1. Background
Cerebral venous sinus thrombosis (CVST) constitutes a distinct subtype of cerebrovascular disease. The cerebral venous system, based on the anatomical and functional characteristics of its vasculature, can be broadly categorized into two principal components: The cerebral veins and the dural venous sinuses. Topographically, a superficial and a deep system can be distinguished (1). The superficial system drains blood from the cerebral cortex primarily into the superior sagittal sinus, which subsequently empties into the transverse sinuses. The deep system drains blood from the white matter and basal ganglia into the inferior sagittal sinus, which continues into the straight sinus and then into the transverse sinuses, ultimately draining into the internal jugular veins (1). The incidence of this condition, according to retrospective studies, has been reported to be as high as 13.2 cases per million annually (2). Regarding gender distribution over time, the proportion of female CVST patients has gradually increased. While CVST patients range in age from neonates to 82 years, the disease predominantly affects individuals between 30 and 41 years of age (3). In the majority of patients, multiple venous sinuses are involved. The most commonly affected locations are the superior sagittal sinus, the lateral sinus, and the sigmoid sinus (4). Identifiable causes and predisposing factors for CVST can be determined in 80% of patients, categorized into infectious (e.g., penetrating head injury, intracranial infection, regional infection, etc.) and non-infectious (e.g., head injury, neurosurgery, stroke and hemorrhage, space-occupying lesions, central venous catheter insertion, surgery with immobilization, hormonal and endocrine causes, etc.) groups (5). Clinical manifestations encompass headache, seizures, focal neurological deficits, altered level of consciousness, neuro-ophthalmic signs, vomiting, and psychiatric symptoms (3). The standard treatment for CVST is anticoagulation therapy. Mortality in CVST is lower than in arterial stroke. The majority of CVST patients have a favorable prognosis (6). In CVST, the median time from onset to death is 13 days, and the average time from diagnosis to death is 5 days (3). Red cell distribution width (RDW) reflects the variation in the size of red blood cells (RBCs). The RDW is an indicator of RBC volume heterogeneity and is used for anemia diagnosis (7). An association exists between elevated RDW levels and thrombotic diseases (8, 9). Given that elevated RDW levels represent a risk factor for intracranial hemorrhage in CVST patients, measuring RDW can potentially prevent disease progression and hemorrhagic complications (7). Mean platelet volume (MPV) represents platelet volume. Studies have demonstrated an association between MPV values and arterial thromboses, but their role in venous thromboses is less well understood (10). Although some studies have investigated the association of RDW and MPV with CVST, this relationship has not been definitively established. In this study, we aim to investigate the simultaneous association of RDW and MPV with CVST. Furthermore, considering that CVST diagnosis relies on MRI findings, and given the limitations in imaging resources at medical centers, as well as the potential for diagnostic delays due to ambiguous imaging findings, we aim to investigate the association of these parameters with CVST by comparing RDW and MPV in patients diagnosed with CVST.
2. Objectives
Our goal is to determine whether these parameters can contribute to earlier diagnosis, potentially even in the absence of imaging findings, and whether they can be used to monitor treatment response and patient follow-up.
3. Methods
This study is a descriptive case-control study. The study population consisted of 41 patients definitively diagnosed with CVST based on medical history, clinical manifestations, and MRI findings, who were hospitalized in the neurology ward of Ali Ibn Abitaleb Hospital in Zahedan. The sample size of the control group was 55 participants. Inclusion criteria included complete patient records, availability of initial CBC tests (within the first 24 hours of admission), presence of clinical symptoms including headache, hemiparesis, seizures, papilledema, and decreased level of consciousness, confirmation of CVST diagnosis by MR venography or MRI, and observation of thrombosis in the superior sagittal, transverse, sigmoid, cavernous sinuses, or jugular vein on MRI. Exclusion criteria included patients with a history of arterial thrombosis (stroke, myocardial infarction, or peripheral arterial thrombosis) or venous thromboembolism, diagnosed cancer (including myeloproliferative neoplasms), or pre-existing liver or autoimmune diseases, and patients undergoing treatment with anticoagulants or lipid-lowering medications. The control group consisted of individuals referred to the hospital laboratory for routine examinations who did not present with clinical complaints, including headache, visual disturbances, or neurological symptoms, and had no history of any illness or medication use. These controls were matched with the CVST group for age and sex. The study protocol was registered and approved by the ethics committee of Zahedan University of Medical Sciences under the code IR.ZAUMS.REC.1401.223, and written informed consent was provided by all participants. Data were collected using information from the patients' medical records, including MRI reports, demographic data, and patient laboratory results. The control group was then selected from individuals referred to the Ali Ibn Abitaleb Hospital according to the inclusion criteria. Descriptive statistics, including mean, median, standard deviation, and interquartile range, were utilized to describe the data. The independent samples t-test and the Mann-Whitney U test were employed to determine the correlation between variables. To reduce the risk of bias, the data analysts were blinded to the group allocation (CVST or control) during the analysis process. All data analysis and statistical tests were conducted using SPSS version 24, with statistical significance defined as a P-value of less than 0.05.
4. Results
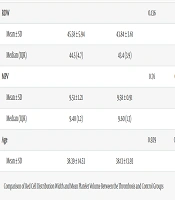
Forty-one patients in the thrombosis group and fifty-five patients in the non-thrombosis group were included in the study. There were 19 males (34.5%) in the non-thrombosis group and 14 males (34.1%) in the thrombosis group. The minimum age of the study participants was 10 years, and the maximum age was 74 years. The mean age of the study participants was 38.24 years, with a standard deviation of 14.11. Among the participants in the CVST group, 85.4% presented with headache, 41.5% with hemiparesis, 22% with seizures, 24.4% with a decreased level of consciousness, and 22% with papilledema. Regarding the location of thrombosis within the cerebral venous sinuses in the CVST group, 73.2% of participants exhibited transverse sinus involvement, 34.1% sagittal sinus involvement, 48.8% sigmoid sinus involvement, 12.4% cavernous sinus involvement, 4.9% straight sinus involvement, and 12.4% superficial cortical sinus involvement. The minimum RDW was 36.3, and the maximum RDW was 56. The mean RDW was 44.59, with a standard deviation of 4.80. The minimum MPV was 6.8, and the maximum MPV was 12.5 among the study participants. The mean MPV was 9.55, with a standard deviation of 1.04. The mean RDW of the CVST group (mean = 45.58, median = 44.5, SD = 5.94, interquartile range = 4.7) was compared with the control group (mean = 43.84, median = 43.4, SD = 3.61, interquartile range = 3.9). Based on the results of this comparison, the difference between the two groups was not statistically significant (P = 0.136), indicating no significant difference in mean RDW between the CVST group and the control group. The mean MPV of the CVST group (mean = 9.51, median = 9.40, SD = 1.21, interquartile range = 1.2) was compared with the control group (mean = 9.58, median = 9.60, SD = 0.91, interquartile range = 1.3). Based on the results of this comparison, the difference between the two groups was not statistically significant (P = 0.76), indicating no significant difference in mean MPV between the CVST group and the control group (Table 1).
| Variables | Sinus Venous Thrombosis | Control | P-Value | Effect Size |
|---|---|---|---|---|
| RDW | 0.136 | 0.15 | ||
| Mean ± SD | 45.58 ± 5.94 | 43.84 ± 3.61 | ||
| Median (IQR) | 44.5 (4.7) | 43.4 (3.9) | ||
| MPV | 0.76 | 0.63 | ||
| Mean ± SD | 9.51 ± 1.21 | 9.58 ± 0.91 | ||
| Median (IQR) | 9.40 (1.2) | 9.60 (1.3) | ||
| Age | 0.929 | 0.019 | ||
| Mean ± SD | 38.39 ± 14.53 | 38.13 ± 13.93 |
Abbreviations: RDW, red cell distribution width; SD, standard deviation; IQR, interquartile range; MPV, mean platelet volume.
5. Discussion
This study found no statistically significant difference in RDW between the CVST and control groups (P = 0.136). Inconsistent with our finding, Demir et al. reported significantly elevated RDW in patients with CVST compared to those with primary headaches (11). Maino et al. reported that individuals with RDW values above the 90th percentile had an approximately four-fold increased risk of CVT compared with those at or below the 90th percentile (12). However, our results do not align with those of Maino et al. Likewise, Ani and Ovbiagele observed significantly higher mean RDW in individuals with stroke compared to those without, suggesting that increased RDW is associated with stroke and predicts the severity of cardiovascular diseases and cerebrovascular events (13). Inconsistent with our finding, Balta et al. reported that RDW is a highly valuable marker in the diagnosis of CVST (14). Regarding MPV, our study found no statistically significant difference in mean MPV between the CVST and control groups (P = 0.76). In a similar study, Zhang et al. found lower MPV levels in the CVST group compared to the control group, suggesting that MPV may not be a reliable marker of inflammation and could decrease during the acute inflammatory phase (15). Consistent with our finding, Saglam demonstrated slightly higher platelet count, PDW, MPV, and MPV/plt ratio in the control group, although the differences between groups were not statistically significant, concluding no difference between patient and control groups (16). Madineni et al. also reported similar MPV and Plateletcrit levels in both severe and non-severe CVST groups, with no impact on outcomes, further supporting the present study's findings (17). However, Kamisli reported significantly increased MPV levels in CVST patients with brain parenchymal lesions, which contradicts our results (18). Although our study did not identify significant associations, future research is recommended to investigate temporal changes in RDW and MPV in order to assess their potential roles in prognosis and treatment response. One of the limitations of the present study was the inability to perform subgroup analyses based on factors such as the anatomical location of thrombosis or the severity of clinical symptoms. Expanding the study population and concurrently evaluating potential confounding variables — including comorbid conditions (e.g., infections, inflammatory diseases), medication use, lifestyle factors, vitamin status, and inflammatory markers — is also advised. Furthermore, future studies should consider matching additional laboratory parameters, such as hemoglobin and mean corpuscular volume (MCV), between groups to reduce potential biases and enhance the reliability of the results.
5.1. Conclusions
The RDW and MPV did not differ significantly between the CVST and control groups. It is suggested that, considering the potentially irreversible sequelae of CVST, MR venography/CT venography (MRV-CTV) should be employed as the diagnostic gold standard in any patient presenting with atypical headache, focal neurological deficits, seizures, altered mental status, or coma.