1. Background
The intensive care unit (ICU) is where patients with life-threatening conditions are managed. According to the Intensive Care Audit of Countries (ICON), the probability of death is statistically correlated with the income level of each country. Developing quality indicators, conducting audits, making necessary adjustments, and monitoring resources should all be required to ensure high-quality care (1, 2). A lack of essential resources, such as personnel, equipment, drugs, and supplies, as well as factors like infection, trauma, and patients’ co-morbidities, contribute to higher ICU mortality rates. Several factors have a direct impact on treatment success and mortality rates in the ICU (3-5). A recent systematic review concluded that the high ICU mortality rates reported during the COVID-19 pandemic were largely due to the rationing of resources in overwhelmed hospitals (6).
Identifying the factors associated with increased ICU mortality will help to improve the management of critically ill patients. Since the quality of ICU care varies, and the findings of other research cannot always be generalized, it is essential for each center to be aware of its own situation. As no similar research has been conducted in Guilan province, this study was designed. The aim of the study is to assess the prevalence and variables associated with ICU mortality among patients admitted to the general ICU in an academic referral hospital in Guilan, northern Iran.
2. Objectives
This study aimed to assess the prevalence and variables associated with the mortality rate among patients admitted to the general intensive care unit (GICU) in an academic referral hospital in Guilan, northern Iran.
3. Methods
This single-centered retrospective study was conducted at the General ICU of Poorsina Hospital, an academic comprehensive specialized hospital affiliated with Guilan University of Medical Sciences (GUMS), from 2019 to 2023. The ICU consists of 23 functional beds and mechanical ventilators. Data were collected using a structured checklist that included patients' socio-demographic characteristics, diagnosis at admission, presence of comorbidities, length of stay, and outcomes.
3.1. Verifiable Variables
The dependent variable in this study was ICU mortality, while the independent variables included age, sex, residency, marital status, and various comorbidities such as cancer, cardiac illness, hypertension, diabetes mellitus (DM), asthma, and chronic obstructive pulmonary disease (COPD). Additionally, the Glasgow Coma Scale (GCS) score, which evaluates ocular, verbal, and motor responses, was considered. The GCS scores were categorized as mild (GCS 13 - 15), moderate (GCS 9 - 12), and severe (GCS ≤ 8). Other independent variables included the number of days on mechanical ventilation (MV), the length of ICU stay, and the reasons for ICU admission. Based on the main outcome, either death or discharge, the patients were divided into two groups.
3.2. Statistical Analysis
Data analysis was conducted using SPSS version 22 (SPSS Inc., Chicago, IL). Continuous variables were expressed as means ± standard deviation, and categorical variables were described in terms of absolute and relative frequencies. Fisher’s exact test, t-test, and chi-square test were used for analysis. To identify variables independently associated with mortality, multivariate logistic regression was performed. A significance level of less than 0.05 was considered statistically significant.
3.3. Ethics Considerations
This study was approved by the Ethics Committee in Research of GUMS under the ethics code IR.GUMS.REC.1402.357.
4. Results
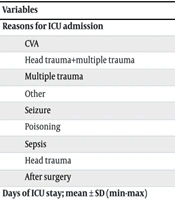
Out of the 8,650 admitted patients, 62.8% were discharged, while 37.2% died. The average age of the patients was 53.2 ± 23.27 years, and 63.1% were men. Additionally, 64.3% of the patients resided in urban areas, 68.5% were married, and 57.5% had comorbidities. The average length of stay in the ICU was 4.82 ± 7.65 days. The demographic data of the patients and reasons for admission are shown in Tables 1 and 2. Comparisons between the death and discharge groups are presented in Tables 3 and 4.
| Variables | No. (%) |
|---|---|
| Gender | |
| Man | 5461 (63.1) |
| Female | 3189 (36.9) |
| Age (y) mean ± SD (min-max) | 53.2 ± 23.27 (1 - 107) |
| Less than 20 | 842 (9.7) |
| 21 - 40 | 2048 (23.7) |
| 41 - 60 | 1969 (22.8) |
| 61 - 80 | 2717 (31.4) |
| More than 80 | 1074 (12.4) |
| Residency | |
| Urban | 5560 (64.3) |
| Rural | 3090 (35.7) |
| Marital status | |
| Single | 2725 (31.5) |
| Married | 5925 (68.5) |
| Co-morbidities | |
| Yes | 4972 (57.5) |
| No | 3678 (42.5) |
| GCS | |
| 3 - 5 | 1499 (17.3) |
| 6 - 8 | 1193 (13.8) |
| 9 - 12 | 2682 (31) |
| 12 - 15 | 3276 (37.9) |
Abbreviation: GCS, Glasgow Coma Scale.
| Variables | No. (%) |
|---|---|
| Reasons for ICU admission | |
| CVA | 2259 (26.1) |
| Head trauma+multiple trauma | 2003 (23.2) |
| Multiple trauma | 1671 (19.3) |
| Other | 772 (8.9) |
| Seizure | 675 (7.8) |
| Poisoning | 483 (5.6) |
| Sepsis | 427 (4.9) |
| Head trauma | 221 (2.6) |
| After surgery | 139 (1.6) |
| Days of ICU stay; mean ± SD (min-max) | 4.82 ± 7.65 (1 - 68) |
| 1 day | 4096 (47) |
| 2 - 3 days | 1766 (20.4) |
| 4 - 7 day | 1418 (16.4) |
| More than 7 days | 1397 (16.2) |
| Days of MV; mean ± SD (min-max) | 2.5 ± 6.8 (0 - 60) |
| No MV | 5407 (62.5) |
| 1 day | 1407 (16.3) |
| 2 - 3 days | 579 (6.7) |
| 4 - 7 days | 476 (5.5) |
| More than 7 days | 781 (9) |
Abbreviations: CVA, cerebral vascular accident; MV, mechanical ventilation; ICU, intensive care unit.
| Variables | Treatment Outcome Discharge | Treatment Outcome Death | P-Value b |
|---|---|---|---|
| Gender | < 0.0001 | ||
| Male | 3605 (66) | 1856 (34) | |
| Female | 1826 (57.3) | 1363 (42.7) | |
| Age (y) | 49.63 ± 23.32 | 59.24 ± 21.9 | < 0.0001 |
| Residency | 0.886 | ||
| Urban | 3494 (62.8) | 2066 (37.2) | |
| Rural | 1937 (62.7) | 1153 (37.3) | |
| Marital status | < 0.0001 | ||
| Single | 1943 (71.3) | 782 (28.7) | |
| Married | 3488 (58.9) | 2437 (41.1) | |
| Co-morbidities | < 0.0001 | ||
| Yes | 2748 (55.3) | 2224 (44.7) | |
| No | 2683 (72.9) | 995 (27.1) | |
| GCS | < 0.0001 | ||
| 3 - 5 | 181 (12.1) | 1318 (87.9) | |
| 6 - 8 | 453 (38) | 740 (62) | |
| 9 - 12 | 1822 (67.9) | 860 (32.1) | |
| 12 - 15 | 2975 (90.8) | 301 (9.2) | |
| Days of ICU stay | 4.13 ± 6.55 | 5.99 ± 9.09 | < 0.0001 |
| Not intubated patients | 4752 (87.9) | 655 (12.1) | < 0.0001 |
| Days of MV | 1.09 ± 4.85 | 4.86 ± 8. 69 | < 0.0001 |
Abbreviations: MV, mechanical ventilation; ICU, intensive care unit; GCS, Glasgow Coma Scale.
a Values are expressed as No. (%) or mean ± SD.
b P < 0.05 was considered statistically significant.
| Reasons of Admission | Discharge | Death | P-Value b |
|---|---|---|---|
| Multiple trauma | 1392 (83.3) | 279 (16.7) | < 0.0001 |
| Head trauma+multiple trauma | 1304 (65.1) | 699 (34.9) | |
| CVA | 984 (43.6) | 1275 (56.4) | |
| Seizure | 542 (80.3) | 133 (19.7) | |
| Other | 392 (50.8) | 380 (49.2) | |
| Poisoning | 388 (80.3) | 95 (19.7) | |
| Sepsis | 207 (48.5) | 220 (51.5) | |
| Head trauma | 148 (67) | 73 (33) | |
| Post surgery | 74 (53.2) | 65 (46.8) |
a Values are expressed as No. (%).
b P < 0.05 was considered statistically significant.
Significant associations with increased mortality risk were found for several variables. Age was a key factor, with the deceased group averaging 59.24 ± 21.9 years, compared to 49.63 ± 23.32 years for those discharged (P < 0.0001). Female gender was more common in the deceased group (42.7%) than in the discharged group (57.3%, P < 0.0001). Married individuals were at a higher risk of mortality, with 41.1% of deceased patients being married, compared to 58.9% of those discharged (P < 0.0001). Additionally, a longer ICU stay was associated with a higher mortality risk, with the deceased group having an average stay of 5.99 ± 9.09 days, compared to 4.13 ± 6.55 days in the discharged group (P < 0.0001).
A GCS score of 3 - 5 was significantly associated with mortality, with 87.9% of the deceased patients in this range compared to 12.1% of the discharged patients (P < 0.0001). Mechanical ventilation was also a strong predictor of mortality. The deceased group had a longer duration of MV (4.86 ± 8.69 days) compared to the discharged group (1.09 ± 4.85 days, P < 0.0001). Comorbidities were present in 44.7% of deceased patients and 55.3% of discharged patients (P < 0.0001).
Logistic regression analysis revealed several independent predictors of mortality. Patients aged 21 - 40 had a 1.78 times higher risk of mortality than those aged less than 20 (P < 0.0001), while patients aged 41 - 60 had a 1.45 times higher risk (P = 0.021), and those aged over 80 had a 1.59 times higher risk compared to patients under 20 (P = 0.009). Female gender increased the risk of mortality by 1.39 times compared to males (P < 0.0001). Married individuals had a 1.22 times higher risk of mortality compared to single individuals (P = 0.022). Comorbidities increased the risk of mortality by 1.5 times (P < 0.0001).
Length of ICU stay also influenced mortality risk. A stay of 4 - 7 days increased the risk of mortality by 1.28 times compared to a one-day stay (P < 0.0001), while a stay of more than 7 days increased the risk by 1.5 times (P < 0.0001). Mechanical ventilation was another significant factor, with one day of MV increasing the risk of mortality by 21.8 times compared to non-intubated patients. Ventilation for 2 - 3 days increased the risk by 17.51 times, and 4-7 days of ventilation increased the risk by 66.22 times (P < 0.0001). A GCS score of 3 - 5 increased the risk of mortality by 41 times, while a GCS score of 6-8 increased the risk by 1.93 times, and a GCS score of 9-12 increased the risk by 79 times compared to patients with a GCS score of 12 - 15 (P < 0.0001).
5. Discussion
This study identified that the ICU mortality rate in the GICU of an academic hospital in northern Iran was higher when compared to other international studies (4, 7, 8). ICU mortality rates have been reported at 18% - 21% in Brazil (9, 10), while Mayo Medical School reported a mortality rate of 8.2% among ICU patients (11). A similar study from Spain found a mortality rate of 52% among ICU patients, but it is important to note that this study only included patients above the age of 65 (8). Brunker et al. also emphasized the relationship between older age and the risk of mortality (12).
In the study by Rafiei Mehr (13), around 70% of the patients were discharged, and a statistically significant relationship was observed between admission status and mortality, which is consistent with our findings. Mohammadi and Haghighi’s (14) study also reported that more than 70% of patients were discharged, and the study by Abrishamkar et al. (15) reported a mortality rate of 37.4%, which aligns with this study.
The findings indicated that 63.1% of ICU patients were men, and there was a statistically significant relationship between mortality and gender. In this study, female gender increased the probability of death by 1.39 times compared to men. Mohammadi et al. (14)showed that 66.5% of ICU patients were men, and Prin and Lie (16) reported that approximately 70% of their patients were men, both of which are similar to our findings. However, Rafieemehr et al. (13) found no significant statistical relationship between gender and mortality, which contrasts with our results. In the study by Izadi et al. (17), 89.5% of ICU patients were men, which is in line with our study, but they found no significant relationship between gender and clinical outcomes, which again differs from our findings.
Similar to our study, Khorramnia et al. (18) also found a significant relationship between gender and mortality. Additionally, an inverse and significant statistical relationship was observed between age and mortality, which was expected since increasing age is associated with more comorbidities and higher ASA (American Society of Anesthesiologists) classification. This association has been reported in other studies as well (13-15, 17).
In the study by Izadi et al. (17), no significant relationship was observed between age and mortality, which contrasts with our findings. This discrepancy may be explained by the fact that most of their study's patients were in the same age range of 16 to 30 years. In contrast, our study, similar to that of Moridi et al. (19), found that older age had a positive and significant relationship with length of stay, decreasing levels of consciousness, and the incidence of infection, all of which are predisposing factors for mortality. Prin and Li (16) also reported that poor outcomes were associated with older ages and comorbidities. A statistically significant relationship was found between mortality and underlying disease status, which increased the mortality rate by 1.5 times, confirming the results of Mohammadi and Haghighi's study (14).
Our study found that a GCS score in the range of 3 - 5 increased the risk of mortality by 10.41 times compared to patients with scores of 12 - 15. This finding aligns with Abrishamkar et al.'s study (15), which reported that brain trauma with a GCS score lower than 8 was a major factor in increasing mortality in ICU patients. Izadi et al. (17) similarly found that the chance of survival decreased by 0.65 for each point decrease in GCS.
In terms of admission causes, cerebrovascular accident (CVA) was the most common, followed by head trauma and multiple traumas. A statistically significant association was observed between admission causes and mortality rates. Mortality was higher among patients with CVA, post-surgery complications, and sepsis compared to trauma cases. This may be attributed to the fact that stroke patients were generally older and had more comorbidities. Additionally, during the period of this study, which coincided with the COVID-19 pandemic, only emergency surgeries and cancer-related surgeries were performed, while elective surgeries were postponed. As a result, surgical patients were often in worse health conditions, which likely contributed to higher mortality rates. Abrishamkar et al. (15) also identified respiratory failure as a major factor in ICU mortality, consistent with our findings, and Khorramnia et al. (18) similarly reported that longer ICU stays were associated with higher mortality rates.
As discussed, the results of different studies vary, underscoring the importance of conducting independent investigations at each center. The quality of care provided in different ICUs is influenced by several factors, including equipment availability, economic resources, the experience and knowledge of ICU staff, and their job satisfaction. Studies have shown that sociodemographic characteristics of the populations and their health status are also influential factors that affect patient outcomes (20).
5.1. Suggestions
Considering the significance of this issue and the lack of comprehensive studies, it is recommended that future research be conducted prospectively and in a multicenter format. This would allow for a more thorough assessment of additional variables and enable follow-up with patients after discharge. In this study, we categorized the outcomes into two groups: Death and discharge; however, we were unable to follow up with patients after discharge. Information about patient survival is much more critical than mere discharge status.
5.2. Limitations
This study provided valuable insights into the current conditions of a general ICU in an academic center. However, being a retrospective study, we acknowledge several limitations. Some medical files were excluded due to missing essential data, and the available data were restricted to what had been recorded in medical files. Another notable limitation was that the study period overlapped with the COVID-19 pandemic, which influenced medical strategies and patient care.
5.3. Conclusions
The findings of this study indicated that 62.8% of the patients were discharged, and 37.2% died—a mortality rate higher than the 12.2% reported in the United States. The most common cause of mortality in the General ICU was "CVA." Factors such as increased length of stay, extended days on MV, and older age were positively associated with a higher mortality rate. While a statistically significant relationship was observed between gender, marital status, and mortality rate, these factors are not practically useful as they are unmodifiable.