1. Background
Multiple pregnancies can occur due to various mechanisms: The fertilization of two or more eggs, a single fertilization followed by an abnormal division of the zygote, or a combination of these processes. These pregnancies are associated with a significantly higher risk of preterm birth, affecting 60% of twin, 90% of triplet, and nearly all quadruplet pregnancies. The global incidence of multiple pregnancies has increased since the 1980s, largely due to advancements in assisted reproductive technologies (ARTs) (1). However, this rise is concerning, as multiple gestations contribute to higher perinatal mortality, congenital anomalies, and long-term neonatal morbidities (2). From a maternal perspective, multiple pregnancies pose greater risks than singleton pregnancies, including twice the likelihood of preeclampsia, postpartum hemorrhage, and maternal mortality. The risk of peripartum hysterectomy and postpartum depression is also elevated. Given these challenges, understanding the epidemiology and contributing factors of multiple pregnancies is essential for maternal and neonatal health management (3, 4).
Epidemiological studies estimate that 1.25% of all pregnancies worldwide result in twins, with significant racial and geographic disparities. Twin pregnancies are most prevalent among African American women (3.5%) and least common among Caucasian women (0.3%), with lower rates reported in Latin American, Asian, and Native American populations. These differences may be linked to variations in follicle-stimulating hormone (FSH) levels, which influence ovarian follicle development (5).
Several factors influence the likelihood of twinning. The incidence of dizygotic twin pregnancies increases fourfold between the ages of 15 and 37, due to both natural increases in FSH stimulation and the greater use of ART in older women. Additionally, maternal parity significantly affects multiple gestations, with multiparous women having up to 20 times higher odds of conceiving twins compared to primiparous women (6). Genetic predisposition also plays a role, as maternal family history of twinning is a stronger predictor than paternal history, with potential links to specific regions on chromosome 6 (7). Beyond genetics, nutritional status and body composition may contribute to twin pregnancies. Studies suggest that taller and heavier women are 25 - 30% more likely to conceive twins than shorter women with a history of nutritional deficiencies. The role of FSH levels as a common determinant connecting race, age, body weight, and fertility has been widely debated. Evidence also suggests that women who conceive within one month of discontinuing oral contraceptives exhibit higher dizygotic twinning rates, further supporting the FSH hypothesis (8, 9).
The ART has significantly influenced the frequency of multiple pregnancies. The use of FSH in combination with chorionic gonadotropin or clomiphene citrate enhances the likelihood of multiple ovulations. Infertility treatments such as ovarian stimulation, intrauterine insemination (IUI), and in vitro fertilization (IVF) have contributed to the rising rates of twins and higher-order multiples. However, in women under 35 with favorable prognoses, transferring more than two embryos during IVF is discouraged to minimize multiple gestations (10). Epidemiological data from Iran reflect a rising trend in multiple pregnancies, consistent with global patterns. For instance, a cross-sectional survey of over 5,170 deliveries in Tehran reported a twin-multiple pregnancy prevalence of 1.48%, with maternal age, ART use, and family history identified as significant predictors (11). In Isfahan, registry data from 2009 - 2010 showed 17.6 twin births, 1.8 triplet births, and 0.03 quadruplet births per 1,000 deliveries (12). A study in Hamadan (2016 - 2017) identified a multiple pregnancy incidence of 3.3% (1.7% twins, 0.39% triplets, 0.11% quadruplets), with ART strongly linked to prematurity and neonatal complications (13).
Internationally, similar findings have been observed: A multicenter Chinese study reported that multiple gestations are associated with significantly higher rates of preterm birth and low birth weight (14). Although multiple pregnancies have been extensively studied worldwide, region-specific data from Iran — particularly from the southeastern provinces — remain scarce. This study was conducted at Ali-ibn-Abi-Talib Hospital in Zahedan, the only specialized obstetrics and gynecology referral center in the region, to determine the prevalence of twin and multiple pregnancies and to identify associated maternal and clinical factors between 2015 and 2018. The primary objective was to estimate the prevalence of multiple pregnancies, while secondary objectives included examining the influence of maternal age, family history, conception type, parity, and delivery method. We hypothesized that maternal age and family history would significantly predict the occurrence of multiple pregnancies. Although there was no strong prior evidence suggesting that this region would differ significantly from national or global trends, the distinct demographic, ethnic, and healthcare characteristics of southeastern Iran — such as higher fertility rates, low ART utilization, and limited access to specialized care — warranted investigation.
2. Objectives
The present study aims to clarify several underexplored aspects, including the true prevalence of spontaneous multiple pregnancies, their distribution across maternal age groups, and trends in delivery practices. By addressing these ambiguities, the study fills a critical knowledge gap and offers evidence to guide region-specific maternal health planning, education, and obstetric care strategies in underserved populations. Based on the study objectives and regional context, we expected to: (1) Quantify the prevalence of multiple pregnancies in this underrepresented population, (2) identify maternal and clinical predictors such as age, parity, and family history, (3) clarify the contribution of spontaneous versus assisted conception in a low-ART-use setting, and (4) provide context-specific evidence to inform targeted prenatal care and health policy in southeastern Iran.
3. Methods
This descriptive cross-sectional study examined the prevalence and associated factors of twin and multiple pregnancies among women who delivered at Ali-ibn-Abi-Talib Hospital in Zahedan between 2015 and 2018. This hospital, as the largest specialized obstetric and gynecologic referral center in southeastern Iran, serves a diverse population, including patients from rural and underserved regions of Sistan and Baluchestan province. Given its status as a university-affiliated teaching hospital, it provides comprehensive maternity care, making it an appropriate setting for studying trends in multiple pregnancies. The time period from 2015 to 2018 was selected because it represented the most recent complete and accessible set of delivery records available at the time of data collection, ensuring data quality and consistency across all variables of interest.
All available cases of multiple pregnancies were included through a census of hospital records. The data were extracted from standardized medical records maintained at Ali-Ibn-Abi-Talib Hospital. These records included structured forms filled out by attending physicians and midwives at the time of delivery. The validity of these data is supported by the fact that the records are routinely used for clinical care and reporting purposes, which ensures that they accurately reflect the maternal and neonatal characteristics. To enhance reliability, data extraction was performed by the primary investigator and cross-checked by an independent reviewer. Any discrepancies were resolved through discussion and verification with the hospital’s obstetric care team. This double-review process minimized errors and ensured consistency in data collection.
Exclusion criteria were applied to ensure data reliability and included cases with incomplete or missing medical records, particularly those lacking information on maternal age, pregnancy history, or delivery method. After obtaining ethical approval from the Research Ethics Committee of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1399.036), the researcher accessed the hospital’s medical archives and retrieved patient records with official authorization. Each record was carefully reviewed to extract maternal and neonatal data, including maternal age, family history of twinning, pregnancy type (spontaneous vs. ART), mode of delivery (cesarean section vs. vaginal delivery), parity, and neonatal gender distribution. Given the region’s low ART utilization rate, special attention was paid to identifying cases involving assisted conception.
Patient confidentiality was maintained by assigning anonymous numerical codes to records, and no personally identifiable information was extracted. The research was carried out exclusively using retrospective hospital records, and no direct patient contact was involved. The collected data were analyzed using SPSS software (version 26). Descriptive statistics were employed to summarize maternal characteristics, pregnancy outcomes, and delivery methods. Continuous variables, such as maternal age, were reported as means and standard deviations, while categorical variables, including pregnancy type, parity, and newborn gender, were expressed as frequency counts and percentages. Comparative analyses between twin and triplet pregnancies were conducted using chi-square tests for categorical variables and independent t-tests for continuous variables, with a significance level set at P < 0.05.
4. Results
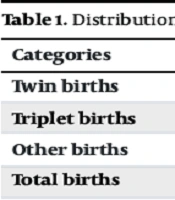
In this study, a total of 25,425 births were analyzed, of which 253 were twin births (0.99%) and 14 were triplet births (0.01%), while the remaining 25,158 births (99.0%) were singletons (Table 1). The distribution of multiple births within the study population highlights their relative rarity.
| Categories | No. (%) |
|---|---|
| Twin births | 253 (0.99) |
| Triplet births | 14 (0.01) |
| Other births | 25,158 (99.0) |
| Total births | 25,425 (100.0) |
4.1. Maternal and Demographic Characteristics
As shown in Table 2, the majority of births occurred in 2015 (40.0%), followed by 2016 (36.0%), 2017 (15.0%), and 2018 (9.0%). Maternal age was predominantly concentrated in the 21 - 30 years group, accounting for 55.0% of the cases, while 8.0% of mothers were under 20 years of age, 33.0% were between 31 and 40 years, and 4.0% were older than 40 years. A family history of multiple births was absent in 86.0% of the cases, with only 14.0% reporting a familial predisposition to multiple pregnancies.
| Categories | No. (%) |
|---|---|
| Year of birth | |
| 2015 | 41 (15.0) |
| 2016 | 106 (40.0) |
| 2017 | 95 (36.0) |
| 2018 | 25 (9.0) |
| Maternal age (y) | |
| < 20 | 21 (8.0) |
| 21 - 30 | 148 (55.0) |
| 31 - 40 | 88 (33.0) |
| > 40 | 10 (4.0) |
| Family history | |
| Present | 37 (14.0) |
| Absent | 230 (86.0) |
4.2. Newborn Gender Distribution
As presented in Table 3, among twin births, the most common gender combination was one boy and one girl, which accounted for 37.15% of cases. This was followed by two girls (33.99%) and two boys (28.85%). In triplet births, the most frequent combination was three girls (35.71%), followed by two girls and one boy (28.57%), three boys (21.43%), and two boys and one girl (14.26%).
| Categories | No. (%) |
|---|---|
| Twins | |
| Two boys | 73 (28.85) |
| Two girls | 86 (33.99) |
| One boy and one girl | 94 (37.15) |
| Total | 253 (100) |
| Triplets | |
| Three boys | 3 (21.43) |
| Three girls | 5 (35.71) |
| Two girls, one boy | 4 (28.57) |
| Two boys, one girl | 2 (14.26) |
| Total | 14 (100) |
4.3. Maternal Age and Delivery Method
As indicated in Table 4, the maternal age distribution for twin and triplet pregnancies showed that the majority of mothers were aged 20 - 30 years, accounting for 55.3% of twin pregnancies and 57.1% of triplet pregnancies. Mothers aged 31 - 40 years represented 32.4% of twin births and 42.9% of triplet births. The predominant mode of delivery was cesarean section, with 74.7% of twin births and 71.4% of triplet births delivered through this method. Vaginal delivery was less common, occurring in 25.3% of twin births and 28.6% of triplet births.
| Categories | Twins | Triplets | Total |
|---|---|---|---|
| Maternal age group (y) | |||
| < 20 | 21 (8.3) | 0 (0.0) | 21 (7.9) |
| 20 - 30 | 140 (55.3) | 8 (57.1) | 148 (55.3) |
| 31 - 40 | 82 (32.4) | 6 (42.9) | 88 (32.9) |
| > 40 | 10 (4.0) | 0 (0.0) | 10 (3.7) |
| Mode of delivery | |||
| Vaginal delivery | 64 (25.3) | 4 (28.6) | 68 (25.5) |
| Cesarean section | 189 (74.7) | 10 (71.4) | 199 (74.5) |
| Pregnancy type | |||
| Spontaneous | 251 (99.2) | 14 (100.0) | 265 (99.2) |
| Art | 2 (0.8) | 0 (0.0) | 2 (0.8) |
| Parity (birth order) | |||
| First | 42 (16.6) | 6 (42.9) | 48 (18.0) |
| Second | 17 (6.7) | 5 (35.7) | 22 (8.1) |
| Third | 42 (16.6) | 0 (0.0) | 42 (15.8) |
| Fourth | 79 (31.2) | 0 (0.0) | 79 (29.6) |
| Fifth | 30 (11.8) | 3 (21.4) | 33 (12.4) |
| Sixth | 5 (2.0) | 0 (0.0) | 5 (1.9) |
| Seventh | 1 (0.4) | 0 (0.0) | 1 (0.4) |
| Eighth | 11 (4.3) | 0 (0.0) | 11 (4.1) |
| Ninth | 19 (7.5) | 0 (0.0) | 19 (7.1) |
| Tenth | 7 (2.8) | 0 (0.0) | 7 (2.6) |
Abbreviations: ART, assisted reproductive technology.
a Values are expressed as No. (%).
Nearly all cases of multiple pregnancies were spontaneous (99.2% for twins and 100.0% for triplets), with ART contributing to 0.8% of twin pregnancies and none of the triplet pregnancies. First births accounted for 42.9% of triplet pregnancies and 16.6% of twin pregnancies. Parity beyond the fourth birth was relatively uncommon, with fifth and higher-order births comprising 28.6% of triplet pregnancies and 34.2% of twin pregnancies. The mode of delivery and pregnancy type did not differ significantly between twins and triplets (P = 1.0, chi-square test). However, the distribution of parity showed a statistically significant difference between twins and triplets (P = 0.033, chi-square test), with first births being more common among triplet pregnancies.
5. Discussion
This study focused on assessing the prevalence and contributing factors of multiple pregnancies in southeastern Iran. We analyzed 25,425 births, which included 253 twin births and 14 triplet births, with the remaining 25,158 births being singletons. Our findings revealed that twin pregnancies accounted for 0.99% of all births, and triplet pregnancies were less common, comprising only 0.01% of the total births in the cohort. These results are consistent with global trends in multiple pregnancy rates, where twin pregnancies typically account for 2 - 4% of all births, and higher-order multiple pregnancies remain comparatively rare (2, 15).
While the increased use of ART in some parts of the world has contributed to higher rates of multiple pregnancies, particularly twin and higher-order pregnancies, our findings suggest that, in Zahedan, spontaneous multiple pregnancies remain predominant, with 99.2% of twin pregnancies and 100% of triplet pregnancies occurring naturally. This reveals the importance of understanding regional differences in the prevalence of ART use and its impact on multiple pregnancies.
One of the most noticeable findings of this study is the significant association between maternal age and the occurrence of multiple pregnancies. The highest prevalence of multiple pregnancies was observed in women aged 21 - 30 years, with a notable increase in the incidence of multiple births among women aged 31 - 40 years. This finding is consistent with established research suggesting that older maternal age is a key determinant of the likelihood of multiple pregnancies, especially dizygotic twins. As maternal age increases, so does the hormonal stimulation of ovarian follicles, which contributes to the increased likelihood of multiple ovulation and subsequent multiple pregnancies (16, 17). Moreover, studies have shown that gonadotropin levels — which are naturally elevated in older women — play a critical role in the increased incidence of multiple ovulation, leading to higher rates of dizygotic twins (18).
Our study also confirmed the significant association between multiple pregnancies and family history. In our cohort, 14% of women with multiple pregnancies reported a family history of such births, which supports findings from previous studies (19). This familial predisposition, especially when it pertains to the maternal side, may be due to genetic factors that influence follicular development and ovulation (20). In addition, specific genetic regions have been linked to increased twinning, further reinforcing the role of genetics in the occurrence of multiple pregnancies (21).
The study’s results indicate that cesarean section was the predominant mode of delivery for both twin (74.7%) and triplet (71.4%) pregnancies. This is consistent with the well-established fact that multiple pregnancies are associated with a higher risk of preterm labor, fetal distress, and malpresentation (22, 23). Cesarean delivery is often required to mitigate these risks and ensure the safety of both mother and child. The high rates of cesarean delivery observed in this study further underscore the need for specialized obstetric care and management strategies tailored to multiple pregnancies (24).
Interestingly, the contribution of ARTs to the incidence of multiple pregnancies in our study was minimal, with only 0.8% of twin pregnancies attributed to ART. This contrasts with findings from Western countries, where ART is a significant factor contributing to the rise in multiple pregnancies, particularly in the context of ovarian stimulation and IVF (25). The lower use of ART in our study may reflect regional differences in access to and utilization of fertility treatments, as well as cultural and socioeconomic factors that influence reproductive practices. In countries with higher ART utilization, the incidence of multiple pregnancies has increased significantly resulting from ovarian stimulation (26).
Our results also confirm the findings of a previous study conducted in Iran (including 5,170 mothers in labor from 103 hospitals with obstetrics and gynecology wards), which stated that the multiple pregnancy rate was 1.48%. They reported the remarkable link between multiple pregnancy and mother’s age as well as ART (11). While their study indicated that ART was associated with a sixfold increase in the odds of twin pregnancies (OR = 6.1), the proportion of ART-related cases in our study was only 0.8%.
Moreover, when comparing our results with broader Iranian data, the prevalence of spontaneous twin pregnancies in our cohort (99.2%) is notably higher than in Isfahan, where approximately 30% of multiple births were associated with ART (12). The U.S. surveillance data indicate that ART contributes to approximately 12.5% of all multiple births, and outcomes research highlights higher rates of prematurity and fetal mortality among ART-related multiples compared to spontaneous ones (e.g., prematurity ~ 72% in IVF twins vs. ~ 70% naturally conceived) (27). These comparisons suggest that while ART plays a dominant role in multiple gestations in other regions, our findings underscore predominant natural conception in Zahedan — a disparity likely reflecting regional healthcare access, socioeconomic context, and fertility practices.
5.1. Conclusions
In conclusion, this study sheds light on the prevalence of multiple pregnancies in Zahedan, Iran, revealing that twin pregnancies account for 0.99% of all births, while triplet pregnancies are rarer at 0.01%. The findings show the role of maternal age, family history, and spontaneous conception as key factors in the occurrence of multiple pregnancies. Notably, ART played a minimal role in our study, suggesting that regional differences in ART usage may contribute to variations in multiple pregnancy rates. The high incidence of cesarean deliveries among mothers of multiple births emphasizes the need for targeted prenatal care and delivery planning.
5.2. Limitations
While this study provides valuable insights, several limitations must be acknowledged. Firstly, the cross-sectional design prevents us from making conclusions about cause-and-effect relationships. Specifically, we cannot establish whether factors such as maternal age, the use of ART, or a family history of multiple pregnancies directly lead to multiple pregnancies. Since the data was collected at a single point in time, we cannot determine whether these factors occurred before or after the multiple pregnancies, which limits our ability to assess their true impact. Secondly, this study did not differentiate between monozygotic (identical) and dizygotic (fraternal) twins, which would have provided more detailed information on the underlying mechanisms of multiple pregnancies. Additionally, postnatal complications in both mothers and newborns were not assessed, and the study was limited by the availability of clinical data on maternal health during pregnancy and pre-existing medical conditions.
5.3. Future Studies
Moreover, this study focused on analyzing the characteristics of multiple pregnancies but did not include a detailed comparative analysis with singleton pregnancies. While general delivery statistics were provided for context, future studies should include matched comparisons with singleton births to better identify factors uniquely associated with multiple gestations. Future research should address these gaps to offer a more comprehensive understanding of the short- and long-term outcomes of multiple pregnancies.
These findings have significant clinical implications for the management of multiple pregnancies and the prevention of adverse outcomes for both mothers and newborns. Future studies should further explore the genetic, hormonal, and environmental factors that influence the occurrence of multiple pregnancies and their long-term impact on maternal and neonatal health. It is essential to develop targeted prenatal care protocols, allocate resources for specialized obstetric care, and promote awareness of risks in multiple pregnancies.