVID-19 pandemic. Excisional lymph node biopsies were reduced or canceled due to the high workload of COVID-19 wards. Antel et al., in their study, proposed establishing a rapid-access lymph node biopsy clinic to reduce diagnostic delay for lymphoma amid the COVID-19 era (13).
The COVID-19 pandemic was a universal unparalleled incident greatly affecting all healthcare systems, and it is required for specialists to be well-prepared beforehand to encounter diagnostic dilemmas during such exceptional conditions (14). The COVID-19 pandemic affected the everyday tasks of health centers and reduced their capacity to deliver elective services, accentuating the necessity of patient triage and paying attention to probably overlapped disease presentations. Regulations and recommendations were constantly changing as the pandemic gradually developed, requiring further preparedness and resilience among healthcare professionals to ensure patient safety and deliver satisfactory medical performance (15, 16).
3.1. Conclusions
In COVID-19 care units, it is necessary to consider the precise and periodic re-evaluation of individuals primarily diagnosed with COVID-19 to identify possibly missed diagnoses. The COVID-19 pandemic poses a new challenge to hematologists/oncologists who need to be more vigilant about lymphoma patients and enhance research efforts to optimize diagnostic algorithms for these patients during the COVID-19 pandemic.