1. Background
Early-onset sepsis (EOS), which usually appears within the first 72 hours of life, and late-onset sepsis (LOS), which appears after 72 hours of birth, are the two types of neonatal sepsis (NS), defined as a systemic infection occurring within the first 28 days of life (1). With an estimated 17% mortality rate, NS affects over 3 million babies worldwide each year (2). Particularly in low-income nations, the frequency is noticeably higher among neonates in need of critical medical care, preterm infants, low birth weight babies, those with perinatal hypoxia, and those experiencing protracted hospitalization (3). Clinical manifestations of NS are often nonspecific and may include temperature instability, poor feeding, respiratory distress, lethargy, and in severe cases, failure to thrive or progression to septic shock (4). While sepsis affects fewer than 1 in 1,000 term infants, the incidence rises to 30% in preterm neonates (4). Meningeal involvement occurs in approximately 15% - 20% of NS cases, and the rate of neurological complications may range from 20% to 50% (4, 5).
Late-onset sepsis is often acquired in hospital settings (nosocomial) or the community, with an incidence of approximately 1.6% among term infants (6, 7). However, in preterm neonates, particularly those with very low birth weight and prolonged invasive interventions, the incidence can range from 12% to 50% (7). The mortality rate of LOS is estimated at 10% - 20%, rising to as high as 35% in infants weighing less than 1000 grams (8). Gram-positive organisms, including coagulase-negative staphylococci (CoNS), Staphylococcus aureus, and Enterococcus spp., are the predominant causes of LOS (9). In contrast, gram-negative bacteria such as Escherichia coli, Klebsiella spp., and Pseudomonas spp. tend to be more aggressive and are associated with higher mortality rates (10). Additionally, fungal pathogens like Candida spp. can cause systemic infections in extremely preterm neonates, particularly those exposed to prolonged broad-spectrum antibiotic therapy and central venous catheters (11).
Although blood culture remains the gold standard for diagnosing NS (11, 12), its diagnostic utility is limited by factors such as delayed results, potential for false negatives due to low bacteremia levels, and limited availability of rapid culture systems in resource-limited settings. Consequently, there is a growing reliance on adjunctive diagnostic markers that are inexpensive, rapid, and widely accessible. The most often used hematological indices are acute-phase reactants, the immature-to-total neutrophil ratio (I/T ratio), and the total leukocyte count. Important acute-phase reactants include procalcitonin (PCT), erythrocyte sedimentation rate (ESR), transferrin, fibronectin, prealbumin, haptoglobin, serum amyloid A, α1-acid glycoprotein (orosomucoid), fibrinogen, ceruloplasmin, and C-reactive protein (CRP) (2).
Notably, PCT has been a promising biomarker for early diagnosis of newborn sepsis in recent years. Procalcitonin levels increase between 2 and 4 hours after the start of an infection, peak between 6 and 12 hours later, and stay high in bacterial infections while remaining low in viral or inflammatory diseases not related to an infection (13). Procalcitonin is a useful screening and diagnostic test for newborn sepsis, according to several investigations (13). The advantages of using PCT include rapid elevation in bacterial infections, aiding early diagnosis, distinguishing bacterial from non-bacterial causes, facilitating targeted therapy, reducing unnecessary antibiotic use, promoting timely discharge, and decreasing healthcare costs. However, limitations also exist — PCT should be interpreted alongside clinical findings and other laboratory results, and transient elevations may occur in healthy neonates due to physiological changes post-birth (12, 13).
Given the clinical significance of CRP and PCT, the present study aims to compare their diagnostic performance in the early detection and monitoring of NS.
2. Objectives
The present study aimed to compare the diagnostic value and clinical utility of two major acute-phase reactants — CRP and PCT — in the early detection and follow-up of NS. By evaluating the sensitivity, specificity, and kinetics of CRP and PCT levels in neonates suspected of sepsis, this study seeks to determine which biomarker offers more accurate and timely information for clinical decision-making and antibiotic stewardship in neonatal care.
3. Methods
The present study was approved by the Ethics Committee of Mashhad University of Medical Sciences (IR.MUMS.REC.1386021) on 40 patients who were admitted to the neonatal intensive care unit (NICU) of Ghaem Hospital between December 2012 and December 2013 with a primary diagnosis of sepsis. This study comprised 40 term infants who were brought to the NICU with suspected sepsis and who were older than three days and weighed more than 2.5 kg. Infants with congenital anomalies, metabolic diseases, chromosomal syndromes, or those whose families did not consent were excluded from the study. All infants were suspected of NS according to the opinion of a neonatologist.
Infants with suspected sepsis had 2 cc of blood drawn for PCT and CRP tests prior to beginning empirical antibiotic treatment. Additionally, each patient had a blood culture and any other testing that the neonatologist deemed essential. Late-onset sepsis was defined as sepsis that developed three to thirty days after birth. All patients began receiving empirical treatment. To evaluate the response to treatment, CRP and PCT were measured both prior to and three days following the initiation of antibiotic treatment. The CRP and PCT values obtained on the third day of treatment to evaluate the response to treatment and before the start of antibiotics for diagnosis were compared.
Quantitative analysis was used to determine CRP levels, with significant values defined as those exceeding 5 mg/dL. Serum PCT measurements were carried out using the Roche Elecsys BRAHMS PCT kit and the electrochemiluminescence immunoassay (ECLIA) method (Roche Diagnostics GmbH, Germany), with significant values defined as those exceeding 2 ng/mL.
Blood samples from neonates suspected of sepsis were collected under sterile conditions and inoculated onto blood agar (Ibresco, Italy) culture media. After colony growth on appropriate media, Gram staining was performed to determine the bacterial type (gram-positive or gram-negative). Subsequently, classical biochemical tests were conducted for more precise bacterial identification. These tests included sugar fermentation assays such as arabinose, xylose, galactose, sorbitol, fructose, mannitol, mannose, rhamnose, raffinose, maltose, lactose, and sucrose. Additionally, enzymatic tests such as catalase, oxidase, urease, urea hydrolysis, and other related tests were performed for definitive bacterial identification (14).
SPSS version 23 was used to analyze all of the data (IBM Corp., Armonk, NY, USA). The mean ± standard deviation (SD) is used to display the data. To evaluate differences between two groups, an independent samples t-test was used. P-values below 0.05 were regarded as statistically significant.
4. Results
A sepsis work-up was performed on all 40 neonates in accordance with accepted clinical practices. Procalcitonin, CRP, and blood cultures were assessed both before and three days after the start of antibiotic treatment. The most frequently isolated pathogen was CoNS, found in 10 cases (25%). Enterobacter spp., Streptococcus epidermidis, and Candida albicans were each identified in two cases (5%). Other isolated organisms included methicillin-resistant coagulase-negative Staphylococcus (MRCNS), E. coli, K. pneumoniae, and P. aeruginosa (one case each, 2.5%).
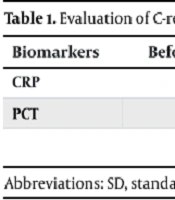
Elevated levels of both CRP and PCT were observed in 31 out of 40 infants (77.5%) prior to treatment. A statistically significant reduction was observed in both CRP and PCT levels three days after treatment initiation (P > 0.05 for both, t-test) (Table 1).
| Biomarkers | Before Treatment (Mean ± SD) | Before Treatment (Median) | After Treatment (Mean ± SD) | After Treatment (Median) | P-Value |
|---|---|---|---|---|---|
| CRP | 31.82 ± 37.3 | 17.8 | 10.80 ± 19.02 | 5 | > 0.05 |
| PCT | 10.77 ± 12.13 | 7.6 | 2.75 ± 7.09 | 0.1 | > 0.05 |
Abbreviations: SD, standard deviation; PCT, procalcitonin; CRP: C-reactive protein.
This table shows the comparison of serum CRP and PCT levels before and after treatment in neonates with LOS. Although a decrease was observed in the mean and median values of both biomarkers after treatment, the changes were not statistically significant (P > 0.05). This indicates that the observed reductions could be due to random variation and not necessarily a response to treatment.
5. Discussion
Sepsis that does not pass via the placenta is a significant concern in neonatal care. Gestational age has little effect on its concentration, although non-infectious conditions such as meconium aspiration syndrome, neonatal hypoxia, and intraventricular hemorrhage may cause it to increase (15, 16). After an infection starts, CRP usually begins to rise 4 - 6 hours later and peaks 24 - 48 hours later. With appropriate care, its levels drop quickly. According to a study by Benitez et al. in Spain, when CRP levels are higher than 5 mg/dL, there is a 10% chance of confirmed sepsis (17). Depending on the study, the specificity of CRP in identifying NS varies from 62% to 95%, whereas the sensitivity ranges from 75% to 93%. In our investigation, CRP showed a 77.5% sensitivity and an 87.5% specificity (17).
Procalcitonin is another acute-phase reactant whose secretion is primarily triggered by bacterial endotoxins. It has been shown that viral infections, autoimmune conditions, oncological diseases, and localized or limited infections do not significantly elevate PCT levels. Therefore, PCT is especially useful for distinguishing bacterial from non-bacterial infections (18). Canpolat et al. in Turkey reported that PCT levels, particularly in umbilical cord blood, had a high positive predictive value (PPV) for diagnosing early-onset NS (19). In a study by Yildiz et al. in Turkey, the sensitivity, specificity, PPV, and negative predictive value (NPV) for PCT (cut-off: 2 ng/mL) were 92.15%, 94.33%, 94%, and 92.5%, respectively. In comparison, for CRP (cut-off: 8 mg/dL), these values were 87.03%, 86.20%, 90%, and 74.6%, respectively (20). These results were approximately 15 - 20% higher than the findings in our study. Similarly, Koksal et al. in Turkey validated the diagnostic value of PCT and CRP in newborn sepsis. According to their investigation, the sensitivity and specificity for PCT (cut-off: 2 ng/mL) were 48% and 100%, while the sensitivity and specificity for CRP (cut-off: 1 mg/dL) were 48% and 87%, respectively. Procalcitonin had a 10 - 15% greater specificity than CRP, which is consistent with the results of our investigation, despite the claimed sensitivity being very low (21).
In a cross-sectional study by Fallahi et al. in Iran, conducted at Shohadaye Tajrish Hospital on 76 neonates with suspected sepsis, the sensitivity and specificity of PCT in the total cohort were 75% and 42.6%, respectively. In neonates younger than two days, sensitivity was 100% and specificity 22.5%; while in those older than two days, both sensitivity and specificity were 71.4%. The authors concluded that although PCT is useful for diagnosing NS, its specificity remains relatively low (22). Finally, in a study by Umran et al. in Iraq at Al-Zahra Hospital in Najaf, PCT levels were considerably higher in septic newborns than in healthy controls. Their findings suggest that PCT is more sensitive than CRP and may be employed as a standard biomarker for the early detection of NS, potentially reducing the unnecessary use of antibiotics (23).
5.1. Conclusions
Procalcitonin is a useful biomarker for the early detection of NS. Its rapid rise in response to bacterial infection underscores its utility in identifying EOS. One of PCT’s main advantages over other inflammatory markers like CRP is its specificity — its levels do not appreciably increase in non-infectious conditions such as meconium aspiration syndrome or after surgery. This feature enhances its ability to distinguish bacterial sepsis from other neonatal problems.