1. Background
Cesarean section, commonly referred to as a C-section, is a surgical procedure in which a baby is delivered through an incision made in the mother's abdomen and uterus, typically when vaginal delivery is deemed unsafe or not feasible for both the mother and the baby (1). The choice between general anesthesia and regional anesthesia for a cesarean section depends on the patient's clinical condition and whether the surgery is elective or an emergency (2). While neuraxial anesthesia (spinal and epidural anesthesia) is considered the gold standard for cesarean sections, general anesthesia is still used, particularly in cases where regional anesthesia is contraindicated or unsuccessful (1, 3). General anesthesia is often preferred in emergencies, such as in cases of fetal distress during pregnancy, as it allows for rapid induction (4).
Contraindications for regional anesthesia include conditions such as increased intracranial pressure, hypovolemic shock, sepsis, coagulation disorders, uterine atony, infection or inflammation at the injection site, severe mitral valve stenosis, and a high risk of severe bleeding (2). Additionally, the hypotension associated with regional anesthesia may affect short-term neonatal outcomes (5). Cesarean sections under general anesthesia offer advantages, including rapid induction, optimal control of the airway, and a reduced risk of hypotension and cardiovascular instability, especially in cases such as preeclampsia with neurological complications (2).
The World Health Organization recommends an ideal cesarean section rate of 10 - 15% (5). However, the prevalence of cesarean sections, particularly in Iran, exceeds this recommended rate, posing significant challenges (6). Cesarean sections are considered life-saving surgical procedures for both the mother and child, with studies estimating their role in preventing a substantial number of maternal and neonatal deaths annually (7). Therefore, anesthesia management during cesarean sections is critical for ensuring the safety of both the newborn and the mother (7).
Due to emergency conditions and time constraints, general anesthesia is often more commonly used than regional anesthesia (8). The choice of anesthesia technique depends on several factors, including the patient's physiological condition, the physician's expertise, and the availability of drugs and medical equipment (7). Spinal anesthesia is frequently preferred for cesarean sections due to its advantages, such as reduced complications associated with general anesthesia and enhanced maternal-fetal bonding (9). However, spinal anesthesia can also lead to side effects like arterial hypotension and fetal distress (10).
General anesthesia involves the administration of intravenous or inhalation anesthetics, while spinal anesthesia requires the injection of a local anesthetic into the subarachnoid space (11). Both methods have associated risks and side effects. Given recent case reports and the preference for general anesthesia over regional anesthesia in certain situations, this study aims to conduct a randomized clinical trial to compare the hemodynamic parameters and fetal outcomes during cesarean sections performed under spinal versus general anesthesia (2, 3).
2. Objectives
This study aims to compare hemodynamic parameters, intraoperative bleeding, blood pressure, postoperative pain, and neonatal outcomes during and after cesarean section in term, singleton pregnancies without complications, performed under spinal and general anesthesia.
3. Methods
This study was a randomized controlled clinical trial with two groups: An intervention group that received spinal anesthesia and a control group that received general anesthesia for elective cesarean section. The study was conducted at Fatemieh Hospital in Hamadan, following ethical approval and informed consent from the participants. Ethical considerations outlined in the Declaration of Helsinki were strictly adhered to throughout the study.
3.1. Participants
The study sample consisted of 62 candidates scheduled for elective cesarean section. Two participants were excluded from the study, leaving 30 participants in each group. Data collection included fieldwork and the completion of a demographic information questionnaire, which gathered details such as age, hospitalization history, and education level.
3.2. Measurement Methods
Intraoperative bleeding was quantified by weighing blood-contaminated gauzes, with each gram of gauze weight considered equivalent to one milliliter of blood loss. Additionally, the volume of blood in the suction reservoir was measured after subtracting wash fluids and amniotic fluid (12). Pain intensity during the first 24 hours post-operation was evaluated using the Numeric Rating Scale (NRS) (13). Blood pressure was monitored using a manometer within the first 24 hours post-surgery. The Apgar scale was used to assess newborns' Apgar scores at the first and fifth minute after delivery. This scale evaluates five parameters: Appearance (skin color), pulse (heart rate), reflex response, activity (muscle tone), and respiration (respiratory rate and effort). Each parameter is scored from 0 to 2, yielding a total score between 0 and 10. A score of 7 or higher at 1 minute indicates good health, while a score below 7 may require immediate medical attention. A 5-minute score below 7 may indicate an increased risk of mortality or cerebral palsy (14, 15). Pain intensity was assessed on a scale of 0 to 10, with higher scores indicating greater pain (16). The average pain intensity was recorded using the NRS pain intensity scale at 0, 6, 12, 18, and 24 hours post-admission. Blood pressure was also monitored at various intervals following admission to the ward: Upon admission, and at 2, 4, 6, 12, and 24 hours thereafter.
3.3. Inclusion and Exclusion Criteria
3.3.1. Inclusion Criteria
- Pregnant women aged between 18 and 40 years.
- Absence of a history of hypertension.
- No history of coagulation disorders.
- Newborn birth weight between 2.5 to 3.8 kilograms, with full-term infants.
- Hemoglobin level of at least 90 grams per liter in patients.
- Categorization of patients according to the American Society of Anesthesiologists (ASA) as class 1 or class 2 in physical status (17).
- Informed consent obtained for participation in the study.
3.3.2. Exclusion Criteria
- Need for an emergency cesarean section.
- History of maternal stillbirth.
- Multiple pregnancies.
- Presence of chromosomal abnormalities.
- Need for a pain pump.
- Presence of polyhydramnios.
Considering a confidence level of 95% and a power of 8%, the sample size was calculated to be 28 participants in each group. Taking into account a 10% dropout probability, the final number of participants was determined to be 31 in each group (18).
3.4. Data Collection Tools
The data collection in this study comprises four parts:
Numeric Rating Scale criteria: In this method, individuals rate their pain on a scale from zero to ten. Zero represents no pain, 1 to 3 indicates mild pain, 4 to 6 represents moderate pain, and 7 to 10 indicates severe pain. According to previous studies, this scale demonstrates good validity and reliability.
Measurement of bleeding: The volume of blood loss was estimated by measuring the amount of blood-contaminated gauze and the volume of blood in the suction reservoir.
Blood pressure monitoring: Continuous monitoring of the patient's blood pressure was conducted for the first 24 hours after surgery using a monitor and manometer. Blood pressure measurements were taken upon admission to the ward and at 2, 4, 6, 12, and 24 hours after admission, and recorded.
Apgar Scale: The Apgar scale was used to assess the effects of anesthesia on the newborn (19). The Apgar score consists of five ordinal qualitative variables, each assigned a numerical value ranging from zero to two, which are then summed together to create a continuous quantitative variable (20).
In the general anesthesia group, after 5 minutes of preoxygenation with a mask, anesthesia induction was performed using thiopental sodium at a dose of 3 mg/kg and succinylcholine at a dose of 1.5 mg/kg. Endotracheal intubation was performed using a size 7.5 or 7 endotracheal tube. After clamping of the umbilical cord, intravenous fentanyl at a dose of 2 μg/kg and atracurium at a dose of 0.5 mg/kg were administered for intraoperative pain management and muscle relaxation, respectively. Neostigmine at a dose of 0.05 mg/kg and atropine at a dose of 0.01 mg/kg were administered to reverse the effects of atracurium.
In the spinal anesthesia group, after skin preparation and sterile draping in the sitting position, a 25-gauge needle was inserted into the L3-4 or L4-5 space. Upon observing cerebrospinal fluid, 2.2 mm of hyperbaric bupivacaine 0.5% at a speed of 0.2 mm/s was injected into the subarachnoid space. Ephedrine was used to manage hypotension during the procedure. Additionally, 3 mm of intravenous fentanyl were administered to the spinal anesthesia group to provide longer-lasting pain relief and reduce postoperative nausea and vomiting (21).
The duration of surgery in both groups was 30 minutes, and 50 units of oxytocin, equivalent to 5 mm, were administered intravenously in both groups.
3.5. Statistical Method
Data analysis was conducted using SPSS version 16 software, with a significance level set at 0.05. Initially, the assumption of normality for the data was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. In cases where the data did not meet the normality assumption, non-parametric equivalents were used. Descriptive statistics, including frequency, percentage, mean, and standard deviation, were calculated. Analytical statistics involved the use of chi-square tests and independent t-tests.
4. Results
A total of 60 patients were included in the study and divided into two groups of 30 each, based on the method of anesthesia: General anesthesia and spinal anesthesia. The most common indication for cesarean section across both groups was a previous cesarean section, accounting for 55% of all patients. The demographic characteristics of the mothers in both groups are summarized in Tables 1-3.
a Values are expressed as No. (%) unless otherwise indicated.
| Variables and Groups | Mean ± Standard Deviation | F | t | Mean Difference | P-Value |
|---|---|---|---|---|---|
| Operation bloodless | 3.981 | 0.190 | 6.16 | 0.85 | |
| Spinal anesthesia | 451.66 ± 146.90 | ||||
| General anesthesia | 445.50 ± 100.57 | ||||
| Apgar score in the first minute after birth | 4.391 | 1.000 | 0.03 | 0.85 | |
| Spinal anesthesia | 9.00 ± 0.00 | ||||
| General anesthesia | 8.96 ± 0.18 | ||||
| Apgar scored in the fifth minute after the birth | 4.291 | 1.000 | 0.03 | 0.32 | |
| Spinal anesthesia | 10.00 ± 0.00 | ||||
| General anesthesia | 9.96 ± 0.18 |
The mean age of participants in the spinal anesthesia group was 32 years [standard deviation (SD) = 3.5], while in the general anesthesia group, the mean age was 34 years (SD = 3.6). Results from the independent t-test indicated that the age difference between the two groups was not statistically significant (P > 0.05). The frequency of patients with a history of hospitalization was 19 (63.3%) in the spinal anesthesia group and 22 (73.3%) in the general anesthesia group. According to the chi-square test, there was no significant difference in hospitalization history between the two groups (P > 0.05).
In terms of educational level distribution, 14 individuals (46.7%) in both groups had a bachelor's degree. In the spinal anesthesia group, 7 individuals (23.3%) held a diploma, and 9 individuals (30%) had less than a diploma. In the general anesthesia group, 8 individuals (26.7%) held a diploma, and another 8 (26.7%) had less than a diploma. The chi-square test results showed no significant difference in educational level distribution between the two groups (P > 0.05).
Using an independent t-test, the amount of intraoperative bleeding and the Apgar scores of newborns at the first and fifth minutes after birth were compared between the spinal anesthesia and general anesthesia groups. The results are presented in Table 3. It was observed that the amount of bleeding during surgery was slightly higher in the general anesthesia group compared to the spinal anesthesia group. However, the results of the independent t-test indicated that this difference was not statistically significant (P = 0.85).
Regarding the Apgar scores at the first and fifth minutes after birth, the values in the spinal anesthesia group were slightly higher than those in the general anesthesia group. Nevertheless, the independent t-test results showed no statistically significant difference between the two groups in terms of Apgar scores at the first and fifth minutes (P = 0.32).
These findings suggest that the use of spinal anesthesia, compared to general anesthesia, did not significantly affect the amount of intraoperative bleeding or the Apgar scores of newborns at the first and fifth minutes after birth.
Using an independent t-test, the pain levels were compared between the spinal anesthesia and general anesthesia groups at the time of admission, every 6 hours, at 12 hours, 18 hours, and 24 hours post-operation. The results are presented in Table 4. As observed, the mean pain score in the general anesthesia group was consistently higher than in the spinal anesthesia group at all assessment stages. The results of this test demonstrated that the difference between the two groups was statistically significant (P = 0.001).
| Variables and Groups | Mean ± Standard Deviation | F | t | Mean Difference | P-Value |
|---|---|---|---|---|---|
| Pain level at the moment of entering the ward | 3.16 | -6.179 | 1.36 | 0.001 | |
| Spinal anesthesia | 6.73 ± 0.96 | ||||
| General anesthesia | 8.10 ± 0.75 | ||||
| Pain level 6 hours after the operation | 0.987 | -6.406 | 1.23 | 0.001 | |
| Spinal anesthesia | 5.20 ± 0.99 | ||||
| General anesthesia | 6.43 ± 1.16 | ||||
| Pain level 12 hours after the operation | 1.841 | -3.420 | 1.16 | 0.001 | |
| Spinal anesthesia | 4.26 ± 1.20 | ||||
| General anesthesia | 5.43 ± 1.43 | ||||
| Pain level 18 hours after the operation | 39.472 | -4.702 | 1.43 | 0.001 | |
| Spinal anesthesia | 2.93 ± 0.63 | ||||
| General anesthesia | 6.35 ± 1.54 | ||||
| Pain level 24 hours after the operation | 3.185 | -5.869 | 1.50 | 0.001 | |
| Spinal anesthesia | 1.66 ± 0.85 | ||||
| General anesthesia | 3.16 ± 1.14 |
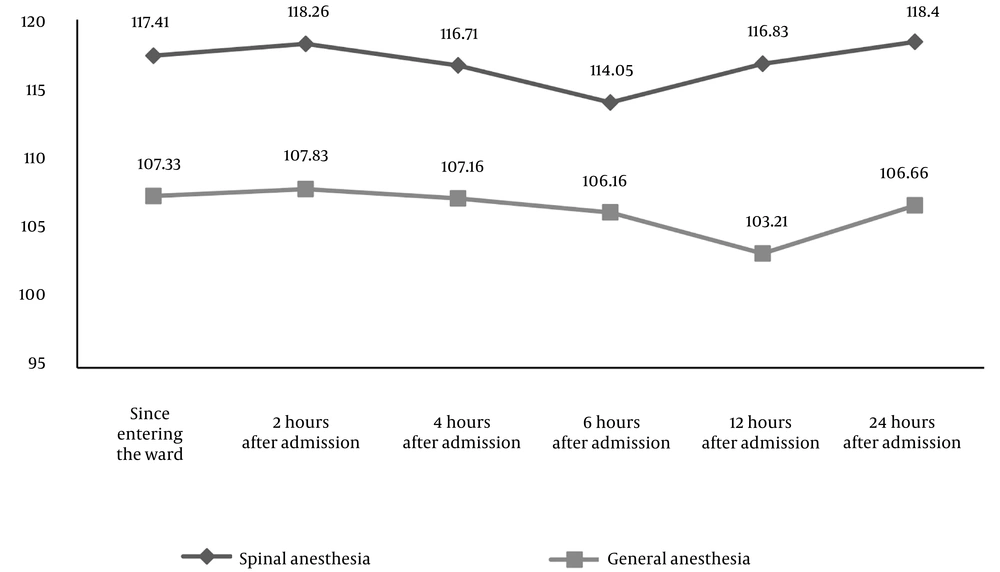
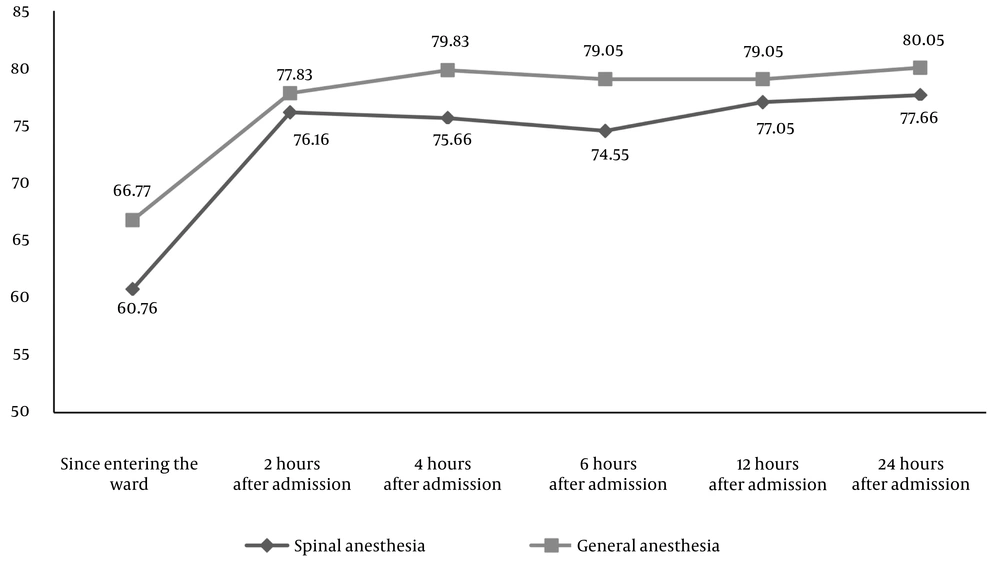
As evident from Figures 1 and 2, blood pressure at various measured times did not follow a consistent trend. For instance, upon admission to the ward, the mean systolic and diastolic blood pressures were 117/76 millimeters of mercury (mmHg) and 60/76 mmHg, respectively. Two hours post-admission, these values increased slightly to 118/76 mmHg and 26/76 mmHg, respectively. However, at 4 hours post-admission, systolic and diastolic blood pressures decreased to 116/75 mmHg and 70/75 mmHg, respectively, compared to two hours earlier and upon admission. Similarly, at the final measurement (24 hours post-admission), the mean systolic and diastolic blood pressures were 118/77 mmHg. Overall, the highest and lowest systolic blood pressure values were recorded at 24 hours post-admission (118/40 mmHg) and 6 hours post-admission (114/05 mmHg), respectively. Regarding diastolic blood pressure, the highest and lowest values were recorded at the same time points (24 hours and 6 hours post-admission), at 77/66 mmHg and 74/55 mmHg, respectively.
Using an independent t-test, blood pressure levels at admission and at 2, 4, 6, 12, and 24 hours post-admission were compared between the spinal anesthesia and general anesthesia groups. The results are depicted in Figures 1 and 2. Overall, systolic blood pressure in the spinal anesthesia group was higher than in the general anesthesia group. Conversely, diastolic blood pressure in the general anesthesia group was higher than in the spinal anesthesia group at all measurement stages. The independent t-test results showed that the difference in systolic blood pressure between the two groups was significant for all measurements (P < 0.05), while for diastolic blood pressure, the difference between the spinal anesthesia and general anesthesia groups was not significant at certain time points (2 hours, 6 hours, and 12 hours post-admission) (P > 0.05).
5. Discussion
We conducted this study on selected cesarean sections to compare two types of anesthesia. No statistically significant differences were found between the two groups regarding age, previous hospitalization history, or maternal education level, which enhances the reliability of our study results. Regarding bleeding, our results indicate that cesarean sections performed under general anesthesia tend to have slightly more bleeding compared to those performed under spinal anesthesia. The mean blood loss during surgery in patients under general anesthesia was higher than in those under spinal anesthesia; however, this difference was not statistically significant.
In this study, blood loss was measured based on the volume of blood-contaminated gauzes and the contents of the suction canister, with deductions made for amniotic fluid and irrigation fluids, rather than using a specific method to estimate blood loss. Multiple studies have demonstrated that cesarean deliveries under general anesthesia result in greater blood loss compared to those under regional anesthesia (22). In a prospective randomized study on selected cesarean cases, the average hemoglobin level in women under general anesthesia decreased by 1.1 g/dL compared to spinal anesthesia, which is consistent with our findings (23). It has been suggested that the increased blood loss under general anesthesia may be due to the effects of uterine muscle relaxants, which are not used in spinal anesthesia, leading to more bleeding in general anesthesia cases (24).
In surgeries where uterine contractions are not a factor, such as pelvic surgeries and hysterectomies, lower blood loss has been reported in the regional anesthesia group compared to the general anesthesia group (25), likely due to the vasodilatory effects of the anesthetic gases used in general anesthesia. In contrast, a study by Al-Husban et al. found that the estimated blood loss was lower in the general anesthesia group compared to spinal anesthesia, which contradicts our results. This difference may be due to the retrospective nature of their study and associated bias (26). However, in a study by Aksoy et al., which compared hemoglobin and hematocrit levels before and after surgery in a prospective study on selected cesareans, they concluded that blood loss was higher in the general anesthesia group compared to the spinal anesthesia group (23), a finding that aligns with our study due to the similarity of the study populations.
Regarding postoperative pain, our study shows that patients undergoing cesarean sections under general anesthesia experience more pain compared to those under spinal anesthesia. This is because neuraxial anesthesia (spinal) is superior to injectable and systemic analgesia for pain relief (22). Additionally, neuraxial analgesia is associated with earlier bowel function recovery, earlier mobilization, and shorter hospital stays compared to systemic analgesia (27). Studies have demonstrated that post-cesarean pain is greater in patients who underwent general anesthesia compared to spinal anesthesia, which aligns with our findings (22). This is likely due to the longer duration of action of intrathecal spinal medications compared to the intravenous opioids used in general anesthesia, as well as the use of intravenous fentanyl in the spinal anesthesia group in our study. Previous cesarean section experiences may have also influenced the results.
Postoperative blood pressure drops are among the risk factors for postoperative shivering and can increase the risk of wound infection, oxygen consumption, and patient discomfort. Therefore, blood pressure management is a critical factor. Our study found that systolic blood pressure was higher in the spinal anesthesia group compared to the general anesthesia group, while diastolic blood pressure was higher in the general anesthesia group at some postoperative hours. This may be due to the effects of adrenaline administered during spinal anesthesia and the volume of intraoperative fluids in the general anesthesia group, findings that are consistent with the study by Karami et al. (28). Chen et al. concluded that, in terms of hemodynamic parameters, general anesthesia is superior to spinal anesthesia, which somewhat aligns with our results, possibly due to better blood pressure management during surgery and the performance of systemic and intravenous anesthesia drugs (17).
Moreover, there was no statistically significant difference in Apgar scores at 1 and 5 minutes between the two groups (29). Data analysis by Cochrane supports this finding, indicating that there is no significant difference not only in terms of the mean Apgar score at the first and fifth minutes but also in the need for neonatal oxygen between the two groups (30). In contrast, a study by Gwanzura et al. found that the Apgar score was higher in the spinal anesthesia group compared to the general anesthesia group, which contradicts our findings (31). This discrepancy may be attributed to various factors, such as the significantly larger sample size in their study compared to ours. Additionally, our study focused exclusively on elective cesarean sections. Similarly, in the study by Al-Husban et al., no significant difference in Apgar scores between the spinal and general anesthesia groups was observed, which is consistent with our results (26).
One of the strengths of this study is the randomization process used to allocate participants to different treatment groups without bias, ensuring that patients were randomly assigned to receive either general or spinal anesthesia for their cesarean section. Additionally, the duration of surgery and the amount of oxytocin administered were standardized across both groups. However, a limitation of our study is the lack of homogeneity in the samples concerning body mass index (BMI), as the study by Zandi et al. found a correlation between BMI and blood loss (32). Other limitations include the small sample size, partly due to maternal dissatisfaction with early maternal-neonatal communication in the spinal anesthesia method, as well as concerns such as depression in infants born under general anesthesia and the risk of maternal aspiration (33, 34). Furthermore, most participants in this study had prior cesarean section experiences, which may have served as a confounding factor in pain perception. Lastly, only elective cesarean sections were investigated. It is hoped that future studies will conduct more comprehensive investigations into variables such as cognitive dysfunction in mothers post-surgery to provide more accurate comparisons between these two anesthesia techniques.
5.1. Conclusions
In this study, systolic blood pressure after childbirth was found to be higher in women undergoing spinal anesthesia, while diastolic blood pressure was higher in women receiving general anesthesia. Additionally, the amount of intraoperative bleeding was greater in the general anesthesia group compared to the spinal anesthesia group. Postoperative pain was reported to be less in the spinal anesthesia group than in the general anesthesia group. There was no statistically significant difference in Apgar scores at 1 and 5 minutes between the two groups. Therefore, regional anesthesia emerged as the preferable option for elective cesarean sections, based on both hemodynamic parameters and pain assessment. The advantages of regional anesthesia for maternal and fetal outcomes were found to be superior to those of general anesthesia.