Introduction
Tracheal diverticulum is a rare entity, usually discovered incidentally as an out pouching at the right side on radiography, or computed tomography (CT) [1, 2]. Two types are present: congenital and acquired [2, 3]. A tracheal diverticulum may act as a source of secretions that may spill over into the tracheobronchial tree, causing cough, dyspnea, stridor, and chronic chest infection [2, 3]. We present the case of a male patient with a tracheal diverticulum detected during a work-up for bronchiectasis. His thoracic CT scan showed sac formation on the dorsal wall of the trachea.
Case Report
The patient is a 59-year-old baker who presented with complaints of cough, shortness of breath, and sputum production. He had these symptoms in milder form since he was 20 years old and had received treatment for them at that time. During the past 2 months the severity of symptoms had increased. One month prior to admission, he developed bilateral lower extremity swelling and was hospitalized in his town for cor pulmonale. He had pleural effusion too. There was no Jugular venous distension or lymphadenopathy in the head and neck. Lung exam showed diffuse coarse crackles on the right side. Cardiac exam was normal. Abdominal exam was normal with no organomegaly. The patient had no clubbing, cyanosis or edema.
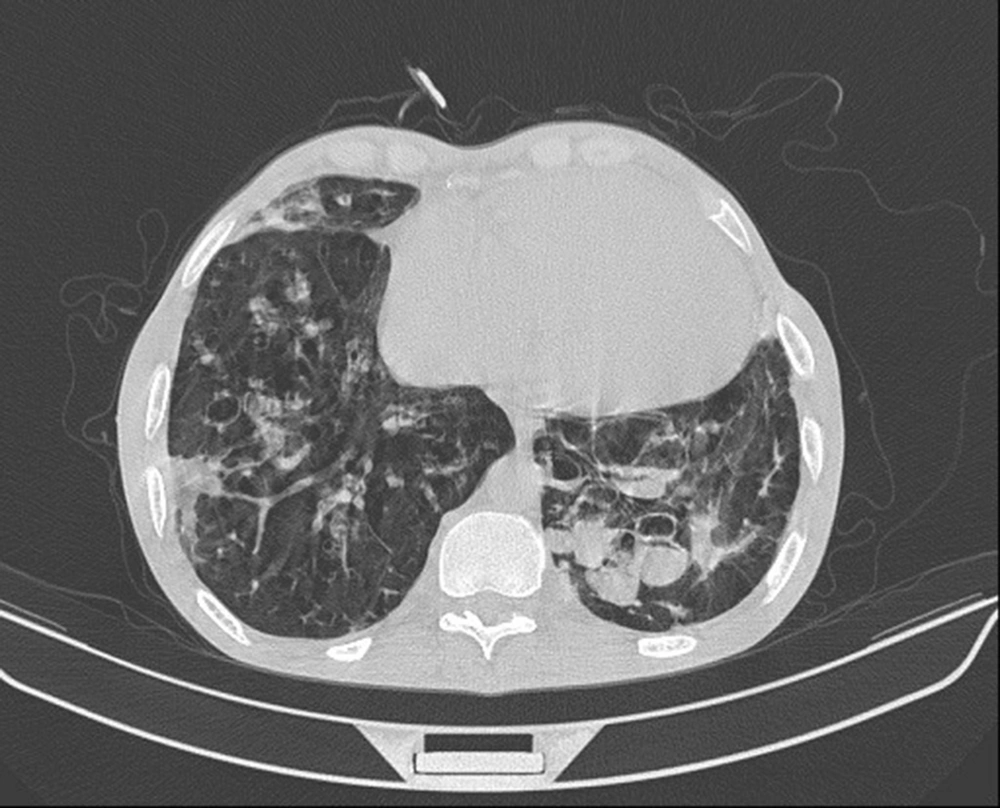
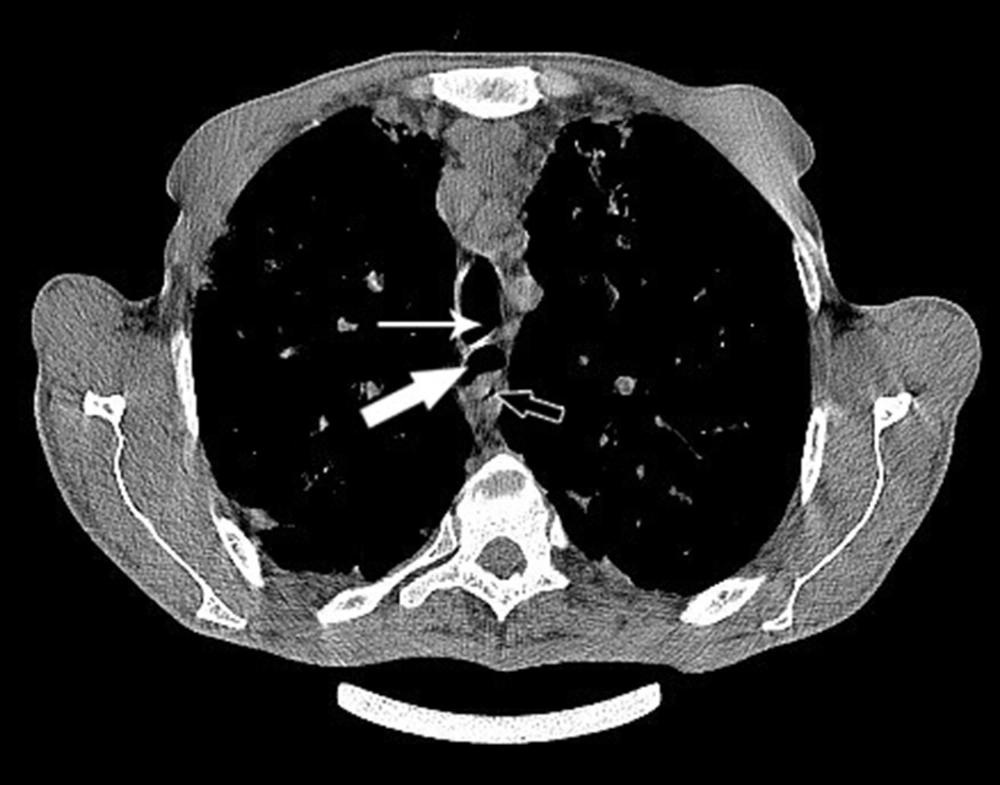
Echocardiogram showed dilated right ventricle and right atrium, HRCT of lungs showed diffuse bronchiectasis with mucus impaction more prominent in left lower lobe, mosaic attenuation in lung fields, and sub pleural consolidation in right lower lobe (Fig. 1). An air filled focus between trachea and esophagus that extended inferiorly with a narrow connection to tracheal lumen was also reported which was compatible with tracheal diverticulum (Fig. 2).
The patient was treated with medications steroid, theophylline, ciprofloxacin and ceftriaxone and supportive care including physiotherapy. He was discharged in good condition. Patient consent was obtained for case presentation.
Discussion
Para tracheal diverticula may be detected incidentally on radiography of patients done for other reasons or may be symptomatic [1]. Prevalence of tracheal diverticulum by autopsy studies has been reported to be 1%. It was first described by Rokitansky in 1838. Goo et al. reported 64 cases [4].
The differential diagnosis of an air filled par tracheal lesion includes a laryngocele, a pharyngocele, a Zenker’s diverticulum, tracheal diverticulum, apical hernia of the lungs, apical paraseptal bullae, and bronchogenic cysts. Radiological barium swallow study, endoscopic techniques, and computed tomography can be used to characterize the lesion. Computed tomography examination, including thin sections or reconstructed images, is the proper imaging method for the study of tracheal diverticulum. It can demonstrate the connection between the diverticulum and the tracheal lumen and the possible damage of lung's parenchyma as the result of chronic illness. It is divided into 2 groups congenital and acquired. Congenital cases are usually smaller and located 4-5 cm below the vocal cords or a few centimeters above the carina. The right side of the trachea is more commonly involved. They are more prevalent among men compared to women [4]. Acquired diverticula can be seen at any level. They can be related to increased pressure in the tracheal lumen [5].
There have been only a few cases of tracheal diverticulum associated with bronchiectasis reported in the literature. There was a case report of a 38-year-old male with chronic cough and sputum production. Helical chest CT showed tracheomegaly and many diverticular outpouchings and cystic bronchiectasis of lower lobes [5]. Tracheal diverticulum can have side effects such as recurrent respiratory infections and difficulty with intubation or chronic cough [6]. There has been report of dysphasia and friction sensation associated with tracheal diverticulum. The diverticulum was removed surgically and at 2 year follow up, the patient had no symptoms [7].
There has also been report of cyclic symptoms such as in a 62-year-old lady with tracheal diverticulum who at times developed a neck mass that was painful along with cough, dysphonic, dysphasia/odynophagia and sometimes feeling out of breath [4].