Introduction
Heart failure (HF), a progressive cardiac disease that accompanies with cardiac dysfunction, salt and water retention and peripheral circulatory disorders, affects nearly 5.7 million Americans of all ages and is responsible for more hospitalizations than all forms of cancer combined [1]. Cardiovascular disease, especially HF is prevalent in Iran and its increasing incidence is estimated almost 3500 people per hundred thousand [1, 2].
Despite recent advances in drug treatment for HF, many patients do not have the compliance of taking drug treatment sufficiently. Previously the only treatment which was offered to these patients could be heart transplantation or a cardiac assist [3].
In approximately 30% of patients with HF, the disease process not only depresses cardiac contractility but also affects the conduction pathways by causing a delay in the onset of right or left ventricular systole [4-6]. So biventricular pacing or CRT (cardiac resynchronization therapy) has been introduced as a promising therapeutic choice in patients with ventricular dyssynchrony; as indicated by prolonged electrocardiography QRS duration and impaired systolic function [7]. A number of investigations have proven that CRT could improve left ventricular systolic and diastolic function, improve quality of life, and decreases morbidity and mortality in HF patients [8-10]. Moreover, the results of our previous study showed that the CRT has a positive effect on LVEF (left ventricular ejection function) in HF patients [11]. These beneficial findings may be associated with a reduction in MR (mitral regurgitation) through improvements in atrioventricular coupling, intraventricular and interventricular synchronization, increased efficiency of left ventricular filling and ejection. However, the reports about acute and chronic reduction of the severity of MR in HF patients were to some degree dissimilar (for example reported significant mean MR reduction of more or less 20% in Acosta et al. to 45% in Linde et al. after biventricular pacing) [12-18].
MR is a common and significant clinical problem occurring in a fair proportion of patients with advanced HF and probably inducing additional adverse ventricular remodeling through volume overload that is associated with decreasing survival in patients with HF independent of the etiology [7]. Thus, MR may be an important factor influencing the final benefits in patients after CRT. Quantitative methods to measure the severity of MR usually leads to more accurate results. So, we aimed to investigate the effect of CRT on the treatment of MR quantitatively using the volumetric Doppler method in HF patients.
Materials and Methods
In this prospective before-after study, 22 symptomatic HF patients with NYHA (New York Heart Association) class III or above despite optimal pharmacological therapy (convenience sampling) were enrolled. Inclusion criteria were an ejection fraction ≤35%, and wide QRS complex (≥120 ms) in the form of bundle branch block or intraventricular conduction delay. The patients were referred to Heshmat educational hospital related to Guilan University of Medical Sciences- northern of Iran in a one year period (from June 2011 till June 2012) were enrolled to undergo implantation of a cardiac-resynchronization device. The informed written consents were taken from the patients and those who did not agree were excluded from the study. Also those patients who had EF >35% who got benefits from medical therapy, patients who had the history of ischemic cerebral or cardiac events during last 3 months and history of MV (mitral valve) disease such as MV prolapsed and chordal rupture were excluded.
Study protocol: Biventricular pacing was done through cardiac-resynchronization device along with three pacing leads: standard right atrial and right ventricular leads, and a specialized left ventricular lead. Right atrial and right ventricular leads were placed through subclavian vein and left ventricular lead was inserted by a transvenous approach through the coronary sinus into either the posterior or posterolateral cardiac vein.
Patients were evaluated both before and 2 months after the CRT procedure for NYHA class, QRS complex width (based on leads II, V1 and V6 in electrocardiography), left ventricular volumes, MV area and MR by two-dimensional Doppler-flow echocardiography (GE, Vivid 6 Milwaukee, Wisconsin, USA) through a multi-frequency (1.5-4 MHz) transducer in parasternal and apical views. MR was graded quantitatively by volumetric method and color Doppler imaging [14]. MR volume was obtained from subtraction of AS (aortic stroke) volume from MS (mitral stroke) volume. The MS volume and AS volume were calculated as the cross-sectional area of mitral annulus and aortic annulus multiplied by the pulsed-wave Doppler time-velocity integral at the annular level, respectively (AS and MS volume= 1.4×π× (diameter)2× (time-velocity integral)). Diameters of the mitral at the time of maximum valvular opening and aortic annuluses were measured from the echocardiographic apical 4- and 2-chamber views and the parasternal long-axis view, respectively. MR fraction (%) was calculated from MR volume divided by MS volume. The protocol of the study was approved by Research Ethical Committee of Guilan University of Medical Sciences.
Statistical analysis: Statistical analysis was performed by SPSS-16.0 (SPSS Inc., Chicago, IL, USA). All results represent averages of three measurements in different cardiac cycles. Results were expressed as mean±SD (standard deviation) unless otherwise specified. The data were tested for normal distribution and homogeneity of variance by the K-S test (Kolmogorov-Smirnov) and Levene test respectively. For the comparison of continuous variables before and after CRT, paired sample t-test was used. p-value of less than 0.05 was considered statistically significant.
Results
Overall, among 22 HF patients who enrolled in the survey (prospective before- after study), 16 (72%) were males and 6 (28%) were females, with the mean age of 60±13 years old. In the initial evaluation, all patients were in NYHA class III and none of them were in NYHA IV. The mean QRS complex width was 125±4 ms. Table 1 shows the initial demographic, hemodynamic and echocardiographic data of all patients. No patient was excluded because of unsuccessful implantation.
Two months after CRT insertion, mean QRS width decreased significantly (105±4 ms, p<0.0001), while 18 patients (81%) were in NYHA class I and 4 (19%) were in NYHA class II (no one maintained the same NYHA class and no one got worse grade).
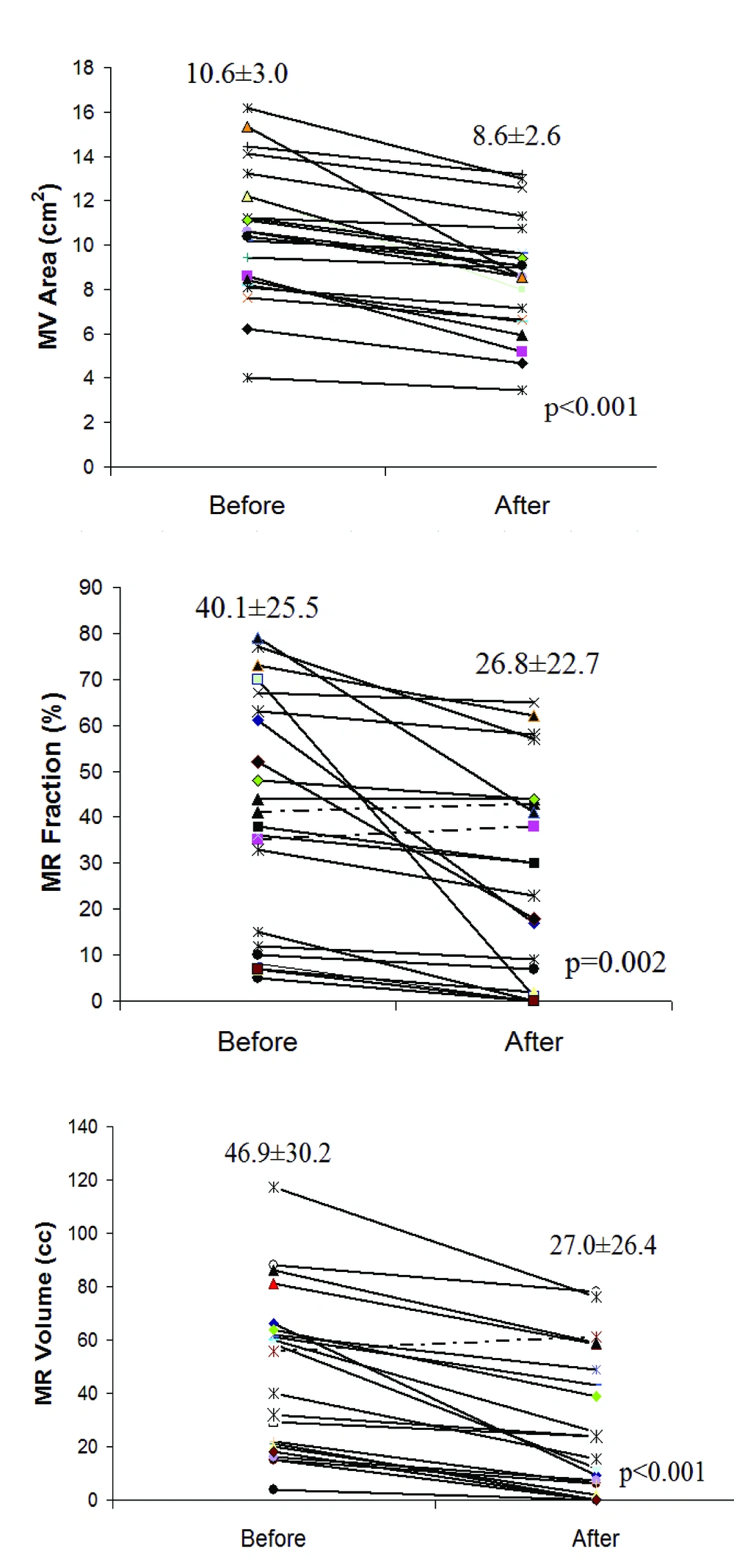
Both mean MR volume and MR fraction decreased significantly 2 months after biventricular pacing (p<0.001, p=0.002 respectively). Mean MV area as also measured initially and after CRT which showed a significant decrease after biventricular pacing (p<0.001), (Table 2).
Biventricular pacing significantly decreased QRS width, MR volume (in 21 of 22 patients and a small increase was observed in one patient after CRT), MR fraction (in 20 of 22 patients and a small increase was observed in 2 patients after CRT) and MV area (in all patients). Totally in the initial evaluation, 9 patients (41%) had mild MR (MR volume <30%), while 13 patients (59%) had moderate and severe MR (MR volume >30%). After 2 months from CRT, 14 patients (64%) had mild MR and only 8 patients (36%) had moderate and severe MR. Individual changes in MR area, MR fraction and MR volume between baseline and post-CRT in all study patients presented in figure 1.
| Variables | Mean±SD |
|---|---|
| Age (yr) | 60±13 |
| QRS width (ms) | 125±4 |
| LVEF (%) | 20.4±5.8 |
| MR volume (mL) | 46.9±30.2 |
| MR fraction (%) | 40.1±25.5 |
| MV area (cm2) | 10.6±3.0 |
a MR= mitral regurgitation, MV=mitral valve, LVEF=left ventricular ejection fraction
| Variables | Before CRT | After CRT | p-Value |
|---|---|---|---|
| MR volume (mL) | 46.9±30.2 | 27.0±26.4 | <0.001 |
| MR fraction (%) | 40.1±25.5 | 26.8±22.7 | <0.002 |
| MV area (cm2) | 10.6±3.0 | 8.6±2.6 | <0.001 |
| QRS width (ms) | 125±4 | 105±4 | <0.001 |
MR= mitral regurgitation, MV=mitral valve
Discussion
In this study, we evaluated effects of CRT on the severity of MR quantitatively in HF patients. The findings support the benefits of CRT on HF patients' morbidity as shown with the significant decrease in NYHA class after CRT and left ventricular synchrony as shown with narrowing of QRS complex after CRT. Our data suggest the efficacy of CRT on the magnitude of MR as indicated with the significant decrease in MR volume, MR fraction and MV area after biventricular pacing.
Today majority of data support the hypothesis that biventricular pacing or CRT can improve cardiac function and efficiency in HF patients with discoordinate contraction due to abnormal conduction. Several recent placebo-controlled trials suggest that CRT benefits can be substantial on HF patients' NYHA class, quality of life score, and left ventricular function following CRT [3, 4, 19-22]. However, the reports about acute and chronic reduction of the severity of MR in HF patients were to some degree dissimilar.
Abraham et al. in a survey on the effect of CRT on HF patients reported that CRT reduced the degree of ventricular dyssynchrony and this effect was accompanied by a decrease in the magnitude of MR [4]. In an investigation by Linde et al. on long-term benefits of biventricular pacing in HF patients (MUSTIC study), the MR decreased by 45% in HF patients with sinus rhythms. They also showed that biventricular pacing had induced a significant decrease in QRS width of 8% to 14% in the same patients [3]. Acosta et al. represented a significant mean absolute MR reduction of 21% after biventricular pacing in HF patients [7]. The present study demonstrated 42% improvement in mean MR volume was shown after CRT in the present survey which is comparable to Linde's survey. In a study by Etienne et al., the MR jet area significantly decreased from 11.5±6 to 6.6±4 cm2. This is to some extent different from 2 cm2 decrease in MV area in this study (10.6 ± 3 cm2 vs. 8.6 ±2.6 cm2). Etienne et al. at baseline, 17 patients (74%) had a moderate or severe MR, but only 7 patients (30%) at 6 months [23]. In our study at baseline, 13 patients (59%) had moderate or severe MR and after 2 months from CRT only 5 patients (23%) had moderate or severe MR. In the study by some differences in the various surveys may be due to different strategy of sampling, evaluating method, time duration following CRT and different populations. Quantitative methods such as volumetric Doppler method to measure the severity of MR in HF patients usually leads to more accurate results. So, in this study we measured MR severity quantitatively using this method to investigate the effect of CRT on the treatment of HF patients.
Effective MV closure depends on the interaction of several anatomical and dynamic factors. Anatomically, the status MV annulus, leaflets, chordae tendinae, papillary muscles, left atrium, together with the size and function of left ventricle play important roles in MV function. When the heart is dilated, as in HF patients, functional MR could be due to increase in the distance between the papillary muscles and mitral annulus dilatation. These geometrical changes could lead to increased tethering of the leaflets, decreasing their mobility and MV closing forces.
Since MR is a common condition in HF patients, it is crucial to say that biventricular pacing could be a novel therapy for the treatment of MR in these patients. Although the mechanisms of this effect are not well understood, one proposed mechanism is resynchronization or better coordination of the contractility of the papillary muscle and the adjacent myocardial tissues which can lead to more effective cooperation of the MV leaflets [7, 14, 24].
There are some limitations in the present survey. As data of our study are limited to two months follow-up, the long-term effects of biventricular pacing are unclear and long-term survival is unknown. The low sample size is another limitation of the present study; though statistical sample calculation showed that in this study the sample size is enough and adequately powered to show differences between the measurements before and after CRT.
Our investigation supports the effectiveness of CRT on the treatment of MR in patients with HF. As MR is associated with morbidity and mortality in these patients and the standard surgical therapy may not be practical for a majority of them, this novel treatment may improve their disease condition significantly.