1. Context
Status epilepticus (SE), a serious neurological condition in pediatric cases, affects individuals of all ages and induces greater mortality and morbidity in infants (1). This condition refers to prolonged electrographic or clinical seizures that do not resolve after an expected time. The incidence of convulsive status epilepticus (CSE) is approximately 15 to 25 per 100,000 pediatric cases per year and 15 to 40 per 100,000 per year. The highest incidence is observed in infancy, and in the elderly, it reflects the underlying CSE etiology (1, 2). The common etiology of adult CSE is acute symptomatic seizure, observed in 48 to 60 percent of CSE cases. Additionally, a common etiology is stroke induced by an infarct or a hemorrhage. Other causes include metabolic, alcohol-related, infection, and hypoxia (3). The second most common etiology of CSE is absent or low ASM levels in epileptic cases, reflecting poor ASM compliance. The most common reason for non-compliance is a sudden, rather than gradual, medication discontinuation (4). Previous studies have highlighted this as a significant problem in CSE causes. A small number of patients, particularly adults, may present with what appears to be CSE or, more accurately, “non-epileptic CSE, psychogenic” (5). In the established SE treatment trial, ten percent of 384 cases registered in this randomized and double-blind study were considered to have the psychogenic type of CSE (6, 7).
Convulsive status epilepticus is often managed by specific local or national algorithms. First-line treatment is used when a focal motor clonic or tonic clonic seizure lasts more than five minutes (premonitory or impending CSE) (8). When CSE persists despite two first-line doses, it is considered established CSE, and second-line treatment is administered. Various randomized clinical trials (RCTs) support the use of benzodiazepines as the first-line drug (9). Additionally, alternative drugs, with less data from RCT studies, include intravenous clonazepam and intramuscular midazolam. Up until 2019, phenytoin and phenobarbital were the preferred second-line drugs, but there is no significant RCT data supporting their use. Lacosamide is also an alternative second-line agent, but it lacks supporting evidence from RCT studies (10). Current data show that intravenous lorazepam or intranasal or buccal midazolam are the most effective first-line drugs for managing premonitory or impending CSE. There is no significant difference in the effectiveness of phenytoin, sodium valproate, or levetiracetam for the management of established CSE (3, 4).
Information from different clinical trial studies from ten to fifteen years ago has indicated that benzodiazepines can manage impending CSE in 60 - 90 percent of patients (11). However, more data is needed to determine the best drug for better control of this condition. In the present review study, we provide a general overview of SE and evaluate therapeutic algorithms in Iran.
2. Evidence Acquisition
2.1. Study Setting
This study was approved and conducted at Tehran University of Medical Sciences.
2.2. Study Design
The present minor review study project was designed according to standard guidelines to assess relevant data concerning depression and multiple sclerosis. The study keywords, which were combined with each other, included “anticonvulsants”, “pediatric”, “status epilepticus”, “convulsive”, “emergency”, “anti-seizure medications”, and “children”.
2.3. Inclusion and Exclusion Criteria
Published studies about SE in Iran and worldwide were evaluated. Furthermore, in research, review articles, and case reports, studies that only had abstracts, examinations lacking safety, book chapters, articles not found, congress abstracts, review-type articles, articles without statistical indices, inadequate data, or irrelevant content were excluded.
2.4. Quality Assessment and Data Extraction
In research and review studies, data were abstracted independently. Additionally, the following data were extracted: Region, size of study sample, study period, country, publication year, and study name. The quality of research was also checked independently according to the Joanna Briggs Institute’s critical appraisal checklist.
2.5. Databases
The study was carried out using English databases, including NHS, WHO, PubMed, Google Scholar, Science Direct, and Scopus.
3. Results
3.1. Status Epilepticus Definition
Different definitions have been published and suggested over the last five decades to define the concept of SE (12). However, there is not yet a universally accepted definition, particularly regarding the duration of clinical seizures that is sufficient and necessary to define SE (13). In 1993, the Epilepsy Foundation of America and the International League Against Epilepsy defined SE as a condition in which one or more seizure attacks continue for more than 30 minutes without recovery of consciousness or function (14, 15). Similarly, the Italian League Against Epilepsy provided the following definition for adults: Status epilepticus is a clinical condition characterized by continuous seizures (partial or generalized, with or without motor manifestations) lasting more than 20 minutes or repeated in less than one minute (16, 17).
The necessary factor in the definitions of SE is the time criterion. Experimental and clinical data have shown that persistent epilepsy (especially more than 20 - 30 minutes), particularly if convulsive, has the potential not only to induce neuronal damage (even with adequate brain oxygenation) but also to lead to central nervous system (CNS) harm. In addition, according to these so-called "injury-based" definitions, which are useful in epidemiological research, there is evidence that a single seizure rarely lasts more than 2 to 10 minutes. This has led to the incorporation of a working definition that allows treatment to be promptly started.
3.2. Classification
Status epilepticus may be classified based on various data: Etiology, duration of seizures, and clinical manifestations (18). Even though there are several SE classifications, according to basal epileptic syndrome over decades, the first basic distinction is between nonconvulsive SE (NCSE) and CSE (7). The second involves different conditions with impaired consciousness (slow psychomotor, obnubilation, absences), with minor motor system activity or absence of this function (complex or simple gestural automatisms, repeated blinking, focal clonus rhythm), although this is not the subject of our article. It must be noted that initial CSE treatment can blunt or prevent motor demonstrations; however, ictal electric activity consistent with NCSE could persist (19, 20).
General and partial epilepticus status distinction is according to the presence of bilateral or unilateral motor demonstration, in addition to generalized or focal electrical activity of seizure. This distinction is fundamental in guiding a diagnosis (13, 21, 22). Based on event duration, which reflects treatment response, CSE could be divided into refractory CSE (lasting > 60 mins); defined CSE (duration 30 - 60 mins); and initial CSE (duration < 20 - 30 mins) (23, 24).
3.3. Etiology and Epidemiology of Convulsive status epilepticus
The CSE incidence is approximately 15 to 25 in 100,000 pediatric cases per year and 15 to 40 per 100,000 per year. In infancy, the highest incidence is observed, and in the elderly, it reflects underlying CSE etiology (25, 26).
Convulsive status epilepticus etiology is relevant to the management of this condition, so it is significant to consider and deplete any treatable etiology, specifically an underlying infection (particularly encephalitis or meningitis) or metabolic etiology (27). The common metabolic etiologies are hypocalcemia, hypoglycemia, hypoxia, and hyper- or hyponatremia (28, 29).
Convulsive status epilepticus analysis based on causes is complicated by the fact that its classification has changed and evolved, and not all authors use the same classification. In addition, the mentioned prevalence of different etiologies is not consistent (27). Recently, the classification of ILAE based on etiology is: Related to epilepsy, acute symptomatic, and febrile; these are also divided into etiologies and specific epilepsy syndromes (30). Based on this definition, a recent study of 665 pediatric cases (≤ 15 years) affected by CSE observed that 55.5% had epileptic CSE, 41.2% had febrile CSE, and 2.1% had acute seizures. Furthermore, a more recent study on children mentioned that the acute symptomatic group was observed in 17% of CSE causes (27, 31).
3.3.1. Adults (> 18 Years)
A common etiology of adult CSE is acute symptomatic seizure, which is observed in 48 to 60 percent of CSE cases. In addition, a common etiology is stroke induced by an infarct or a hemorrhage. Additional causes include metabolic, alcohol-related, infection, and hypoxia. The second most common cause of CSE in older cases is absent or low ASM levels in cases with previous epilepsy, which shows a low level of compliance to ASM. The probable etiology of cases without compliance is a precipitate and not a gradual discontinuation of the drug. There is an important problem in CSE etiology. A small number of patients, particularly adults, could present with what appears to be CSE or, more suitably, “non-epileptic or psychogenic CSE” (32). Based on etiology, pediatric cases with CSE could be divided into the following (16, 33-35):
- Healthy pediatric cases with febrile convulsion which is initially prolonged
- Healthy pediatric cases with febrile convulsion which is previously prolonged
- Healthy pediatric cases at the first manifestation of idiopathic epilepsy
- Healthy pediatric cases with a previous detection of idiopathic epilepsy
- Pediatric cases with a previous detection of symptomatic epilepsy
- Previously normal pediatric cases with an acute CNS insult
- Pediatric cases with a CSE in the first episode, not included in the mentioned cases
3.4. Early Recognition and Diagnosis
Multiple studies have investigated pediatric SE etiologies, and febrile SE is the most common diagnosis (36). Precipitant categories include acute symptomatic, remote symptomatic, acute-on-remote symptomatic, cryptogenic, and idiopathic. Acute symptomatic and acute-on-remote symptomatic causes, which comprise 17% to 26% of cases of pediatric SE, respectively (3, 11, 37, 38), should be evaluated urgently, as addressing these precipitants may simultaneously treat seizures. The American Academy of Neurology practice parameter addressing the diagnostic assessment of a child with CSE reported that abnormal results among children who underwent testing included low anti-seizure medication levels (32%), neuroimaging abnormalities (8%), electrolytes (6%), inborn errors of metabolism (4%), ingestion (4%), CNS infections (3%), and positive blood cultures (3%) (39). To identify these precipitants, the Neurocritical Care Society’s guideline recommends a finger-stick glucose in the initial two minutes as well as a serum glucose, complete blood count, basic metabolic panel, blood gas, calcium, magnesium, and anti-seizure medication levels drawn in the initial five minutes (3). Rapidly correctable causes of SE should be identified and treated as quickly as possible, including hypoglycemia, hypocalcemia, hyponatremia, and hypomagnesemia (40). Therefore, considering certain conditions that predispose a person to seizures can be used for rapid diagnosis.
Status epilepticus management in prehospital setting: Generalized CSE, as an emergency condition, should be dealt with adequately and promptly to decrease mortality and morbidity. Treatment of this condition must start before hospital arrival, even without venous access (41). In the prehospital setting, use benzodiazepines in seizures lasting more than five minutes, which improves outcomes. For years, in the prehospital setting, rectal diazepam (0.5 mg/kg) was the choice management approach (38, 42). In addition, transmucosal midazolam administered buccally (0.5 mg/kg) is as effective as diazepam administered rectally (0.5 mg/kg) and has equal safety; however, buccal transmucosal midazolam is higher socially (43). Also, transmucosal nasal midazolam (0.2 mg/kg) has a higher effect and is safer than rectal diazepam (44). A recent study observed that intramuscular midazolam by paramedics was as effective as, and safer than, intravenous lorazepam. Intravenous midazolam use has been recently evaluated in Italy for SE treatment (37, 45).
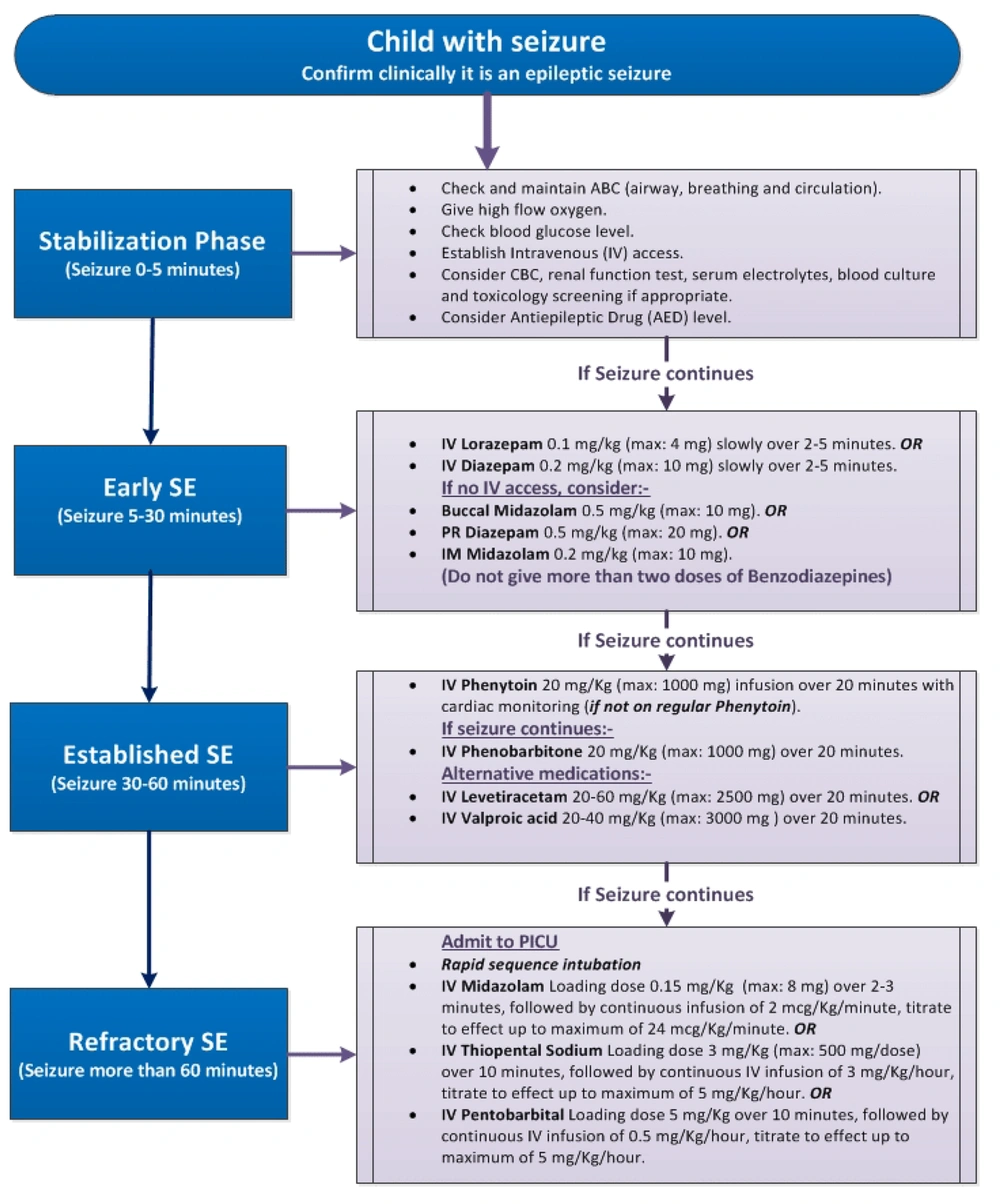
3.5. Status Epilepticus Management in Hospital Setting
At first, vital signs should be evaluated based on the ABC sequence during all phases. Based on the change from primitive to definitive SE, any effort should be made to determine SE etiology, correct any dysfunction of the metabolic system, and treat and monitor abnormal blood pressure changes (19). It is also necessary to start monitoring EEG, if this has not been previously done, to confirm, assess, and detect therapy effectiveness and the need for admission to the ICU for further treatment. International guidelines and treatment algorithms for CSE are provided in Figure 1 (6, 39).
Clinical algorithm for treatment of convulsive status epilepticus (CSE) in children (46)
3.6. Medicine Management
3.6.1. Initial Convulsive Status Epilepticus
Benzodiazepines are the first-line medicine for the management of initial CSE. In pediatric cases, intravenous lorazepam has an effect equal to intravenous diazepam (47). Pediatric cases receiving intravenous lorazepam are less likely to need additional anticonvulsant agent doses to stop seizures, develop respiratory system depression, and require ICU admission (15). Midazolam administered intramuscularly is as effective and safe as intravenous diazepam, with an overall shorter time for resolution of CSE, and has effectiveness and safety equal to intravenous lorazepam (24, 48).
3.6.2. Definite Convulsive Status Epilepticus
Phenobarbital and sodium phenytoin are other drugs to consider if benzodiazepines fail. There is no comparative research in pediatric cases of phenobarbital and phenytoin (49). In adult cases, phenytoin is less effective than phenobarbital; however, it is just as effective as phenytoin (50). In some protocols in pediatric cases, phenobarbital and sodium phenytoin are not used sequentially but alternately. When used in sequence, as suggested by the mentioned protocol, phenytoin is generally preferred to phenobarbital based on its higher safety and lower depression of the cardiorespiratory system, especially in cases where benzodiazepines have already been used (11, 51). In a recent double-blind and randomized study in pediatric cases under two years of age, after the use of intravenous diazepam with persistent CSE, a bolus intravenous injection of valproic acid had a higher influence and was better tolerated than a bolus intravenous injection of phenobarbital (11, 38).
3.6.3. Refractory Convulsive Status Epilepticus
After all mentioned items, if seizures persist, the patient must be transferred to an ICU for coma induction by barbiturates, midazolam, or propofol (52). In pediatric cases, monitoring of EEG in refractory CSE follows the same rules as in adults. Management and induction of drug-induced coma must be completed based on continuous EEG monitoring of brain activity (52). Recurrent CSE has a higher rate of mortality, mainly related to the underlying etiology. Prognosis is more severe when CSE occurs in the course of encephalitis (53). There are no RCT studies for refractory SE treatment in pediatric cases, but retrospective studies could provide information about the type of medicine used (midazolam, propofol, sodium thiopental), as well as proficient guidelines and opinions (40). Treatment guidelines differ from country to country based on legislative regulations and commercially available sedatives (54, 55).
3.6.4. Treatment Protocol in Iran
The management method for CSE in Iran is consistent with the methods and procedures used in other countries, as mentioned in the following related data. In 0 - 5 minutes, once the diagnosis is confirmed, monitor temperature, blood pressure, heart rate, respiration, and EEG, establish an oral airway, and administer oxygen if necessary. Take an IV catheter and send a venous blood sample for serum levels of anticonvulsants, electrolytes, calcium, magnesium, BUN, and CBC. Check the patient's blood sugar with a glucometer, and suction the patient frequently. Transfer the patient to the PICU. In 6 to 9 minutes, administer 10 ml/kg normal saline intravenously and 5 ml/kg dextrose 5% (in case of hypoglycemia). In 10 to 40 minutes, the medicine is administered based on three levels as follows:
- Lorazepam: Administer 0.1 mg/kg at a rate of 1 - 2 mg/min. Can be repeated one more time after 5 minutes (max. 5 mg) or as follows,
- Diazepam: Administer 0.3 mg/kg within 2 minutes. Can be repeated one more time after 5 minutes (maximum 5 mg in infants and 10 mg in children),
- Phenytoin: Twenty mg/kg at a rate of 1 mg/kg/min. It is possible before starting the next stage; another 10 mg/kg is needed (maximum 1000 mg).
In 41 to 50 minutes, one of the following methods can be used: Phenobarbital: Twenty mg/kg at 50 mg/min (maximum 1000 mg) or sodium valproate: Forty - 20 mg/kg at 3 - 6 mg/kg/min or levetiracetam: Thirty - 60 mg/kg within 5 minutes. In 60 minutes, midazolam should be started at 0.15 mg/kg and then administered at a rate of 1 - 20 µg/kg/min intravenous infusion. Increase the dose every 15 minutes to control seizures based on EEG. The duration of the treatment period is about 12 to 48 hours, and then every 30 minutes, 13 µg/kg/min of the drug dose is tapered. In 61 - 80 minutes, if seizures still persist, use pentobarbital or thiopental, or start general anesthesia with halothane and neuromuscular block. Doses of the mentioned drugs are as follows:
- Pentobarbital: First, 5 mg/kg is administered and then continue intravenous infusion at a rate of 1 - 5 mg/kg/h until the burst-suppression pattern appears in the EEG. The maintenance treatment continues for approximately 4 hours, and by reducing the infusion rate, the patient is checked for the occurrence of convulsive activity. If the patient has seizures again or generalized discharges appear in the EEG, the procedure is repeated. Otherwise, the drug will be tapered within 12 to 24 hours.
- Thiopental: First, 5 mg/kg and then continue intravenous infusion at a rate of 1 mg/kg/h. Increase the dose by 1 mg/kg/h every 30 minutes until a maximum dose of 6 mg/kg/h is reached or before seizures are controlled. The duration of the treatment is 48 hours, and then every 12 hours, 25% of the drug dose is tapered.
One of the strengths of this algorithm is its effective therapeutic application until the end of the treatment. The weakness is the lack of access to some of these drugs in first-level centers.
4. Discussion
Convulsive status epilepticus is the most common SE and accounts for around 90 percent of all pediatric cases. The present study evaluated recent data in Iran and compared it to the world for optimal CSE management in the Emergency Room or Accident Department setting (56). The conducted studies will not evaluate the management of convulsive seizures in neonatal CSE (which is often seen in neonatal special settings or ICU) or non-CSE. It will concentrate on child treatment referred to the Emergency Room or Emergency and Accident Department setting in prolonged generalized or focal tonic-clonic seizure (18, 57). Clinical trial studies and related studies in CSE treatment will often include some data about the need for more research to refute or confirm their results or to detect more effective ASM (58). This is to be expected, as there is yet no combination of drugs or single drug that will terminate established or impending CSE in all cases. The three large clinical trials that evaluated the use of sodium valproate, phenytoin/fosphenytoin, and levetiracetam in established CSE observed a success rate of 50 - 70% (56). Recently, Wang et al. mentioned in a review study the assessment accuracy of STESS diagnostic ability (59). The diagnostic value of the mentioned method was estimated as a specificity of 53% and sensitivity of 81% with an under curve area of 0.81. Based on study analysis, study design, ethnicity, sample size, and publication year did not significantly influence the detection accuracy of STESS. In all mentioned research, STESS may have an excellent negative predictive value (97% - 99%) (2, 60, 61). It remains unclear whether the EEG treatment goal should be the termination of seizures or induction of burst-suppression. The Neurocritical Care Society’s guideline considers either electrographic seizure cessation or burst-suppression as appropriate goals (55). It remains unclear how long the patient should be maintained in pharmacologic coma. A survey of experts in SE management across all age groups reported they would continue pharmacologic coma for 24 hours (62). The Neurocritical Care Society’s guideline recommends 24 - 48 hours of electrographic seizure control prior to the slow withdrawal of continuous infusions (55).
4.1. Conclusions
Data from several clinical trial studies from ten to fifteen years ago mentioned that benzodiazepines can manage impending CSE in 60 - 90 percent of patients. Without immediate intravenous access, these studies have not mentioned that midazolam (intra-nasal or buccal) is significantly more effective or safer than diazepam prescribed rectally. Recent studies have mentioned there is no diversity in effectiveness between intranasal and buccal midazolam. Notwithstanding, we observed less data on superior midazolam efficacy, with a higher efficacy of intranasal or buccal types instead of rectal diazepam. So, the first-choice benzodiazepine is midazolam in the management of first or impending CSE in cases without intravenous access. Intramuscular midazolam offers a third option in cases without intravenous access. However, in cases with immediate intravenous access, studies mentioned there is no diversity in the depression of the respiratory system and efficacy of diazepam and lorazepam administered intravenously. Nevertheless, safety and efficacy information from RCT studies suggest that intravenous lorazepam is preferred to intravenous diazepam. Based on this, the Iranian and international protocols are highly consistent with each other; however, the treatment protocol needs to be modified based on the demographic characteristics of Iran and the treatment response of children in the country.
4.2. Limitations
Our study limitation was the lack of previous studies in the research area in the evaluated field, so we searched studies over a wider time and, based on summarizing them, we have reached a review study. In addition, there is a need for further research about the treatment of CSE.