1. Background
Sexual problems are often expressed as secrets, and individuals are embarrassed or feel ashamed to address them. Individuals' refusal to seek help for specific sexual problems has led to the negligence of these disorders, resulting in limited treatments (1, 2). Premature ejaculation (PE) is one of these problems and is a common sexual dysfunction in men. Even though the true prevalence rate of PE is not specified, it might affect 20 to 30% of men regardless of age and race (3). PE affects various aspects of the patient's life, including mental and emotional health and interpersonal relationship with their spouse (4). Despite this, PE is a part of men's sexual health that is generally disregarded, indicating an unmet medical need. This is probably due to many factors, such as the low rate of seeking medical help due to shame and physicians' confusion regarding the clinical management of this dysfunction (5, 6). PE in men can lower self-esteem and lead to concerns regarding the impact of this problem on the quality of their interpersonal relationships. The main impact of PE on men's lives is diminished sexual confidence. Anxiety about performing well, shame regarding the current state, and depression are among the effects caused by PE in men (7). Various treatments have been suggested for this disorder; however, their effects are not permanent or inclusive.
A few drug therapies have been suggested for PE, none of which are currently approved as effective treatments. Tricyclic antidepressants (TCAs) are effective in treating PE; however, their use is restricted because of their considerable side effects, such as anticholinergic effects, including nausea, dry mouth, blurred vision, and cardiovascular toxicity (8, 9). Clomipramine is a primary agent used as PE treatment and has proven effective in increasing the time interval between penetration and ejaculation. Tramadol has also been tested as a potential treatment for PE. The exact mechanism is unknown, but it is assumed that tramadol might operate as an agonist, an antagonist of the HT2C5 receptor, and a modulator of serotonin and norepinephrine (noradrenaline) (10). Considering the limited research base, it is essential to conduct more investigations to determine the safety and effectiveness of drugs for these patients. Moreover, psychotherapy is another option that can benefit patients with PE.
Psychotherapy might provide patients with PE with a mental, natural, or acquired variable and specify this disorder's interpersonal or psychological causes (6). The physician can discover and examine deeper psychological and interpersonal factors in these methods. Psychological treatment might be effective in reducing the distress associated with PE. The evidence that supports the psychological procedures to manage PE is contradictory and lacks long-term follow-up (8). Some have posed the question of whether PE is merely psychological.
Some researchers have found differences in nerve conduction/delay and hormonal differences in men with PE compared with men who do not experience PE. This theory states that some men suffer from excessive stimulation or sensitivity of reproductive organs, which prevents the regulation of sympathetic paths and leads to a delay in orgasm (3, 11). Electroencephalography studies and neuroimaging have detected abnormal responses and activation of the brain to ergogenic stimulation and changes in brain structure in patients with PE. A study by Lu et al. (12) used functional magnetic resonance imaging (fMRI) and demonstrated that patients with lifelong PE have an abnormal brain control network that facilitates the reduction of central control of early ejaculation. Ejaculation is a spinal reflex subject to acute neuromodulation. It comprises two steps. Discretion and discharge of this coordination guarantee the unstable propulsion of semen. It secretes into the urinary tract and is followed by discharge, a process in which rhythmic muscular contractions and pelvic muscles lead to the movement and discharge of semen through the urinary tract (13-15). Examining transcranial direct current stimulation (tDCS) can effectively treat PE since the brain is effective in these actions and reactions.
Brain stimulation includes invasive and non-invasive methods currently discussed in the field of neurological sciences (16, 17). tDCS is a method that applies a continuing and low-intensity electrical current to the head. This type of stimulation is an invasive method to stimulate the brain, which is influential in modulating cortical arousal and the direction of human behavior and perception (18, 19). Over the past two decades, numerous studies have demonstrated positive clinical results using this method (20). Transcranial direct current stimulation is a weak current that causes temporary changes in the stimulation of cortical regions. Physical parameters of tDCS include current severity, stimulation site, electrode size, stimulation duration, and current polarity (anode or cathode), each of which causes different effects (21). In this method, large electrodes are placed on the head that passes through a continuous and weak current. The effectiveness of tDCS depends on the direction of the electrical current. Anode stimulation increases the brain's activity and stimulation, and cathode stimulation reduces it (22, 23).
2.Objectives
This study aimed to investigate the effects of tDCS on the treatment of PE in men with sexual dysfunction.
3. Methods
3.1. Design and Participants
The study was quasi-experimental with a pretest-posttest control design and a two-month follow-up. The statistical population of this research included all men with PE living in Tehran who visited sexual health centers in 2021. A total of 30 individuals within the 25 - 65 age group were selected through convenient sampling and randomly divided into experimental and control groups (n = 15). The inclusion criteria were the ability to read and write, not being diagnosed with acute or chronic diseases, no neurological and psychological problems, substance abuse, age range between 25 - 65 years old, and visiting sexual health and psychological counseling centers in Tehran in 2021. The exclusion criterion was absence from more than two sessions.
3.2. Instrument
The international index of erectile function (IIEF): IIEF is a scale to measure sexual function in men. It was developed by Rosen et al. (24) and was validated in a group of men with erectile dysfunction. IIEF is one of the tools to measure the international index of erectile function. It comprises 15 items and evaluates erectile function in men in five fields, including erectile function, orgasmic function, sexual desire, intercourse satisfaction, and overall satisfaction. The questions are scored based on the 5-point Likert scale. In this study, the subscales of orgasmic function and overall satisfaction were examined. Babazadeh et al. (25) reported the reliability of this scale as equal to 0.73.
3.3. Intervention
Transcranial direct current stimulation (tDCS): This study used an Oasis/Pro device made in Canada. Since it operates with batteries, it was connected to two sensors or electrodes via wires. These electrodes are placed in a sponge cloth soaked in a water and salt solution (to make it more conductive) to boost electrical current conduction. This device has a small monitor that shows the power voltage, the required duration, and the treatment method. It can be adjusted manually. The device has feed-in and feed-out, which slowly increases the waves, and in the end, slowly decreases them to prevent dizziness in the patient. The treatment with this device is a technique in which the device generates low and stable direct electrical current on the skin through electrodes installed on different poles on the scalp. Its electrodes must be made of conductive plastics, soaked in sponges with a dimension of 6 × 8 cm, then placed in salt water to prevent chemical reactions between the skin and electrodes. Three types of electrodes include anodal, cathodal, and control. Anodal stimulation is positive stimulation that increases the capability of stimulating neurons. Cathodal stimulation reduces the stimulation of neurons, which is also used for cases of ADHD. A short stimulation is carried out in the control stimulation and then stopped. This type of stimulation is essential to examine the effect of anodal or cathodal stimulation.
3.4. Procedure
When the sample was determined due to the subject's sensitivity, a briefing was conducted for the participants to carry out the required arrangements. After the required explanations regarding the study's objective and research methodology, an informed letter of consent was obtained from the participants. After the briefing and obtaining the participants’ consent, the status of PE of all participants in both groups was measured by random selection (pretest). Then, the experimental group underwent tDCS for one month (8 sessions). The control group received no treatment plan during this time. After the completion of the intervention, the questionnaire was distributed among the experimental and control groups, and this variable was reexamined. Accordingly, the PE of participants was investigated after observing possible differences in the responses to the tDCS. After two months, a follow-up was carried out to examine the impact of time on the results.
3.5. Statistical Analyses
The research data were analyzed using the indices of mean and standard deviation at the descriptive level and through covariance analysis at the inferential level. The statistical data were analyzed in SPSS-23.
4. Results
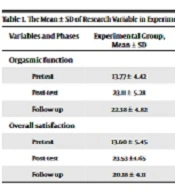
Table 1 shows the groups' mean and standard deviation (SD) of research variables separately. Accordingly, the mean of orgasmic function and overall satisfaction in men with sexual dysfunction in the experimental group was increased in the post-test and follow-up stages compared with the pretest stage.
| Variables and Phases | Experimental Group, Mean ± SD | Control Group, Mean ± SD |
|---|---|---|
| Orgasmic function | ||
| Pretest | 13.77 ± 4.42 | 14.68 ± 4.87 |
| Post-test | 23.11 ± 5.28 | 15.53 ± 4.83 |
| Follow-up | 22.38 ± 4.82 | 16.28 ± 5.36 |
| Overall satisfaction | ||
| Pretest | 13.60 ± 5.45 | 14.57 ± 5.89 |
| Post-test | 23.53 ±4.65 | 13.29 ± 4.77 |
| Follow-up | 20.18 ± 4.11 | 15.09 ± 5.85 |
The Mean ± SD of Research Variable in Experimental and Control Groups
Before the covariance (ANCOVA) analysis, the normality of the distribution of the scores was examined using the Shapiro-Wilk test, and variances were studied per Levene’s test. The results of the Shapiro-Wilk test on the subscales of orgasmic function and overall satisfaction manifested that the data follow a normal distribution. Furthermore, the assessment of the convergence of variance through Levene’s test concerning the subscales of orgasmic function and overall satisfaction demonstrated that the presumption of convergence of variance was observed. Considering the normality of data distribution, the ANCOVA was used. Following the results of Table 2, the experimental and control groups had a significant difference in the PE components, including orgasmic function and overall satisfaction (P < 0.001). Therefore, it can be argued that tDCS effectively treats PE in men with sexual dysfunction.
| Variables | SS | df | MS | F | P-Value | η2 |
|---|---|---|---|---|---|---|
| Orgasmic function | ||||||
| Time | 47.35 | 1 | 47.35 | 10.88 | < 0.001 | 0.41 |
| Group | 74.91 | 1 | 74.91 | 16.76 | < 0.001 | 0.66 |
| Error | 107.63 | 27 | 3.99 | |||
| Overall satisfaction | ||||||
| Time | 175.39 | 1 | 175.39 | 7.55 | < 0.001 | 0.14 |
| Group | 583.27 | 1 | 583.27 | 23.12 | < 0.001 | 0.68 |
| Error | 627.13 | 27 | 23.23 |
Results of Analysis of Covariance on Research Variables in Experimental and Control Groups in the Post-test Phase
As shown in Table 3, in the follow-up, the PE components, including orgasmic function (P = 0.032) and overall satisfaction (P = 0.027), were significantly different in the experimental and control groups. Thus, tDCS was effective in treating PE after two months.
| Variables | SS | df | MS | F | P-Value | η2 |
|---|---|---|---|---|---|---|
| Orgasmic function | ||||||
| Time | 40.15 | 1 | 40.15 | 8.42 | 0.044 | 0.39 |
| Group | 65.77 | 1 | 65.77 | 13.46 | 0.032 | 0.48 |
| Error | 96.23 | 27 | 3.56 | |||
| Overall satisfaction | ||||||
| Time | 163.21 | 1 | 163.21 | 5.77 | 0.025 | 0.32 |
| Group | 496.38 | 1 | 496.38 | 18.09 | 0.027 | 0.42 |
| Error | 525.74 | 27 | 19.47 |
Results of Analysis of Covariance on Research Variables in Experimental and Control Groups in the Follow-up Phase
5. Discussion
The present study aimed to investigate the effects of tDCS on the treatment of PE in men with sexual dysfunction in Tehran. The results suggested that tDCS improved orgasmic function and overall satisfaction in men with sexual dysfunction, and this effectiveness continued up to the follow-up stage. This finding is consistent with the findings of previous studies (26).
A disorder in any body part affects the overall system and other parts. Problems related to the brain, nerves, and nerve stimulation cause disorders in other organs, especially the reproductive system, which has a major relationship with the brain and nerves. The brain and the nervous system are the most sensitive areas in the human body; these special conditions need different treatment methods. According to researchers in the field, most internal diseases of the brain are related to the mental and psychological condition of the individuals (27). Sexual dysfunctions such as low sexual desire, frequency of sexual activity in both sexes and erectile dysfunction, and sexual and ejaculation dysfunction in men are called dyspareunia and inhibited orgasm (28). The nervous system creates a regular process between the brain, motor and sensory nerves, and reproductive system, and any disorder on this path can cause a problem. Per the results, tDCS was effective.
tDCS is a non-invasive method to stimulate the brain, in which the electrical current is used to influence the activity of the cerebral cortex. This method seeks to increase or decrease the activity of special areas in the brain and amplify or suppress special functions. This idea can provide new and interesting treatment methods for different diseases and even improve cognitive functions (18). Some initial evidence indicated that tDCS might influence the ability of individuals to learn new skills. For instance, in one study, tDCS improved number processing skills and other numerical abilities with lasting effects for six months after the initial treatment in individuals who tried to remember some symbols (29). Other similar studies have reported that when the primary motor cortex was stimulated with tDCS, it improved the ability to learn motor skills (30). It should be taken into account that sexual function as a skill can be affected by this method. In addition, the results of a study on people with insomnia suggested that using tDCS when sleeping can improve the "sleep efficiency" in these individuals. This means that this method reduced the duration of light-stage sleep and increased the duration of deep stages of sleep. It was specified that high sleep quality positively impacted sexual function (30).
This research had several limitations. The study's statistical population included men with PE who visited sexual health centers in Tehran. Thus, generalizing the results to other communities with different sociocultural structures should be cautiously done. The target group in this research was men with sexual dysfunction; therefore, the results cannot be generalized to women.
5.1. Conclusions
The results suggested that tDCS was influential in the treatment of PE in men with sexual dysfunction. Considering the effectiveness of tDCS in treating PE and increasing marital satisfaction, it is recommended to use this method to treat sexual dysfunction. In addition, it is recommended to teach this method to family and marriage counselors and psychologists to treat sexual dysfunctions using specialized methods. Since most of these individuals and medical specialists believe that drug therapy is the only treatment for PE, information regarding this non-drug treatment should be spread. Furthermore, to provide researchers with insight for future studies, it is recommended to conduct qualitative studies to learn the criteria for stopping PE. It is also recommended to carry out this research with other statistical populations in other metropolises since individuals' mindsets and physical and sexual status might be different in other cities.