1. Background
Most families experience a range of positive life events. However, in certain situations, families might encounter challenging periods, such as welcoming a child with special needs, impacting the family's dynamics (1). The birth of a child with mental, physical, or behavioral disabilities, or a combination thereof, significantly multiplies the psychological stress on family members, particularly the parents (2). Family members, especially mothers, endure considerable stress and mental strain due to the myriad issues associated with these children. Motherhood, inherently complex, becomes even more so and is filled with numerous negative emotions when it involves caring for a child with a disability. The care demands for children with intellectual disabilities are both physically and emotionally draining (3), and studies show that mothers of such children have a higher incidence of depression (4, 5).
Depression ranks as a leading cause of morbidity worldwide and stands as one of humanity's oldest known ailments. It is among the most prevalent mental disorders, incurring significant healthcare costs for individuals and society alike (6, 7). Research suggests that individuals with depression tend to view events through a pessimistic lens, focusing selectively on life's negative aspects (8). They dwell on stressful situations, shortcomings, and failures, blaming themselves for every occurrence and engaging in constant self-criticism (9). Given its destructive nature, depression has driven extensive research into its underlying causes (10). In this context, the ability of mothers of children with intellectual disabilities to manage their negative thoughts emerges as a critical factor influencing depression.
Managing negative thoughts involves strategies for coping with stressful situations or adverse events (11). Having children with mental and physical disabilities significantly contributes to the onset of negative thoughts, rumination, and depression among parents. Thus, parents, particularly mothers, can prevent the onset of further issues, including depression, by effectively managing their negative thoughts (12). To this end, five thought control strategies are identified: Distraction (intentionally redirecting attention away from a distressing thought towards another), worry (concentrating on and obsessing over a distressing thought), social control (discussing the thought with others), punishment (getting angry at oneself for contemplating the distressing subject), and re-appraisal (reassessing the meaning of the intrusive thought) (13).
Lifestyle is identified as another significant factor contributing to depression among mothers of children with intellectual disabilities (14). Generally, the health and advancement of any society rely greatly on the health of its women. Similarly, a mother's lifestyle profoundly affects the health of the mother-child relationship. Despite notable advancements in healthcare services for mothers and children, mothers of children with intellectual disabilities encounter numerous challenges that could affect their well-being (14). Overall, societal values and culture play a role in shaping perceptions of health, and the lifestyle of a society is partly shaped by its dominant culture (15). Both healthy and unhealthy lifestyles have their respective impacts on health, promoting and detracting from it (16). Several studies have established a connection between lifestyle and depression (17, 18).
Evidence indicates that the aforementioned variables-control over negative thoughts and lifestyle-directly influence depression among mothers of children with intellectual disabilities. This study aims to explore variables that could moderate the relationship between depression and both lifestyle and control over negative thoughts in these mothers. Social health is considered one of these mediating variables. Social health encompasses the ability to adapt to changes and adverse conditions, the successful operation of mental processes, effective activities, and productive interpersonal relationships (19). It involves the capacity to fulfill social roles effectively and efficiently without causing harm to others (20). Research by Eskandari et al. (18) has shown a significant negative correlation between social health and symptoms of depression.
The importance of this research stems from the understanding that the family is a social system where the dysfunction of any member can lead to additional problems. A child's disability is one such factor that impacts the family system, hindering family members from fulfilling their normal roles. Since support for families of children with intellectual disabilities has shown positive outcomes for the child, the family, and society at large, providing assistance to these families has become crucial in recent decades. Specialists have concentrated on the effects of children with intellectual disabilities on the family and their mutual interactions. The presence of a child with intellectual disabilities can cause marital strife, mental stress, significant financial burdens, and neglect of the needs of other family members. Contemporary evidence strongly supports this assertion. Addressing these issues is essential from a basic research perspective, as such investigations can lay the groundwork for applied research, potentially leading to effective strategies for reducing depression among mothers. Given the crucial role and influence of mothers in both family and societal development, and considering the challenges and stress associated with raising children with disabilities, it is vital to develop approaches to overcome the challenges faced by these mothers.
2. Objectives
This study sought to examine the mediating role of social health in the dynamics between depression, lifestyle, and control over negative thoughts among mothers of children with intellectual disabilities. The theoretical model of this research, as related to the stated objectives, is illustrated in Figure 1.
3. Methods
A descriptive correlational study was carried out, targeting all mothers of children with intellectual disabilities in Tehran in 2020. The study sample comprised 213 mothers. Inclusion criteria included written consent for participation, being aged between 27 and 50 years, and having at least a middle school diploma. Exclusion criteria were incomplete questionnaires and withdrawal from the study. The mothers completed various research questionnaires. In path analysis, the determination of the number of parameters is based on the count of direct paths, the tally of exogenous variables, and the enumeration of error variances. Furthermore, this study adhered to Kline's (21) guideline, which recommends a minimum of 15 participants per parameter to substantiate the model's validity, confirming the adequacy of the sample size for model testing.
3.1. Research Instruments
3.1.1. Beck's Depression Inventory
This study utilized the 13 item Beck Depression Inventory, which categorizes the severity of symptoms across a wide spectrum of scores, from neutral to extreme. Each item is scored on a scale from 0 to 3 (neutral to extreme) (22). Dadfar and Kalibatseva (23) found Beck's Depression Inventory to have an alpha Cronbach coefficient of 0.89. In our research, the Cronbach's alpha for this instrument was 0.85.
3.1.2. Thought Control Questionnaire
Developed by Wells and Davies (24), this 30 item questionnaire evaluates the differences in respondents' abilities to manage intrusive thoughts. It covers thought control strategies such as distraction, worry, social control, punishment, and re-appraisal. Each of its five subscales contains six items, answered on a four-point scale (almost always, often, sometimes, never) and scored from 4 to 1, respectively. Thus, total scores can range from 30 to 120. Darvish Molla et al. (25) reported an alpha Cronbach coefficient of 0.73 for the Thought Control Questionnaire. In our research, the reliability of this questionnaire was established at 0.79 using Cronbach's alpha. In our study, the reliability of the thought control questionnaire was 0.83 using Cronbach's alpha.
The Lifestyle Assessment Inventory, developed by Miller and Smith (26), comprises 20 items, each offering five response options: Always = 1, often = 2, sometimes = 3, rarely = 4, and never = 5. Higher scores indicate a less desirable and unhealthier lifestyle. Ghorbani Taghlidabad and Tasbihsazan Mashhadi (27) reported reliability of α = 0.85 for the Lifestyle Assessment Inventory. In this study, the reliability of the Lifestyle Assessment Inventory was determined to be 0.80 using Cronbach's alpha.
The Social well-being Scale, created by Keyes (28), contains 20 items that measure social integration, social acceptance, social contribution, social actualization, and social coherence. Responses are recorded on a four-point Likert scale, with participants indicating their level of agreement with each statement as follows: Strongly agree = 4, agree = 3, disagree = 2, and strongly disagree = 1. The total social health score can range from 20 (the lowest) to 80 (the highest), with scores classified into three categories reflecting low, medium, and high levels of social health. Shayeghian et al. (29) found the reliability of the Social Well-being Scale to be α = 0.72. In our study, the reliability of this instrument was 0.79, as measured by Cronbach's alpha.
3.2. Statistical Analyses
To investigate the relationships among the variables, Pearson's correlation coefficient and path analysis were utilized, employing AMOS-25 and SPSS v.27 software.
4. Results
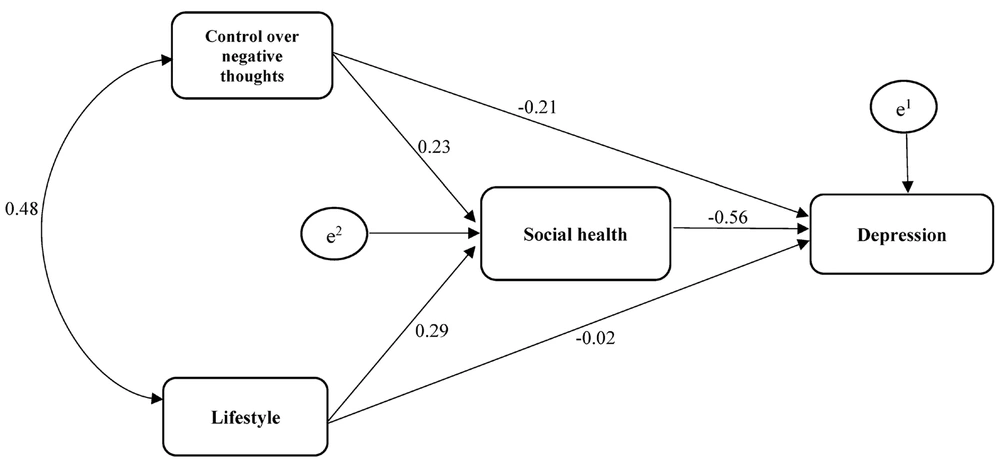
The average age of the mothers was 31.15 years, with a standard deviation of 4.07. Table 1 provides descriptive statistics, including means and standard deviations. The assumption of data normality was evaluated through skewness and kurtosis values, as shown in Table 1. Given that all referenced statistics are within the range of -2 to 2, the data distribution's normality assumption was confirmed. Results from the Pearson correlation coefficient, detailed in Table 2, indicated a significant correlation among all research variables (P < 0.01). Figure 2 illustrates the initial model that delineates the impact of the ability to control negative thoughts, lifestyle, and social health on depression.
| Variables | Mean | SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Depression | 16.14 | 7.96 | 0.76 | 0.98 |
| Control over negative thoughts | 72.49 | 18.51 | -0.28 | -0.62 |
| Lifestyle | 62.31 | 17.73 | 0.18 | -0.67 |
| Social health | 46.06 | 14.56 | 1.06 | -0.84 |
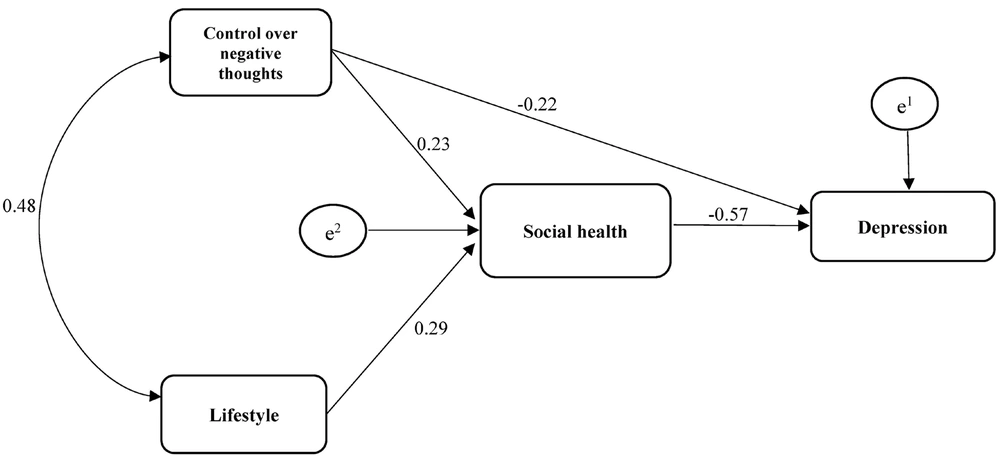
The data shown in Table 3 reveal that the root mean square error of approximation (RMSEA) value of 0.424 suggests the need for modifications to the initial model. This initial model was characterized by saturation, with all potential paths included, which precluded the computation of metrics like chi-square. However, eliminating the path from lifestyle to depression alleviated the model's saturation, enabling the calculation of indicators such as the coefficient of determination using the software. The final model achieved an RMSEA value of 0.001, signifying a well-fitting model. Figure 3 displays the adjusted model.
| Fit indicators | χ2 | df | (χ2/df) | RFI | IFI | TLI | CFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|
| Initial model | - | - | - | - | - | - | - | 0.424 | |
| Revised model | 0.095 | 1 | 0.095 | 0.99 | 0.99 | 0.99 | 0.99 | 0.99 | 0.001 |
Table 4 presents the estimated path coefficients for evaluating the direct and indirect hypotheses. The findings indicate a direct and negative correlation between control over negative thoughts and depression (β = -0.22, P < 0.001) and between social health and depression (β = -0.57, P < 0.001) among mothers of children with intellectual disabilities. Additionally, a positive and significant association was observed between control over negative thoughts and social health (β = 0.23, P < 0.001), and between lifestyle and social health (β = 0.29, P< 0.001), in these mothers. Table 4 also reveals no significant correlation between lifestyle and depression (β = -0.02, P < 0.758). Furthermore, Table 4 highlights a significant indirect correlation between control over negative thoughts and depression, with social health serving as a mediator. Similarly, the link between lifestyle and depression, mediated by social health, was found to be significant (P < 0.001).
| Paths | Revised Model | |
|---|---|---|
| β | P | |
| Control over negative thoughts → depression | -0.22 | 0.001 |
| Lifestyle → depression | -0.02 | 0.758 |
| Control over negative thoughts → social health | 0.23 | 0.001 |
| Lifestyle → social health | 0.29 | 0.001 |
| Social health → depression | -0.57 | 0.001 |
| Control over negative thoughts → depression through social health | -0.09 | 0.001 |
| Lifestyle → depression through social health | -0.12 | 0.001 |
5. Discussion
This study sought to explore the mediating role of social health in the dynamics between depression, lifestyle, and control over negative thoughts among mothers of children with intellectual disabilities. The findings revealed a negative correlation between control over negative thoughts and depression among these mothers, aligning with the research by Spinhoven et al. (30). The presence of children with disorders or disabilities can adversely affect the marital relationships of parents, especially mothers who spend a considerable amount of time with their children. Such circumstances may also precipitate the onset of mental disorders, like depression, in mothers of children with intellectual disabilities. Research indicates that poor marital functioning adversely affects the physical and mental well-being of mothers (31). Moreover, marital dissatisfaction greatly heightens the risk of divorce among mothers of children with intellectual disabilities. Should parents fail to manage their worries and negative thoughts effectively, they might internalize guilt over their child's condition, leading to rumination. This, in turn, could strain the marital relationship, disrupt family dynamics, and contribute to parental depression (5). It can be argued that mothers who strategically manage and exert control over negative thoughts tend to be more content and lead more fulfilling lives. Furthermore, the discourse on controlling negative thoughts is based on the notion that managing negative thinking is key to building self-esteem, personal efficacy, and individuality. Addressing these factors can enhance positive thinking while mitigating negative thoughts and depression, thereby fostering an individual's overall happiness and life satisfaction.
Furthermore, the study found no significant or positive correlation between lifestyle and depression, a conclusion that diverges from the findings of van Lee et al. (17). In prior research, the relationship between control over negative thoughts and depression was examined through correlation and regression analyses, revealing a significant association. However, this study applied structural equation modeling to incorporate the mediating variable, rendering the direct link between control of negative thoughts and depression as not significant. Yet, with social health serving as a mediator, the indirect relationship between lifestyle and depression became noteworthy. In other words, control over negative thoughts indirectly influences depression through social health. A proper lifestyle enhances family functioning and the mental health of mothers, with those maintaining a healthy lifestyle making superior choices regarding nutrition, attire, and physical activity. When mothers maintain robust physical and mental health, their energy positively influences other family members, safeguarding against mental disorders and depression. The negative effects of having a child with an intellectual disability are mitigated under these conditions. Lifestyle also plays a role in shaping interpersonal relationships during times of distress and challenges. Moreover, improving one's state of consciousness, transcendental awareness, and critical thinking can have a beneficial effect on psychological well-being. This is attributed to the way lifestyle provides a framework for identifying and organizing essential qualities such as skills, capabilities, and a set of necessary values and beliefs, which in turn can influence depressive symptoms (17).
Another significant outcome of this study is the direct relationship between social health and depression, aligning with Eskandari et al.’s findings (18). The challenging conditions arising from caring for a child with an intellectual disability can lead to depression and other mental health issues for mothers. In such contexts, social support plays a crucial role in mitigating psychological harm due to its positive impact on mental well-being (32). Emotional self-regulation allows individuals to manage their feelings and how they express emotions. Seen as a cognitive strategy for regulating emotions, self-blame, or attributing blame externally, mirrors attributional styles, which tend to be more pervasive, fixed, and internally directed. Cognitive strategies for emotion regulation are crucial for managing arousal and negative emotions (18), and are associated with the emergence or presence of mental health issues. Studies have shown that individuals with high scores on depression scales often have poorer social and psychological health (4). Conversely, those with lower depression scores utilize a variety of coping mechanisms in stressful situations, including seeking social support, applying constructive criticism, and implementing self-control and problem-solving techniques. Consequently, it can be inferred that the presence of social health in mothers correlates with lower levels of depression.
The analysis of indirect paths uncovered an indirect link between control over negative thoughts and depression, moderated by social health. Furthermore, social health was found to mediate the relationship between lifestyle and depression, a finding for which there are no directly comparable studies. The direct paths examined revealed that social health moderates the relationship between control over negative thoughts, lifestyle, and depression. With the presence of a child with an intellectual disability, it is reasonable to anticipate that the child's condition will impact the family, exacerbating the challenges faced by parents, especially mothers. The occurrence of disabilities and disorders in children is widely acknowledged as a significant factor in fostering negative thoughts and self-blame among parents. If parents can practice empathy and manage their negative thoughts effectively, they are likely to experience increased intimacy and closeness with each other, enhancing marital satisfaction. This, in turn, can lead to a decrease in depression and other related disorders. Moreover, a healthy lifestyle among mothers contributes to better physical health, which influences their social health, quality of life, and levels of depression.
As a limitation, this study acknowledges that various factors, such as the number of children, the mothers' employment status, and economic conditions, could have influenced its outcomes. The research sample consisted of mothers of children with intellectual disabilities in Tehran, which necessitates caution in extending the findings to other populations and cultural contexts. Additionally, the study may not have fully accounted for confounding variables like marital conflict and marital burnout, which could affect mothers' social health. Therefore, further research involving diverse samples is recommended to validate the findings more broadly.
5.1. Conclusions
The study found that control over negative thoughts and lifestyle was inversely related to depression among mothers of children with intellectual disabilities. The revised model demonstrated a good fit, suggesting its potential utility in creating programs aimed at alleviating the stress faced by these parents and mitigating their depression. Moreover, the results highlight the importance of increased professional support and the development of psychological and social assistance programs for mothers with children who have intellectual disabilities. Based on these insights, we recommend the implementation of psychotherapy programs focused on enhancing lifestyle and bolstering control over negative thoughts for mothers of children with intellectual disabilities.