Introduction
In paraxial optics, the focus is essentially stigmatic. Peripheral or non-paraxial rays do not necessarily focus stigmatically. Deviations from stigmatic imaging are called aberrations.
Unlike the spherical lens surface, the astigmatic lens surface does not have the same curvature and refracting power in all meridians. The curvature of an astigmatic lens varies from a minimum value to a maximum value, with the extreme values located in meridians 90° apart. Thus, the refracting power varies from one meridian to the next, and an astigmatic surface does not have a single point of focus [1]. Astigmatism may cause blurred vision, glare sensation, monocular diplopia, asthenopia and visual aberrations [2]. Correction of astigmatism is one of the main purposes of modern cataract surgery; this has resulted in a shift toward small incision surgery using foldable intraocular lenses (IOLs) [3].
Several methods have been employed for this purpose including changing the size and site of the incision [4], using corneal or limbal relaxing incisions [5], applying opposite clear corneal incision (OCCI) on the steep axis [6], implantation of toric IOLs [7, 8] and laser in situ keratomileusis (LASIK) [9]. The aim of all the above-mentioned measures is to achieve acceptable uncorrected visual acuity (UCVA) and improve patient satisfaction. Early visual rehabitation and targeting of emmetropia is the main objectives of modern cataract surgery. Lever and Dahan were the first to apply a pair of OCCI on the steep axis to correct pre-existing astigmatism during cataract surgery [6]. This method does not require additional skill or instruments. IN our study we evaluated the efficacy of adding an OCCI on the steep axis of the cornea during phacoemulsification in order to reduce pre-existing corneal astigmatism. Applying opposite clear corneal incision (OCCI) on the steep axis can cause flattening and decrease corneal astigmatism which is effective and have low cost.
Materials and Methods
This randomized clinical trial was conducted on 40 patients in tow group with senile cataracts with age greater than 21 and corneal astigmatism greater than 1.5 dioptre (D). Exclusion criteria were any previous ocular surgery, corneal lesions, scars, degenerations, dystrophies, glaucoma, and irregular astigmatism.
Preoperative evaluation included visual acuity with snelen chart, refraction (Topcon auto-refractometry RM A7000), bio microscopy (Topcon-SL-3C) detailed slit lamp bio microscopy, applanation tonometry (HAAG-AT-900), dilated fundoscopy (Topcon-PS-12), keratometry (Tomey auto-ref-keratometry RC-1000) and topography (Zeiss-Humphrey corneal topography model 995). The procedure was explained to the patients preoperatively and informed consent obtained. The steep corneal axis was marked on the conjunctiva with an astigmatic marker while the patient sat upright to avoid the torsional effects of the oblique muscles.
The type of anaesthesia was either general or local retro bulbar. In Opposite clear corneal incision (OCCI) group self-sealing 3-step corneal incision was performed with a 3.2 mm keratome 1 mm anterior to the limbus on the steep axis. After viscoelastic injection, a similar incision was made opposite the first incision on the steep axis to enhance flattening of the cornea for correction of the pre-existing astigmatism. One incision was used for phacoemulsification, and the other was left unused, and in second group phacoemulsification incision was made in steep meridian.
A standard conventional phacoemulsification was performed followed by bimanual irrigation/aspiration then foldable posterior chamber intraocular lens implantation inside the capsular bag. At the end of the operation only the irrigation/aspiration incisions were hydrated. All the patients received routine postoperative topical steroids and antibiotics eye drops for 5 th weeks. They were examined at the first and 4th and 12 week postoperatively. During the follow up period, all the patients were assessed for best corrected visual acuity, refraction, keratometry, and topography. Statistical analysis was performed with preoperative and postoperative topographic keratometric reading using simple subtraction with the mean and standard deviation and compare data with paired t-test in SPSS-16 program. p≤0.05 was statistically significant.
Results
The two study groups did not differ significantly in terms of age and sex (data not presented).
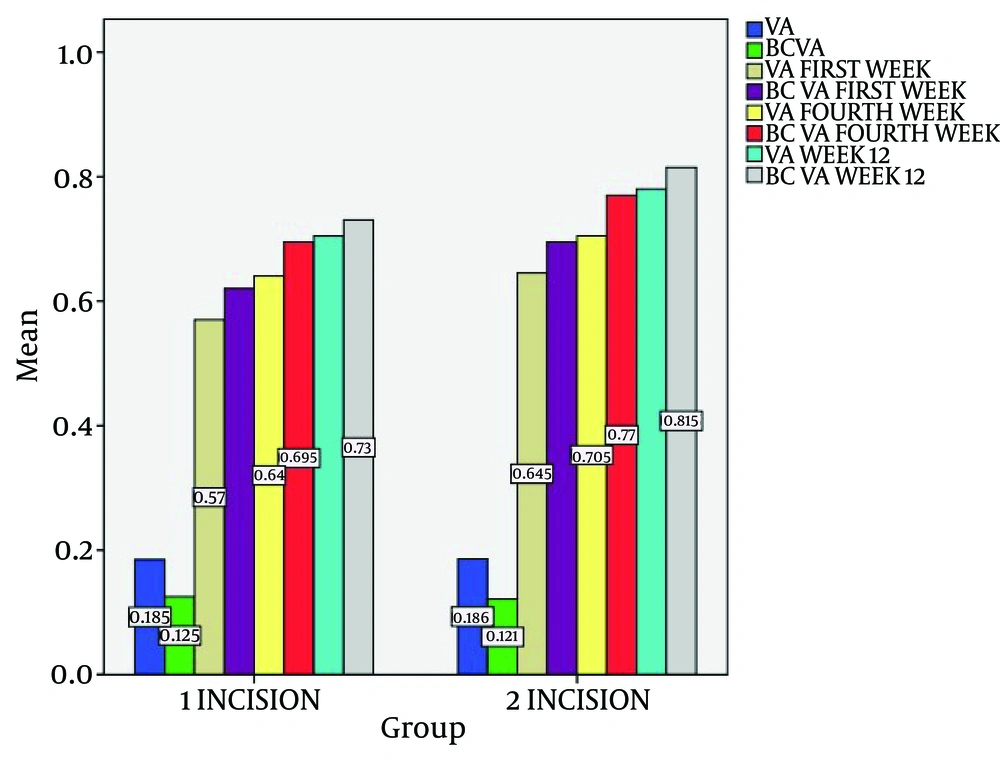
Figure 1 summarizes pre- and postoperative visual acuity in study groups which had not significantly difference. Mean corrected visual acuity at 1 week was significantly better in occi group (p=0.01). Mean UN corrected visual acuity at 4 week was significantly better in occi group (p=0.01). Mean UN corrected visual acuity at 12 week was significantly better in occi group (p=0.007).
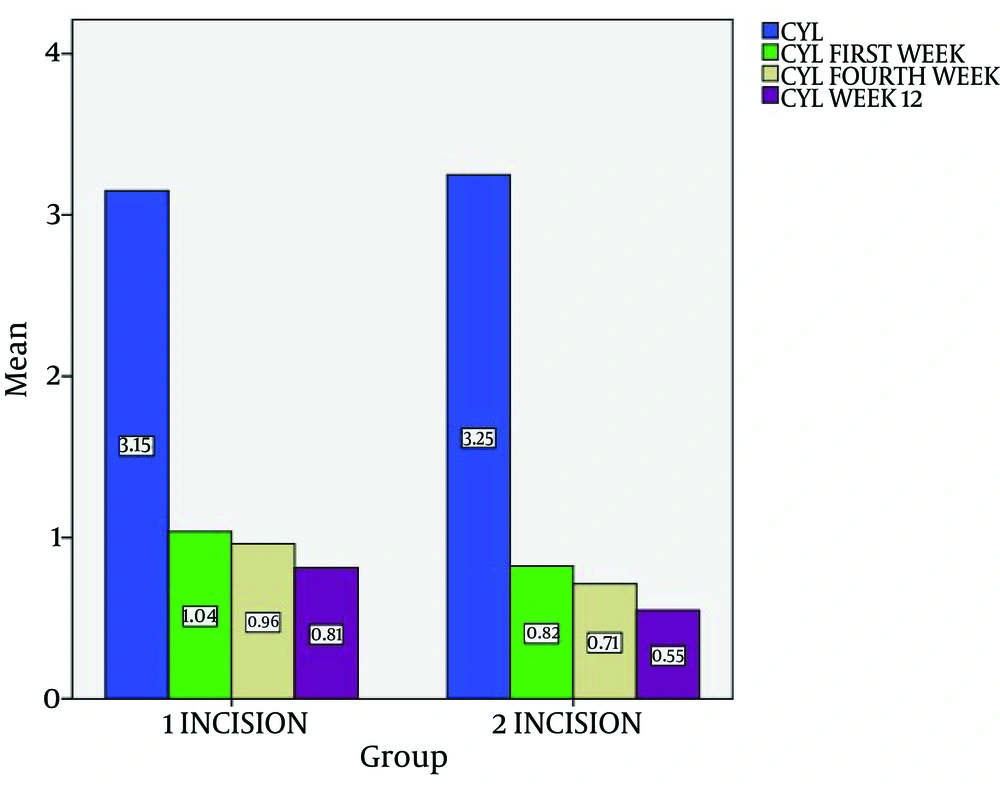
Figure 2 summarizes pre-operative astigmatism in study groups which had not significantly difference. Post-operative residual astigmatism in steep incision group was significantly greater than occi group at 1 week (p=0.005). Post-operative astigmatism in steep incision group was significantly greater than occi group at 4 week (p=0.001) Post-operative astigmatism in steep incision group was significantly greater than occi group at 12 week (p=0.001).
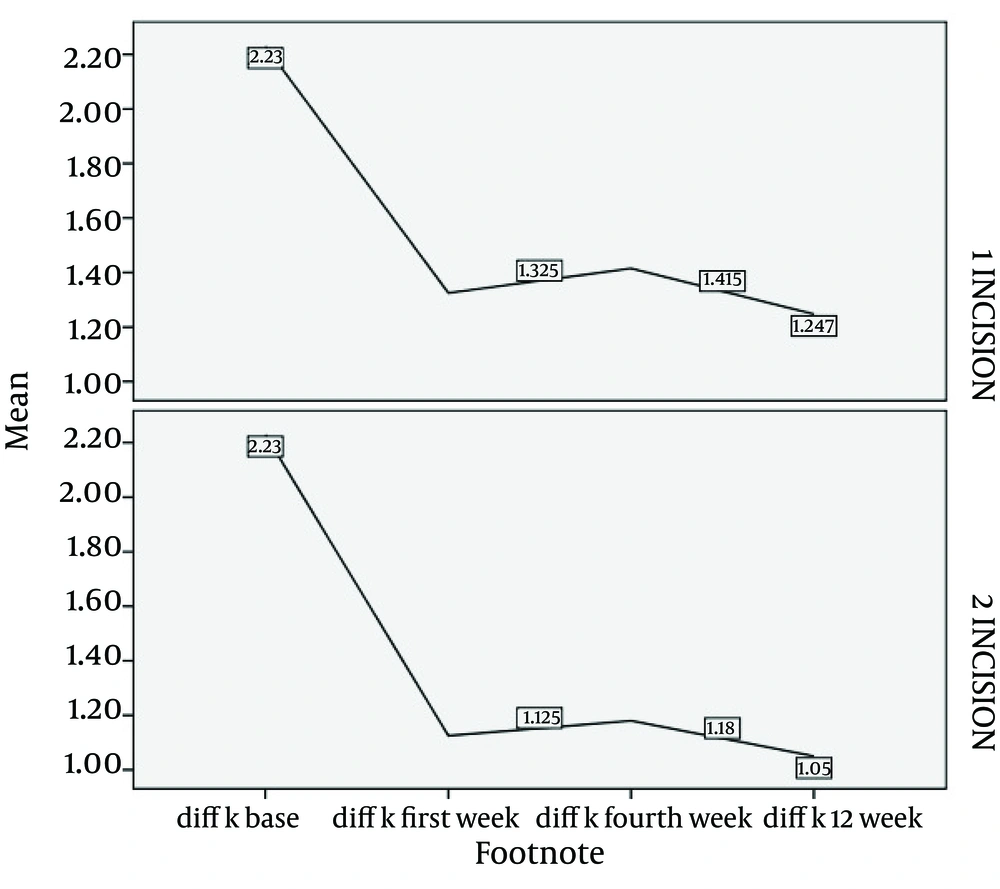
Figure 3 summarizes pre-operative keratometry in study groups which had not significantly difference. Post-operative keratometry in steep incision group was significantly greater than occi group at 1 week (p=0.001). Post-operative keratometry in steep incision group was significantly greater than occi group at 4 week (p=0.002). Post-operative keratometry in steep incision group was significantly greater than occi group at 12 week (p=0.01).
Discussion
In our study mean corrected astigmatism was greater in opposite clear corneal incision group than steep meridian incision phacoemulsification group. No significant change occurred in amount of astigmatism in two groups.
Astigmatism can correct with glass, contact lens or surgery in regular pattern and with contact lens in irregular pattern. Most cause of astigmatism is cornea and with the rule astigmatism [1] astigmatism correction done with flattening in steep meridian [10].
Post-operative residual astigmatism in steep incision group was significantly greater than occi group. So corrected astigmatism in occi group was greater than steep incision group.
Patients undergoing cataract surgery expect clear vision and less dependence on spectacles. To attain this goal, one important consideration is reduction of astigmatism. Modern cataract surgery using small incisions and foldable IOLs has led to achieving emmetropia in a great number of patients. Modifications in surgical technique and incisions may further improve refractive outcomes by reduction of astigmatism. Different methods have been used to correct pre-existing astigmatism during cataract surgery. Making the incision on the steep corneal axis is the simplest method but may be difficult or impossible with certain axes. The amount of correction using this method varies but is usually reported to be less than 1 D. Astigmatic keratotomy, is another alternative which entails drawbacks such as glare sensation, diplopia and fluctuation of refractive error due to proximity of the incisions to the center cornea. In addition, it requires preoperative pachymetry and use of a diamond knife. Corneal relaxing incisions are another method for correction of pre-existing corneal astigmatism; advantages include being technically easy, producing fewer symptoms, earlier wound stabilization due to the location of the incision and inducing no change in spherical equivalent when 2 incisions are made due to coupling effect. However, this method also suffers from limitations such as requiring pachymetry and use of a diamond knife, in addition to controversies regarding application of the nomogram. Implantation of toric IOLs is another option, however these lenses are expensive and their implantation requires additional skills; moreover, postoperative rotation remains a major drawback. Excimer laser ablation may also be used to correct residual or induced astigmatism after cataract surgery. Major concerns include the cost of the procedure, limited number of canters equipped with excimer machines, adverse effects specific to excimer laser surgery such as loss of BCVA, flap related complications, night vision disturbances and regression.
Lever and Dahan reported 33 patients that 3.5 mm opposite clear cornea incisions straddling the steep axis decreased pre-existing astigmatism by a mean value of 2 D [6]. Corresponding figures using this method have been reported to be 1.5 D by Khokhar et al. [11].
In contrast to the previously mentioned methods, paired OCCI on the steep axis is technically easy without need for additional equipment. The same 3.2 mm knife used by most surgeons for routine phacoemulsification cataract surgery is used for making both incisions and therefore no additional cost is entailed. This method is effective for correction of mild to moderate corneal astigmatism, but in eyes with higher degrees of astigmatism it is recommended to use an alternative method or a combination of two or more methods.
Some authors recommend a larger clear cornea incision on the steep axis to increase the effect of the procedure while temporary sutures are placed for closing the wound. Disadvantages of this method include the increased risk of endophthalmitis due to the penetrating nature of the incisions as compared to non-penetrating methods. For control of leakage in this method one can use nylon sutures for wound closure.
Qmar and Mullaney reported 15 patients that 3.5 mm opposite clear cornea incisions straddling the steep axis decreased pre-existing astigmatism by a mean value of 2 D [12] and 0.5 D by Tadros et al. [13].
Zemaitiene et al. reported 28 patients that 4 mm opposite clear cornea incisions straddling the steep axis and 9 patients that 3 mm opposite clear cornea incisions straddling the steep axis decreased pre-existing astigmatism [14]. Bazzazi et al. reported that 3.5 mm opposite clear cornea incisions straddling the steep axis decreased pre-existing astigmatism [15]. Zare et al. reported that limbal relaxing decreased pre-existing astigmatism [16].
The two study groups did not differ significantly in terms of age and sex. Pre- and postoperative visual acuity in study groups had not significantly difference. Mean corrected visual acuity at 1 week was significantly better in occi group. Mean UN corrected visual acuity at 4 week was significantly better in occi group. Mean UN corrected visual acuity at 12 week was significantly better in occi group.
Pre-operative astigmatism in study groups had not significantly difference. Post-operative residual astigmatism in steep incision group was significantly greater than occi group at 1 week. Post-operative astigmatism in steep incision group was significantly greater than occi group at 4 week. Post-operative astigmatism in steep incision group was significantly greater than occi group at 12 week. Pre-operative keratometry in study groups had not significantly difference. Post-operative keratometry in steep incision group was significantly greater than occi group at 1 week. Post-operative keratometry in steep incision group was significantly greater than occi group at 4 week. Post-operative keratometry in steep incision group was significantly greater than occi group at 12 week.
In conclusion, paired opposite clear corneal incisions on the steep axis are useful for correcting mild to moderate pre-existing astigmatism during cataract surgery. Employing this technique during routine phacoemulsification using a 3.2 mm incision does not require additional instruments and therefore can be performed without altering the surgical setting.