1. Background
Diabetes is a collective term used to describe a group of diseases characterized by elevated glucose levels in the blood. This condition arises from a deficiency in either the production or function of insulin, or both (1). Diabetes is categorized into two types: Type 1 and type 2. The etiology of type 2 diabetes is well-established, involving various genetic factors and the influence of multiple determinants. Prevention and treatment of type 2 diabetes entail the removal or reduction of these factors (2).
Type 1 diabetes mellitus (T1DM) is a chronic condition marked by insulin deficiency resulting from the loss of pancreatic β-cells. It accounts for 5% to 15% of all cases of diabetes and is often seen in children. Type 1 diabetes mellitus is associated with elevated blood glucose levels, a condition known as hyperglycemia. The etiology of T1DM remains incompletely understood, and effective prevention strategies have yet to be defined. Recently, a proposal has been made to screen families at risk for T1DM for autoantibodies (3).
A systematic review conducted in 2020 reported a global prevalence rate of 9.5 cases of T1DM per 10,000 individuals. The incidence rate of this condition in America and Europe was 12.2 per 10,000 individuals. In Africa, the incidence rate was 3.5 per 10,000 individuals, and in Asia, it was 6.9 per 10,000 individuals (4). The proportion of T1DM in Iran has been reported to be 11.4% (5). Other findings indicate that over a span of 12 years, specifically from 1999 to 2010, the incidence of T1DM exhibited a mean annual growth rate of 0.08% (6).
The complications associated with diabetes primarily involve microvascular complications, including nephropathy, retinopathy, and neuropathy (7-9). These complications are directly influenced by glycemic control. Additionally, careful glycemic control can help prevent delayed macrovascular effects in individuals with T1DM (7). Diabetes-related autonomic neuropathy may affect ocular structures such as the cornea, lacrimal gland, and retina (9). A study revealed that individuals with T1DM demonstrated a significant decrease in Schirmer test results, a rise in intraocular pressure, and a reduction in retinal thickness compared to a control group of the same age (9). Also, in a study in Iran, the rate of diabetic retinopathy was reported to be 21.9% (5). Children diagnosed with T1DM face an increased susceptibility to developing diabetic neuropathy and retinopathy. If left undetected and untreated, these conditions can lead to visual impairments and potentially result in blindness (9).
Ethnicity and environmental factors play an important role in the occurrence of diseases. Previous research has demonstrated that environmental factors and ethnicity contribute substantially to the prevalence of diabetes (6) and its associated complications (10). According to regional data, it is evident that certain regions, such as North Africa and the Middle East, have a high public health burden of diabetes. Minorities in the United States exhibit a higher propensity for developing microvascular complications of diabetes and experiencing lower limb amputations, which can potentially contribute to disability (10). Cataracts, as one of the ocular complications of diabetes, are associated with environmental factors such as exposure to solar ultraviolet radiation and living in tropical areas (11-13).
Considering the influence of environmental factors on diabetes complications, this study intended to assess the ocular complications of T1DM in Zahedan, a tropical region in southeastern Iran. The study’s findings can have practical implications for the implementation of screening and healthcare programs for individuals with T1DM. More specifically, these results can aid in the early identification of ocular complications in this population and in the management of factors that contribute to the worsening of these complications.
2. Objectives
The present study aimed to assess the ocular complications of T1DM in Zahedan, a tropical region in southeastern Iran.
3. Methods
The study adhered to the principles required by the Declaration of Helsinki and obtained approval from the Ethics Committee affiliated with Zahedan University of Medical Sciences (IR.ZAUMS.REC.1401.097). Furthermore, an informed consent form was signed by all participants or their legal guardians.
In this retrospective, single-center cross-sectional study conducted at Al-Zahra Eye Hospital in 2023 - 2024, patients with type 1 diabetes were referred from a private office of an endocrinologist. Inclusion criteria were patients with T1DM and no other preexisting ocular or systemic diseases such as hypertension and hyperlipidemia. Subjects who had chronic or recurrent inflammatory eye diseases, a history of ocular surgery or laser therapy, intraocular trauma, or who were currently using any ophthalmic or systemic steroid were excluded from the study.
All patients received ophthalmic and physical examinations, including a thorough assessment of their current medication usage and medical history. Dilated binocular indirect ophthalmoscopy with a +90 D condensing lens and slit-lamp biomicroscopy were performed to examine the retina and anterior segment of the eye for any signs of ocular complication in all patients. The best corrected distance visual acuity (VA) was assessed using the Snellen chart at a distance of 6 meters under standard light conditions. Visual acuity was recorded as logMAR. If patients did not have ocular complications, VA in the right eye was recorded; if they had ocular complications, VA with the most severe complication was recorded.
Venous blood samples were collected to measure glycosylated hemoglobin (HbA1c) levels. The HbA1c is a measure of the mean blood glucose concentration over the previous 2 - 3 months, serving as an indicator of the effectiveness of diabetes treatment. Elevated HbA1c levels beyond the range of 4% - 6.4% typically indicate inadequate control of blood glucose. The study collected data on gender, age, diabetes mellitus onset, and HbA1c levels.
3.1. Statistical Analysis
The analyses were conducted using SPSS version 17 statistical software (SPSS Inc., Chicago, IL, USA). The statistics were reported descriptively as mean ± standard deviation (SD), 95% confidence interval (CI), and percentage. The Kolmogorov-Smirnov test was used to check the normality of quantitative data. An independent t-test was employed to compare the diabetes duration, age, and HbA1c levels in the two groups with and without ocular complications. The Mann-Whitney test was used to analyze qualitative and nonparametric variables. Additionally, binary logistic regression analysis for variables of age, HbA1c, duration, and onset age of diabetes was utilized to determine the adjusted odds ratio (OR). The level of significance was established as P < 0.05.
4. Results
Seventy-six patients with T1DM, comprising 39 males and 37 females, who met the inclusion criteria were enrolled in the study using a convenience sample. Their mean age was 11.93 ± 3.76 years (range: 4 - 18 years). The average diabetes duration was 4.69 ± 2.53 years (range: 1 - 11 years). The mean HbA1c level was 10.16 ± 2.39. Among the 76 patients diagnosed with diabetes, ocular complications were present in 25% (19 individuals). Moreover, 6.6% (n = 5) exhibited mild nuclear cataracts with VA of 0.02 ± 0.09 logMAR, 14.5% (n = 11) suffered from mild anterior and posterior sub-capsular opacity with VA of 0.01 ± 0.08 logMAR, and 3.9% (n = 3) displayed mild diabetic retinopathy with VA of 0.01 ± 0.05 logMAR. The remaining 75% (n = 57) did not have any ocular complications (VA: -0.07 ± 0.13 logMAR). There was no significant difference in VA among these complications and patients without complications (P = 0.053).
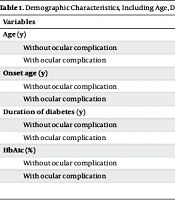
Table 1 details the demographic characteristics, including age, disease duration, and HbA1c level, of individuals categorized into two groups: Those with and those without ocular complications. The independent t-test results indicated a significant difference between the groups in age (P = 0.01) and disease duration (P = 0.04). Nevertheless, no significant difference was observed in HbA1c levels (P = 0.22). Furthermore, no statistically significant difference in ocular complications was observed between males and females (P = 0.35).
| Variables | Mean ± SD | 95% CI | P-Value |
|---|---|---|---|
| Age (y) | 0.01 | ||
| Without ocular complication | 13.65 ± 3.65 | 12.01 - 15.29 | |
| With ocular complication | 11.18 ± 3.35 | 10.29 - 12.11 | |
| Onset age (y) | 0.16 | ||
| Without ocular complication | 8.10 ± 3.82 | 5.84 - 7.62 | |
| With ocular complication | 6.82 ± 3.31 | 6.47 - 9.89 | |
| Duration of diabetes (y) | 0.04 | ||
| Without ocular complication | 4.39 ± 2.47 | 3.74 - 5.07 | |
| With ocular complication | 5.64 ± 2.59 | 4.53 - 6.88 | |
| HbA1c (%) | 0.22 | ||
| Without ocular complication | 9.60 ± 1.58 | 8.80 - 10.29 | |
| With ocular complication | 10.15 ± 2.22 | 9.55 - 10.76 |
Demographic Characteristics, Including Age, Disease Duration, and Glycosylated Hemoglobin Level in Groups with and Without Ocular Complications
The multiple regression analysis indicated that age (adjusted OR: 1.32, 95% CI: 1.04 - 1.68, P = 0.019) and duration of diabetes (OR: 1.32, 95% CI: 1.04 - 1.68, P = 0.01) were significant risk factors for ocular complications. The OR for HbA1c (OR: 1.21, 95% CI: 0.92 - 1.57, P = 0.15) and onset age (OR: 0.90, 95% CI: 0.71 - 1.14, P = 0.39) did not show statistical significance.
5. Discussion
The global incidence of diabetes is on the rise, leading to heightened apprehension regarding the emergence of chronic complications that amplify disability and affect quality of life. The study findings indicate that a quarter of individuals with T1DM in Zahedan experienced ocular complications, with the prevailing occurrence being anterior and posterior sub-capsular opacity without a statistically significant reduction in VA. Approximately 21.1% of the participants below 18 years with a disease duration of 4.5 years experienced cataracts associated with T1DM. The incidence rate of nuclear cataracts was found to be 6.6%, while the prevalence of anterior and posterior sub-capsular opacity was 14.5%. The high prevalence of cataracts obtained in this study was without a statistically significant decrease in VA. Although the P-value for VA was very close to 0.05, which may become significant with a larger sample size, the VA obtained in the cataract groups compared to the group without ocular complications showed a difference of less than one line, which does not indicate a clinically significant difference.
The occurrence of cataracts in individuals with early-onset diabetes varies depending on age, ranging from 0.7% to 13.9%, and this prevalence tends to increase as age increases (14). Diabetic cataracts frequently manifest as an initial indication of T1DM or develop shortly after the diagnosis of T1DM (15-17). Diabetic cataracts can either be permanent or temporary, with the latter being resolved through enhanced glycemic control (18). Cataract development has been linked to hyperglycemia and ketoacidosis (18). The development of early-stage cataracts appears to be influenced by multiple factors, such as gender, genetics, nutrition, region, and growth (11, 15). Prior research has indicated a positive correlation between the prevalence of cataracts and environmental factors such as elevated temperatures, decreased humidity levels, and increased exposure to solar ultraviolet radiation (11, 12). The increased prevalence of cataracts in tropical regions compared to subtropical regions has been shown in previous studies (12, 13). The higher frequency of cataracts observed in the present study compared to previous research may be due to the tropical nature of the study region. Zahedan, a city in Sistan and Baluchestan province, located in southeastern Iran, has a hot and dry desert climate, with temperatures above 27°C more than 70% of the time (19). It should be noted that the high prevalence of cataracts obtained in this study may differ in other regions with different environmental factors, genetic backgrounds, and access to healthcare.
Due to the significant occurrence of cataracts associated with diabetes in Zahedan, it is imperative to implement eye screening initiatives in the healthcare system. Previous research has indicated that cataracts can manifest as an ocular complication shortly after the diagnosis of T1DM but can potentially be resolved through effective diabetes management. Therefore, early detection of cataracts in T1DM patients is crucial, warranting the implementation of annual screening programs.
The study findings indicated a prevalence rate of 3.9% for mild non-proliferative diabetic retinopathy among the patients. Consistent with these findings, further investigations revealed a prevalence of 2.4% and 4.8% of mild non-proliferative diabetic retinopathy in young diabetic patients under 18 with a mean diabetes duration of 4.8 years (9, 20). Another investigation was conducted on individuals aged 18 to 60 with T1DM who had developed the disease before the age of 40. The study found that the prevalence of each type of diabetic retinopathy was 27.4%, with severe retinopathy reported in 8% of the participants (21). The disparity in findings between Hammes et al.’s study (21) and our study may be attributed to patient age differences. Specifically, the patients in our study were under 18 years old, whereas Hammes’ study included patients under 60 years old.
The findings of our study indicate a statistically significant association between age, duration of diabetes, and the occurrence of ocular complications. Previous research has shown a consistent relationship between age and ocular complications in patients with T1DM (21). Additionally, the duration of diabetes has been noted as a significant risk factor for ocular complications, including diabetic retinopathy and cataracts (14, 21, 22). Higher HbA1c levels are considered a risk factor for cataracts and diabetic retinopathy in T1DM (22-24). In this study, although the OR showed a positive association between higher HbA1c levels and an increased likelihood of ocular complications, this association was not statistically significant. A possible reason for this finding could be the single-point measurement of HbA1c compared with its long-term assessment.
The study findings indicate that cataract, specifically anterior and posterior subcapsular cataract, was the prevailing ocular complication among individuals with T1DM in the tropical city of Zahedan. The high prevalence of cataracts obtained in this study was without a statistically and clinically significant decrease in VA. The incidence of ocular complications was significantly linked to the disease’s duration and the patients’ age. Hence, it is imperative to incorporate strategic planning in the healthcare systems to implement annual eye screening programs aimed at early detection of ocular complications in individuals with T1DM.
5.1. Limitations
This study had some limitations. One of the limitations is the sample size, which was relatively small to investigate the prevalence of ocular complications and identify specific risk factors in diabetic patients. Another limitation is the cross-sectional nature of the study, which can only show an associative relationship, not a causative relationship between variables, and cannot definitively prove that these factors cause complications. Also, in cross-sectional studies, it is difficult to determine the temporal sequence of events, such as the priority of the effect of the duration of diabetes or the duration of poor blood sugar control on ocular complications. Another limitation of this study was the lack of classification of cataract severity, which does not allow for a more accurate assessment of the relationship between cataract severity and risk factors. Although risk factors such as gender, age, HbA1c, onset, and duration of diabetes were examined in this study, other potential risk factors such as nutrition, sunlight exposure, smoking status, genetic predisposition, and socio-economic factors such as low income and limited access to healthcare were not assessed. Therefore, it is recommended that future studies be conducted as cohort studies with larger sample sizes to accurately investigate the risk factors and the temporal sequence of these risk factors on ocular complications and their severity.