1. Background
The safeguarding of patients' rights is a cornerstone of modern healthcare systems, reflecting the fundamental ethical principles of beneficence, non-maleficence, autonomy, and justice. As healthcare delivery becomes increasingly complex, the role of healthcare professionals in protecting and promoting these interests has gained paramount importance (1-3). The concept of patients' rights has evolved significantly over the past century, encompassing a broad spectrum of entitlements, including the right to informed consent, confidentiality, dignity, and autonomy in medical decision-making (4, 5). It requires healthcare professionals to navigate complex ethical dilemmas, balance competing priorities, and make decisions that align with both professional standards and individual patient needs. The multifaceted nature of this responsibility demands a nuanced approach to performance assessment (6, 7).
Conflict of interest occurs when a professional's judgment regarding a primary interest is inappropriately influenced by a secondary interest. It arises when an individual in a position of trust has personal or group interests that conflict with their professional duties (8). This situation can lead to compromised decision-making, even unintentionally, where the primary interest may be neglected in favor of the secondary one. Importantly, an actual compromise of the primary interest isn't necessary for a conflict to exist; the mere potential for such compromise due to existing conditions or relationships is sufficient to constitute a conflict of interest (9, 10).
Recent years have witnessed a growing emphasis on patient-centered care, shared decision-making, and the recognition of patients as active participants in their healthcare journey. This paradigm shift has further underscored the importance of healthcare professionals' ability to effectively safeguard patients' interests (11, 12). It has also highlighted the need for robust assessment methodologies that can capture the subtleties and complexities of this aspect of healthcare delivery.
2. Objectives
However, developing effective assessment strategies in this area presents significant challenges. The subjective nature of many aspects of patient safeguarding, the diversity of healthcare settings and specialties, and the potential influence of systemic factors on individual performance all contribute to the complexity of this task (13-15). The current study investigated healthcare professionals' performance regarding safeguarding patients' rights.
3. Methods
This research employed a cross-sectional design to assess the performance of healthcare professionals in safeguarding patients' rights at Guilan University of Medical Sciences in Rasht, Iran. The study aimed to evaluate how well healthcare professionals understand and implement patient rights, which are essential for ethical healthcare delivery.
3.1. Inclusion Criteria
Participants included a diverse range of healthcare professionals, specifically nurses, residents, general physicians, and medical students. This variety allowed us to capture a comprehensive perspective on performance related to patient rights across different levels of experience and specialization. All individuals who consented to participate were included in the study. Informed consent was obtained from each participant prior to data collection, ensuring that they understood the purpose of the study and their right to withdraw at any time without any consequences.
3.2. Exclusion Criteria
Healthcare professionals with less than six months of experience in their respective roles were excluded to ensure that participants had sufficient exposure to patient interactions and relevant ethical considerations.
Data were collected through a self-designed questionnaire that included demographic information (age, gender, marital status, occupation, and education level) as well as specific questions related to knowledge and practices concerning patients' rights. The questionnaire was developed based on existing literature and guidelines on patient rights to ensure relevance and comprehensiveness. Informed consent was obtained from all participants prior to data collection, ensuring that they understood the purpose of the study and their right to withdraw at any time.
Data were analyzed using IBM SPSS Statistics version 26. Descriptive statistics were calculated to summarize demographic characteristics and performance scores. The Kolmogorov-Smirnov test was used to assess the normality of the data distribution. For comparisons between groups, t-tests and ANOVA were employed as appropriate. Additionally, Pearson correlation coefficients were calculated to explore relationships between demographic variables and performance scores. Multiple linear regression analysis was conducted to determine associations between demographic characteristics and informed consent quality scores.
4. Results
A total of 130 healthcare professionals were enrolled in the study. The mean age of participants was 29.42 ± 5.54 years (range, 22 - 51 years), and the majority were female (59.2%). Most healthcare professionals were single (56.2%), nurses (56.9%), and held bachelor's degrees (61.5%). The mean performance score among healthcare professionals was 8.38 ± 1.83, with scores ranging from 4 to 14 (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 53 (40.8) |
| Female | 77 (59.2) |
| Marital status | |
| Single | 73 (56.2) |
| Married | 57 (43.8) |
| Educational status | |
| Bachelor degree | 80 (61.5) |
| Medical student | 6 (4.6) |
| Medical doctor | 44 (33.8) |
| Occupation | |
| Nurse | 74 (56.9) |
| General physician | 13 (10.0) |
| Resident | 13 (10.0) |
| Student | 30 (23.1) |
Demographic Characteristics of Participants (N = 130)
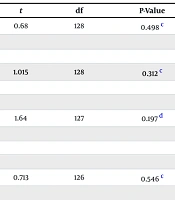
Analysis of professional performance scores showed no statistically significant differences based on gender, marital status, educational status, or occupation (P > 0.05). While females, single individuals, medical doctors, and residents tended to have higher performance scores, these differences were not statistically significant (P > 0.05). For instance, the mean score for females was 8.52 ± 1.79 compared to 8.23 ± 1.87 for males, but this difference did not reach statistical significance (Table 2).
| Variables | Score | t | df b | P-Value c |
|---|---|---|---|---|
| Gender | 0.68 | 128 | 0.498 d | |
| Male | 8.24 ± 2.06 | |||
| Female | 8.47 ± 1.66 | |||
| Marital status | 1.015 | 128 | 0.312 d | |
| Single | 8.52 ± 1.98 | |||
| Married | 8.19 ± 1.61 | |||
| Educational status | 1.64 | 127 | 0.197 e | |
| Bachelor degree | 8.35 ± 1.77 | |||
| Medical student | 7.17 ± 1.72 | |||
| Medical doctor | 8.59 ± 1.91 | |||
| Occupation | 0.713 | 126 | 0.546 d | |
| Nurse | 8.46 ± 1.74 | |||
| General physician | 7.79 ± 1.81 | |||
| Resident | 8.69 ± 1.84 | |||
| Student | 8.54 ± 2.33 |
The Association Between Demographical and Educational Data of 130 Healthcare Professionals with Their Professional Performance a
Regression analysis revealed that none of the variables (gender, marital status, occupation, and educational status) significantly predicted performance scores (P > 0.05). Although gender had a positive unstandardized coefficient (B = 0.060), indicating a potential positive association, this effect was not statistically significant (P > 0.05) (Table 3).
| Variables | Unstandardized Coefficients | Standardized Coefficients | t | P-Value | |
|---|---|---|---|---|---|
| B | SE | Beta | |||
| Gender | 0.060 | 0.034 | 0.181 | 7.392 | 0.083 |
| Marital status | -0.615 | 0.368 | -0.168 | 1.749 | 0.098 |
| Occupation | -0.029 | 0.091 | -0.046 | -1.668 | 0.755 |
| Educational status | -0.123 | 0.194 | -0.096 | -0.313 | 0.528 |
The Assessments of Simultaneous Effects of Demographical and Educational Variables on Professionals' Performance a
5. Discussion
Protecting patients' rights is a foundational principle in contemporary healthcare, encompassing the ethical obligation to respect individuals' autonomy, dignity, and privacy in medical settings. These rights, which include informed consent, the right to refuse treatment, confidentiality, and access to care, are crucial for maintaining the trust that underpins patient-provider relationships (2, 16). In an era where healthcare systems are rapidly evolving due to technological advancements, policy shifts, and the increasing complexity of care delivery, ensuring that these rights are upheld is more important than ever. Ethical medical practices require that healthcare professionals remain vigilant in their efforts to balance clinical objectives with respect for patients' choices and needs (17, 18). Moreover, as healthcare becomes more interdisciplinary and data-driven, there is a growing need to continually evaluate how well healthcare systems support patient rights, adapting policies and practices to meet emerging challenges (19, 20). Protecting these rights not only safeguards individuals from harm or neglect but also fosters a healthcare environment rooted in respect, transparency, and accountability.
In the current study, the average performance score suggested a moderate level of performance in safeguarding patients' rights. This result aligns with previous studies that have highlighted varying levels of awareness and implementation of patient rights among healthcare providers. Despite the moderate performance score, our analysis showed no statistically significant differences in performance based on demographic factors such as gender, marital status, educational status, or occupation (P > 0.05). This lack of significant findings contrasts with some existing literature that suggests demographic factors can influence healthcare professionals' knowledge and practice regarding patient rights. For instance, studies by Alraimi and Shelke (21) and Czajowska et al. (22) have indicated that specific demographic characteristics may correlate with higher awareness and better communication of patients' rights. However, our results suggest that the factors influencing performance may be more nuanced than previously understood.
Interestingly, although females, single individuals, medical doctors, and residents exhibited higher average performance scores, these differences were not statistically significant. This trend raises important questions about the underlying reasons for these observations. For example, while female healthcare professionals often report higher levels of empathy and communication skills — traits essential for safeguarding patient rights — our study did not find a corresponding statistical significance in their performance scores. This discrepancy may indicate that other factors, such as institutional support or training opportunities, play a more critical role in determining performance than demographic characteristics alone.
The regression analysis further confirmed that none of the demographic variables significantly impacted performance scores (P > 0.05). However, the positive unstandardized coefficient for gender (B = 0.060) suggests a potential association worth exploring in future research. This finding aligns with the notion that gender dynamics within healthcare settings may influence professional interactions and patient advocacy efforts. Moreover, the absence of significant differences based on marital status contradicts some studies that have linked marital status to job satisfaction and burnout levels among healthcare professionals.
For instance, previous research has shown that married individuals often report higher job satisfaction compared to their single counterparts (23-25). However, our findings suggest that marital status may not directly influence performance in safeguarding patients' rights within this specific context. The moderate performance level observed in this study underscores the necessity for targeted educational programs and policy interventions aimed at enhancing healthcare professionals' understanding and implementation of patient rights. As healthcare systems become increasingly complex due to technological advancements and evolving patient needs, it is crucial to ensure that all healthcare providers are adequately trained to uphold ethical standards related to patient care.
This study had several limitations: First, the relatively small sample size and the focus on a single healthcare setting might limit generalizability. Second, while the study collected demographic data (age, gender, marital status, occupation, education), it did not explore other potentially influential factors such as years of experience, specific training related to patient rights, or institutional policies that might impact performance. Future research could benefit from larger, multi-center studies to validate these findings across diverse healthcare environments. These findings underscore the need for comprehensive, targeted interventions to enhance healthcare professionals' competencies in protecting and promoting patients' rights across all demographic groups.
5.1. Conclusions
The lack of significant differences in performance across demographic groups highlights the importance of developing comprehensive training programs that are universally applicable. These programs should focus on enhancing competencies in safeguarding patients' rights, regardless of healthcare professionals' gender, marital status, occupation, or educational background. Additionally, exploring other factors that might influence performance, such as work environment or training experiences, could provide further insights into improving patient care.