1. Background
Infrequent voiding is associated with urinary tract infection (UTI) (1); this condition may be associated with a weak bladder muscle, a blockage in the flow of urine, behavioral problems, or habits that develop over time (2). The prevalence of infrequent voiding was different in some studies, but approximately 5 - 15% was observed in different age ranges (3). Affected children are often girls who urinate 2 times per day; normal urination is 4 to 7 times per day. With excessive bladder dilation and prolonged urinary retention, bacterial growth leads to recurrent urinary tract infections (2, 4). Some of these children also have constipation, and some sometimes have overflow incontinence (5, 6). As a problem in these patients, UTI may accompany the behavioral disorder; treatments include antibacterial treatment, encouraging repeated urination, and complete voiding by double voiding until the normal urination pattern is restored (7, 8). Since this problem and associated urinary tract infection cause developmental disruption (3), studies on developmental disabilities and infrequent voiding have been poorly studied. At the same time, treatment of this condition seems to be effective in improving the growth and development of these children; in addition, previous studies have evaluated other urinary disorders.
2. Objectives
In the present study, we have considered infrequent voiding as our main aim disorder, so we compared the growth and development of normal cases with infrequent voiding ones.
3. Methods
3.1. Study Setting
This is a hospital-based, case-control study conducted in the pediatric clinic at Amirkabir Hospital.
3.2. Study the Population
We considered 200 children for study conduction; in representative sampling, 100 children with infrequent voiding as the case group and 100 healthy ones as the control group; we used a simple sampling method to enroll cases for the study. Children were taken from male and female gender and 6 to 7 years of age, with infrequent voiding. Patients who have all the Infrequent Voiding criteria and were never controlled and treated were included in the study. Patients with chronic systemic disease, including heart failure, liver failure, diabetes, renal failure, growth hormone deficiency, malabsorption, asthma, and others, could affect children's growth. In addition, diseases other than infrequent voiding, those with mental retardation, or other underlying neuropsychiatric disorders that affect development, and patients who do not cooperate are excluded. We controlled the confounders by restricting the study population and matching the two comparison groups about some factors.
3.3. Measurements
We take the study population at the same levels in both groups concerning demographic and socio-economic issues. In two groups, height and weight were measured and compatible with gender and age. In addition, personal and social development, problem-solving, fine motor, gross motor, communication, and linguistic evolution have been obtained by ASQ (Ages and Stages Questionnaires) and Nelson development table (9). Validity and reliability are 0.84 and 0.94, respectively, and the ability of the test to determine developmental disorders is more than 96% (10).
3.4. Ethical Considerations
The authors have observed ethical issues (including plagiarism, data fabrication, and double publication). In addition, the ethical committee of Arak University of Medical Sciences approved the study protocol, with the approval code as IR.ARAKMU.REC.1391.124.6.
3.5. Statistical Analysis
Data analysis was conducted by chi-square and t-test in the SPSS program, and significance levels (P < 0.05) were considered. In addition, we have compared two groups based on the OR calculation of different indices.
Inclusion and exclusion criteria
3.5.1. Inclusion criteria
- Each child 6 to 7 years old,
- With infrequent voiding
- And not treated in the past.
3.5.2. Exclusion criteria
- Children with mental disorders,
- Any systemic diseases,
- Not having the necessary cooperation in the study,
- And any other disorders that affect the development of children.
In total, 120 children in the case group and 120 healthy children in the control group based on inclusion criteria have been enrolled to study; in addition, after consideration of exclusion criteria, 20 cases in any group have been excluded, and 100 cases have been allocated in the study.
4. Results:
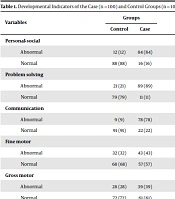
Of evaluated cases in the personal-social (P = 0.009), problem-solving (P = 0.006), communication (P = 0.008), and language development (P = 0.006) have a statistically significant difference between the two groups. In addition, based on the odds ratio (OR) of evaluated indices, all developmental indicators have direct communication with infrequent voiding (Table 1)
| Variables | Groups | P-Value | OR | |
|---|---|---|---|---|
| Control | Case | |||
| Personal-social | 0.009 | 38.54 | ||
| Abnormal | 12 (12) | 84 (84) | ||
| Normal | 88 (88) | 16 (16) | ||
| Problem solving | 0.006 | 30.5 | ||
| Abnormal | 21 (21) | 89 (89) | ||
| Normal | 79 (79) | 11 (11) | ||
| Communication | 0.008 | 35.4 | ||
| Abnormal | 9 (9) | 78 (78) | ||
| Normal | 91 (91) | 22 (22) | ||
| Fine motor | 0.57 | 1.6 | ||
| Abnormal | 32 (32) | 43 (43) | ||
| Normal | 68 (68) | 57 (57) | ||
| Gross motor | 0.60 | 1.6 | ||
| Abnormal | 28 (28) | 39 (39) | ||
| Normal | 72 (72) | 61 (61) | ||
| Language development | 0.006 | 33.4 | ||
| Abnormal | 12 (12) | 82 (82) | ||
| Normal | 88 (88) | 18 (18) | ||
Developmental Indicators of the Case (n = 100) and Control Groups (n = 100).
On the other hand, in terms of growth indices, in the survey of girls height index > 50 percentile, and the < 50 percentile (P = 0.001), height index > 50 percentile, and the < 50 percentile (P = 0.012), weight > 50 percentile, and in > 50 percentile (P = 0.014), weight > 50 percentile, and weight < 50 percentile (P = 0.016), there is a statistically significant difference. In addition, accordingly, the weight and height of the two groups were significantly different in the two groups. Also, based on ORs, weight has a direct link, and height has an indirect link to infrequent voiding (Table 2).
| Domains | Groups | P-Value | OR | |
|---|---|---|---|---|
| Control | Case | |||
| Height (female) | 0.001 | 0.45 | ||
| < 50% | 23 (23) | 12 (12) | ||
| > 50% | 77 (77) | 88 (88) | ||
| Height (male) | 0.012 | 0.24 | ||
| < 50% | 49 (49) | 19 (19) | ||
| > 50% | 51 (51) | 81 (81) | ||
| Weight (female) | 0.016 | 68.2 | ||
| < 50% | 9 (9) | 87 (87) | ||
| > 50% | 91 (91) | 13 (13) | ||
| Weight (male) | 0.014 | 42.7 | ||
| < 50% | 11 (11) | 84 (84) | ||
| > 50% | 89 (89) | 16 (16) | ||
Growth Indicators of the Case (n = 100) and Control Groups (n = 100)
5. Discussion
In the present study, infrequent voiding cases have a higher rate of developmental and growth disorders than healthy ones, so based on these results, detailed physical examinations and careful history were important in infrequent voiding's first investigation. However, in other studies, some other results have been discussed in the following.
In a study of patients with enuresis, Touchette et al. reported that the highest incidence of enuresis was in children between 29 and 41 months. In boys with enuresis, motor development was lower than in controls. In addition, they reported that enuresis was earlier than control girls and was more likely to be overactive and inattentive. Speech skills were also lower in the enuresis group than in the control group, but there was no difference in physical growth and sleep patterns between the two groups (11). Accordingly, the similarity of the study with the recent study on speech skills deficits has shown the importance of correcting this problem in all children with enuresis. In addition, Birenbaum and Cunha in another study, reported that children with enuresis had a higher prevalence of language disorders compared to uninfected children, and this disorder was particularly widespread in phonology and speech (12). Accordingly, this study, equal to the recent study of language disorders in children with enuresis, has proven that by correcting this disorder, the major problem of the inability to control urine can be partially remedied and subsequently improved in patients.
In another study, Sarici et al. reported that bone density and age in children with nocturnal enuresis were significantly lower than those of non-affected children and that chronological age was higher than bone age in the affected group. In contrast, it was not significantly different in the control group (13). The present study, such as the recent study of development and as a consequence of height in children with enuresis, has been found to be effective in improving enuresis by correcting growth problems and short stature treatment. In addition, Nuhoglu et al. reported no direct relationship between nocturnal enuresis and skeletal puberty (14). von Gontard et al. also evaluated patients with enuresis and used Zurich's evaluation of neuromotor development to evaluate whether children with enuresis had slower motor development than controls (15). In this study, motor development in children with nocturnal enuresis, in contrast to our study, was impaired. The limitation of our study was the low number of cases in the evaluated groups and the lack of cooperation by some patients and their parents. However, based on this, other studies, especially prospective ones with more cases, evaluate the correlation of infrequent voiding with developmental and growth disorders.
5.1. Conclusions
We have evaluated the association between infrequent voiding and developmental disorders in children as our main aim. Based on ORs, children with infrequent voiding have a higher risk of developmental disorders; also, developmental disorders can increase the prevalence of infrequent voiding. Based on this, we can reduce growth and developmental disorders by the treatment of infrequent voiding in male and female children.