1. Background
Labor pain is a key concern for parturients and is often the most severe pain that most women experience in their lives. Effective and safe pain relief during labor continues to be a challenge for both anesthesiologists and obstetricians (1). The positive influence of painless labor (PL) on maternal and neonatal outcomes is supported by valid evidence. Studies have demonstrated that postpartum depression is lower in women who experience PL compared to those who undergo natural delivery (2). While research on PL in developed countries has advanced to focus on methods of choice (3, 4), in developing countries, research is very limited (5-7). Studies indicate that in low-income and developing countries, PL is often neglected due to a lack of sufficient information about its possibility among both pregnant women and medical staff (8).
Since PL is one of the main rights of every pregnant woman, serious efforts are necessary to promote it. As a first step, it is essential to identify the obstacles. These obstacles vary by center and are influenced by factors such as the level of knowledge of mothers, cultural beliefs (9), the views and attitudes of doctors (5, 6), the facilities available at the center, and the socio-economic characteristics of individuals. Therefore, the results of other research cannot be generalized, and each hospital must be aware of its specific situation (7, 10-12). It should be noted that fear of severe pain during labor is a major deterrent to childbearing (13). Given the negative population growth in Iran, practical interventions are needed to improve the current situation (14).
Al-Zahra is an academic hospital and the main referral center for elective and emergency high-risk pregnancies. Therefore, optimal care is expected for both mother and baby. To the best of our knowledge, no similar study has been conducted in Guilan province focusing on PL, particularly in this university hospital. Thus, this research was planned to investigate the main barriers to developing PL. Studies have shown that a mother's unpleasant experiences from previous childbirth can negatively impact her desire for childbearing. Considering the importance of the youth population in the country, and especially in Guilan province, conducting this research is valuable (15).
2. Objectives
This study aims to examine the obstacles to PL from the perspectives of anesthesiologists, obstetricians, and midwives at Al-Zahra Hospital, an academic referral center.
3. Methods
Following approval from the Research Ethics Committee of Guilan University of Medical Sciences (GUMS), this cross-sectional descriptive study was conducted at Al-Zahra Hospital from May 2024 to June 2024. Al-Zahra is a referral and academic center affiliated with GUMS, located in the north of Iran, with 182 beds specializing in all types of obstetrics and gynecology surgeries.
Initially, the purpose of the study was explained to the subjects, and those who agreed to participate were asked to complete a checklist. The data collection tool comprised two parts: The first part collected demographic data (gender, years of experience, specialized fields, and degree), and the second part included 8 items addressing the barriers to PL in this hospital. These barriers included lack of anesthesiologists, not informing pregnant women about the possibility of PL, unwillingness of obstetricians to schedule pregnant women for painless delivery, obstetricians' concerns about interference with the delivery process, maternal refusal, lack of necessary facilities, lack of anesthesiology technicians, and lack of midwives. Participants could select one or more items.
Sampling was conducted using a census method, including all members working at Al-Zahra Hospital in the three groups: Obstetrics and gynecology, anesthesiology, and midwifery.
3.1. Inclusion Criteria
All members of the obstetrics & gynecology, anesthesiology, and midwifery departments at Al-Zahra Hospital.
3.2. Exclusion Criteria
Unwillingness to participate in the research.
3.3. Statistical Analysis
The collected data were analyzed using SPSS version 22 software. Results were expressed as frequency (percentage) for categorical data, or as mean and standard deviation (SD), or median for continuous data. The chi-square test was also used.
3.4. Ethics Considerations
This study was approved by the Committee of Ethics in Research of GUMS under the reference number IR.GUMS.REC.1403.033.
4. Results
Finally, 65 out of the expected 84 questionnaires were fully completed, resulting in a response rate of 77.3%. Among the participants, 6.15% were men, and 93.85% were women. The mean years of experience was 9.91 ± 7.49 (range: 1 - 32 years). A total of 60% of the participants had less than 10 years of experience, 32.3% had 10 - 20 years, and 7.7% had more than 20 years of experience (Table 1).
| Variables | Values |
|---|---|
| Gender | |
| Male | 4 (6.2) |
| Female | 61 (93.8) |
| Years of experience [mean ± SD (min - max)] | 9.91 ± 7.49 (1 - 32) |
| ≤ 10 | 39 (60) |
| 10 - 20 | 21 (32.3) |
| ≥ 20 | 5 (7.7) |
| Groups | |
| Anesthesiology | 15 (23.1) |
| Obstetricians | 23 (35.4) |
| Midwifery | 27 (41.5) |
a Values are expressed as No. (%) unless otherwise indicated.
The most frequently reported barrier was obstetricians’ concern about the interference of this method with the delivery process, cited by 43 participants (25%), followed by a lack of anesthesiologists (37 participants, 21.5%) and the unwillingness of obstetricians to recommend painless delivery to pregnant women (28 participants, 16.3%). The least reported barrier was maternal refusal, noted by 3 participants (1.7%) (Table 2).
| Barriers to PL | No. (%) |
|---|---|
| Obstetrics’ worry about the interference of this method with the delivery process | 43 (25) |
| Lack of anesthesiologists | 37 (21.5) |
| Unwillingness of obstetricians to schedule pregnant women for painless delivery | 28 (16.3) |
| Lack of necessary facilities (suitable space-tools) | 28 (16.3) |
| Lack of technician of anesthesiology | 16 (9.3) |
| Not informing pregnant women about the possibility of PL | 11 (6.4) |
| Lack of midwives | 6 (3.5) |
| Maternal refusal | 3 (1.7) |
| Total | 172 (100) |
Abbreviation: PL, painless labor.
Participants with less than 10 years of experience most frequently cited "obstetricians’ concern about the interference of this method with the delivery process" as the primary obstacle (30 participants, 28.6%). In contrast, those with more than 10 years of experience identified "lack of anesthesiologists" as the main barrier (13 participants, 24.5%) (Table 3).
| Barriers to PL | Years of Experience ≤ 10 | Years of Experience 10 - 20 | Years of Experience ≥ 20 |
|---|---|---|---|
| Lack of anesthesiologists | 19 (18.1) | 13 (24.5) | 4 (35.7) |
| Not informing pregnant women about the possibility of PL | 7 (6.7) | 4 (7.5) | 0 (0) |
| Unwillingness of obstetricians to schedule pregnant women for painless delivery | 18 (7.1) | 9 (17) | 1 (7.1) |
| Obstetrics’ worry about the interference of this method with the delivery process | 30 (28.6) | 12 (22.6) | 1 (7.1) |
| Maternal refusal | 2 (1.9) | 1 (1.9) | 0 (0) |
| Lack of necessary facilities (suitable space-tools) | 17 (16.2) | 7 (13.2) | 4 (28.6) |
| Lack of technician of anesthesiology | 7 (6.7) | 6 (11.3) | 3 (21.4) |
| Lack of midwives | 5 (4.7) | 1 (1.9) | 0 (0) |
Abbreviation: PL, painless labor.
a Values are expressed as No. (%).
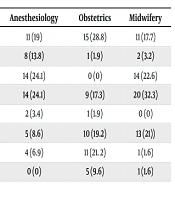
As shown in Table 4, anesthesiology and midwifery professionals identified "unwillingness of obstetricians and gynecologists to recommend painless delivery" and "concern about the interference of this method with the delivery process" as the main obstacles. However, in the field of obstetrics, the most frequently mentioned barrier was the "low number of anesthesiologists", cited by 28.8% of participants.
| Barriers to PL | Anesthesiology | Obstetrics | Midwifery |
|---|---|---|---|
| Lack of anesthesiologists | 11 (19) | 15 (28.8) | 11 (17.7) |
| Not informing pregnant women about the possibility of PL | 8 (13.8) | 1 (1.9) | 2 (3.2) |
| Unwillingness of obstetricians to schedule pregnant women for painless delivery | 14 (24.1) | 0 (0) | 14 (22.6) |
| Obstetrics’ worry about the interference of this method with the delivery process | 14 (24.1) | 9 (17.3) | 20 (32.3) |
| Maternal refusal | 2 (3.4) | 1 (1.9) | 0 (0) |
| Lack of necessary facilities (suitable space-tools) | 5 (8.6) | 10 (19.2) | 13 (21)) |
| Lack of technician of anesthesiology | 4 (6.9) | 11 (21. 2) | 1 (1.6) |
| Lack of midwives | 0 (0) | 5 (9.6) | 1 (1.6) |
Abbreviation: PL, painless labor.
a Values are expressed as No. (%).
5. Discussion
In this study, for the first time in Iran, the main barriers to PL were investigated. The results from an academic referral center in Guilan province showed a response rate of 77.3%, with the highest participation from the midwifery group. A noteworthy finding was that specialists with more than twenty years of experience had the lowest participation, which is not a desirable outcome.
Overall, the primary barrier identified was the "unwillingness of obstetricians and gynecologists to recommend PL to pregnant women". This concern was closely linked to another major reported barrier: "obstetricians’ and gynecologists’ worry about interference with the delivery process". This misconception requires special attention and correction, as valid studies have clearly demonstrated that PL does not significantly interfere with labor. Deepak et al. reported that regional techniques were applied without an increased risk of instrumental vaginal birth or cesarean section. The duration of the active phase of the first stage of labor was not prolonged, although the duration of the second stage was slightly affected, with no adverse outcomes (16).
Another significant barrier was the lack of an adequate number of anesthesiologists. Since implementing PL requires active collaboration between anesthesiology and obstetrics teams, the limited number of anesthesiologists could be a major challenge. The disparity in the number of assistants and specialists in obstetrics and anesthesia itself may act as the first barrier in any joint planning effort, including PL implementation.
Al-Zahra Hospital is an academic and referral center for high-risk and emergency pregnancies. Additionally, it serves as a super-specialized center for various gynecological surgeries. Due to this high patient turnover, the workload of anesthesiologists at this center is substantial. Notably, only one anesthesiologist is available during evening and night shifts to handle all these demanding responsibilities, while the obstetrics department is staffed with two specialists and eight residents per shift. These unequal conditions can negatively impact the anesthesiologist's performance and compromise patient safety. This issue extends beyond PL and is evident in other critical situations, such as neonatal resuscitation in the operating room.
Currently, the role of anesthesiologists extends far beyond the operating room. They are critically involved in radiology (17), cardiology (18, 19), pain management (20, 21), intensive care units (22, 23), and other medical fields. The expansion of hospitals, operating rooms, and outpatient procedures requiring sedation, along with increased public awareness and expectations regarding the presence and intervention of anesthesiology experts, has further emphasized the role of anesthesiologists. The complexity of this profession and its unique challenges (24, 25) should not be overlooked, as they are not specific to Iran but are observed globally (26-28). Additionally, in crisis situations such as the COVID-19 pandemic, anesthesiologists have played a crucial role in managing emergencies and reducing mortality rates (29, 30).
Unfortunately, given the current conditions for anesthesiology residents in Iran and the lack of motivation to enter the field, public health may be at serious risk in the near future.
Another reported barrier was the lack of patient education about the availability of painless childbirth, but this cannot be attributed solely to the hospital's medical staff. Promoting PL when adequate facilities are not available can lead to dissatisfaction and frustration. It is essential to first establish continuous and practical pain relief services and address existing barriers before promoting this option.
On the other hand, a previous study at this center demonstrated that despite limited maternal knowledge about PL, women had a positive attitude and acceptance toward the method (31), which contrasts with similar studies conducted in Iran (7, 32). Therefore, as shown in this study, this factor may not be a significant barrier.
A study conducted at a teaching hospital in Pakistan found that PL was rarely accepted by pregnant women. The primary barriers included false beliefs and misconceptions among pregnant women (which contrasts with our findings), the attitudes of gynecologists, and the insufficient number of trained medical personnel — issues that align with the present study (33).
Similarly, Rafiq et al. explored barriers to effective PL in government and academic hospitals among obstetricians and gynecologists. Their findings identified maternal comorbidities, improper nutrition, psychological issues, and professional incompetency as key obstacles (34).
In a study from Egypt, 95% of women reported not receiving adequate information about PL (11), while a recent study in Iran found that 56.61% of women lacked sufficient knowledge about it (8). Additionally, Vosoughian et al. assessed midwives' attitudes toward PL in Iran and found that only 13% of participants achieved a good score (35).
Overall, the importance of PL is widely recognized, and the right of women to experience childbirth without unnecessary pain should not be overlooked. However, the identified barriers must be critically examined, and efforts should focus on addressing and modifying those that can be changed to improve access to PL services.
5.1. Limitations
The findings of this study cannot be generalized to private-sector healthcare settings. The single-center nature of the study is one of its key limitations.
5.2. Suggestions
Given the importance of this issue, it is recommended that future studies be conducted in multiple centers, including private specialist centers and non-educational government hospitals, to compare results and improve the generalizability of findings.
5.3. Conclusions
This study demonstrated that "the unwillingness of obstetricians to recommend PL to pregnant women", strongly driven by concerns about interference with the delivery process, should be corrected. Furthermore, the lack of a sufficient number of anesthesiologists, which limits planning for services beyond the operating room, was confirmed as a major issue. This challenge, which poses a significant threat to the future health of society, must be urgently addressed and resolved by national health policymakers.