1. Introduction
Echinococcosis or hydatid disease is mainly caused by the larval stage of the tapeworm Echinococcus granulosus and less frequently by Echinococcus multilocularis. Echinococcosis is an important systemic zoonotic disease over the world [1, 2]. Hydatidosis is endemic in many parts of the world including Mediterranean region, Africa, South America, Middle East, Australia and New Zealand [3, 4]. However, this condition may occur even in non-endemic areas occasionally, because of rapid people transferring from endemic regions. Hydatosis is a medical and public health problem all over the world [3]. People may infected by ova, then the embryos are released in blood circulation [2] and reach other organs, more commonly to liver (60 - 70%) and then lung (10 - 15%); where involvement of the other organs is seldom [5]. Cerebral hydatid cyst (HC) is very rare, roughly 2% of all hydatosis; which is seen after secondary involvement mostly in cerebral parenchyma. Metastasis of the HCs in the brain may is a result of the liver or lung function failure. The rout of ova penetration to the brain is hematogenous [2, 3, 5, 6]. It can occur within any region of the brain but particularly in middle cerebral artery territory and most often in parietal and tempero-occipital lobes [2, 5]. In comparison to the adults, the brain HC is more common in children [5-7].
2. Case Presentation
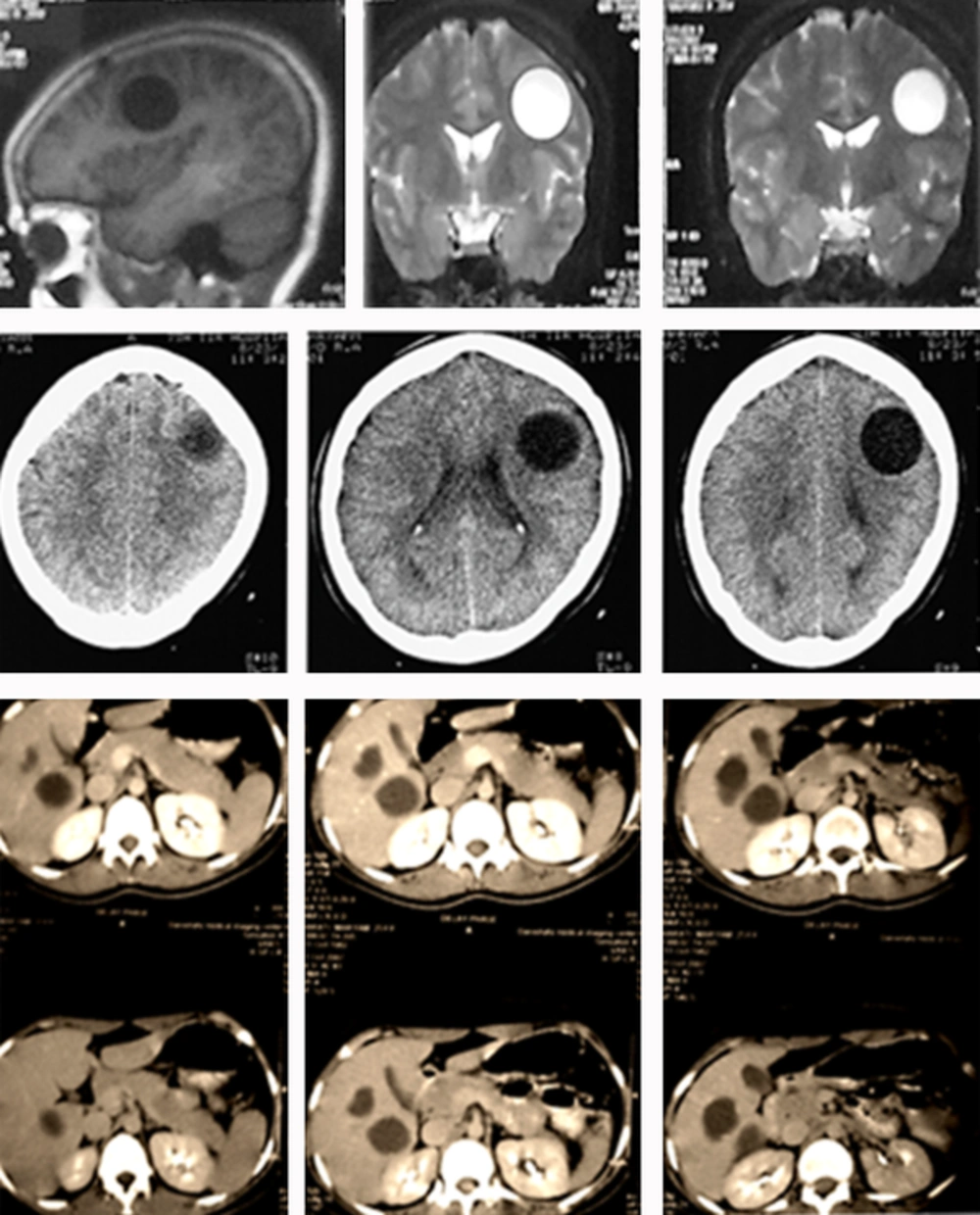
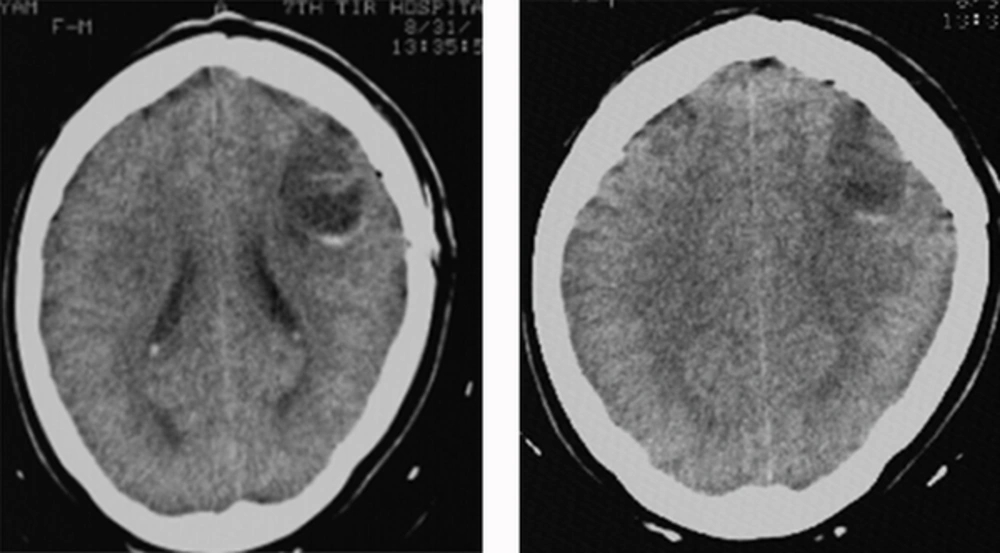
A 25-year-old woman, with one episode of seizure 2 hours before examination, was admitted by the emergency ward of Shohadaye Hafte-Tir Hospital, related to Shahid Beheshti University of Medical Sciences, Tehran, Iran. During the general primary examination, she experienced another generalized tonic colonic seizure, which was confirmed by a neurologist. She had no other symptoms. On the neurological examination she had paresthesia in the right upper extremity, with no pupil edema. The brain computed tomography (CT) revealed a 4.7 × 3.2 cm round hypodense and non-enhancing space occupied lesion without pericystic edema or ring enhancement at the left hemisphere in the parietal lobe. Furthermore, magnetic resonance imaging (MRI) demonstrated a hemispheric round lesion with no edema and invasion, at the left hemisphere. Figure 1 (top) illustrates a hypo intense in the T1-weighted and a hyper intense in the T2-weighted images without any mural nodule. Furthermore, Figure 1 (middle), axial brain CT scan, shows a hypodense rounded non enhancing fluid space occupied lesion without pericystic edema or ring enhancement. Additionally, abdominal CT scan with contrast revealed certain cystic lesions in the right lobe of the liver, Figure 1 (bottom). Moreover, in the clinical laboratory exams, the IgG ELISA test was positive. Further, the histopathlogical examinations confirmed the HC. The patient underwent craniotomy and the cyst was resected completely without rupture. After the surgery, no cyst was seen any more in the brain CT (Figure 2). Thereafter, drug treatment was prescribed, albendazole (for 6 months and phenytoin for 8 months). The patient’s postoperative follow up showed normal neurological examinations, and she had good progressive recovery course.
(Top row) pre-operational MRI sagittal T1 and coronal T2 weighted image show a round hypointense T1, hyperintense T2 area in the parietal lobe; (middle row) axial CT scan shows a hypodense rounded non enhancing fluid space occupied lesion without pericystic edema or ring enhancement; (Bottom row) abdominal CT scan with contrast that shows cystic lesions in the right lobe of liver.
3. Discussion
Echinococcosis incidence has a low rate in the developed countries [4]. However, it is usually seen in endemic area of sheep raising. Moreover Echinococcus granulosus is responsible for the unilocular form or HCs, while echinococcosis alveolaris is causative for the multilocular form [5]. Human is the intermediate host for Echinococcus granulosus developing the cysts in the liver, lungs, heart, and brain. Cerebral hydatidosis is a very rare disease and it occurs roughly in 2% of all echinococcosis cases [3-6]. It includes 1.6 - 5.2% of all intracerebral space-occupying lesions [4]. Brain cysts are commonly seen in children, especially males and young adults. Studies show that 50 - 93% of the brain cysts are found in children younger than 17 years [2, 3, 7]. Additionally, incidence of the brain cysts in the children is eight times more than adults [4]. Echinococcosis brain cysts are usually single, medium and primary. The multiple cysts are very rare [3, 5]. The cysts grow slowly and they generally are asymptomatic until they reach a medium size. The most common symptoms are headache and vomiting [5]. Respecting the cyst site the other symptoms are hemiparesis, seizures, visual field defect, cranial nerve defect and ataxia; however, papilledema is usually a sign [5, 6].
Clinical feature of the brain HC is a little bit different in children, comparing with adults; it is more acute in adults. Papilledema is seen more frequently in younger ages. However, in the older patients the focal findings are predominant. These are hemiparesis, hemianopia, speech disorders, and sometimes epileptic seizures [2-7]. Most of the cysts are located in the supratentorial region and rarely in posterior fossa, ventricles postrolandic parts, subarachnoid space of the cerebellopontine angle, aqueduct of Sylvius, ventricular system, pons and intracranial epidural space [5]. Obviously, the HCs in the brain grow faster than those in the other organs by a ratio of 3:1. This shows that brain tissue, such as the lung tissue, expedites growing of the cyst [2, 5]. The cerebral cysts can grow to a mass, with a diameter of 1 cm, during 5 - 16 months. There are different reports respecting the growth-rate of the hydatid cysts. Abbassioun and Amir-Jamshidi [5] and Nemati et al. [7] reported a growth-rate of 1 cm per year in adults, where in the children is 4.5 cm per year. Furthermore, Mallik et al. reported the growth-rate of 10 cm per year in 15 years old boy [6].
Multiple cerebral HCs are very rare which are commonly seen after rupture, e.g. surgical, spontaneous, or traumatic; of a solitary primary cyst or rupture of a cyst in another site and embolization to the brain. The rate of the surgical rupture is about 25% [5, 8]. Aleksic-Shihabi and Vidolinb believed that the primary HCs could cause a defect between the left and right side of the heart [8]. The primary cysts are produced because of larva penetration in the brain without other visceral involvement [3]. In contrast, the solitary cerebral HC is the most common and cause of focal neurological deficits as well as increasing intracranial pressure [7]. We assume that at the time of diagnosis of the multiple cerebral cysts, with a faster growth-rate, the other organs’ cysts are too small to be distinguished. Occasionally, one will face with a new cyst in another organ few years after a cerebral cyst operation [3]. Therefore, prescription of the drugs after a cerebral surgery is recommended. In the other organs the activity of the immune system restricts growth-rate of the HCs; except in the CNS, which has a limited access to the immune system [6]. CT and MRI are very helpful in diagnosis of HC before surgery. Moreover, the serological tests are useful; however, sometimes they are false negative because of an insufficient immune response. Roughly 10 - 20% of the patients with HCs and 40% of the patients with pulmonary cysts, have false negative serologic tests [4, 8]. In diagnostic procedures CT shows the cerebral HCs with an accuracy of more than 90% [5]. Furthermore, MRI and CT show oval or cystic mass with intensity or absorption value similar to the CSF and without pericystic edema which sometimes cause compression on ventricular system and hydrocephalus. In contrast, HC mass is without pericystic edema which is typical for abscesses and cystic tumors also a hypointense rim in T2-weighted MRI is specific for brain HC [4, 5, 7]. It seems that MRI is superior to CT in determination of rim enhancement, pericystic edema and detection the degree of mass effect [2]. Although CT and MRI may be pathognomonic, but differentiation between HCs and other cerebral lesions, such as cystic brain tumors, abscesses, arachnoid cysts; is very important. Hence, absence of the pericystic edema and rim enhancement in the CT and MRI are valuable parameters in diagnosis [2, 7]. Also clinical findings, e.g. lesser age, chronic increased intracranial pressure, recent neurological defects, and epilepsy, tend to diagnosis of a benign disease [5]. The HCs are metabolically active, thus these patients are potentially appropriate for proton MRS (Magnetic Resonance Spectroscopy) [2-5]. However, the definitive diagnosis of HCs is based on the pathological examinations after surgery [2]. Surgery is the essential treatment for the cysts; however, drugs such as albendazole and/or mebendazole are used to prevent recurrence or dissemination [5]. We have to mention that in the present case, lactate, alanine, acetate, a medium resonance of pyruvate were observed.
In the present case (patient), the first manifestation was sudden seizure which was repeated after 2 hours, without any another symptom. In our opinion this type of presentation is rare in cerebral HCs. In this patient liver was also involved by several cystic lesions. Commonly drug treatment with antihelment, e.g. Albendazole, especially preoperatively, is beneficial for patients with medium (> 5 cm) or multiple cysts [2]. Moreover, we suggest a follow up for the operated patients in order to recognize the recurrence and/or complications. We also recommend postoperative medical therapy for these types of the patients. In our opinion in the endemic areas, hydatidosis should be considered using CT and/or MRI for the patients with a brain cystic mass. We also believe that in the nonendemic areas this should be noticed, because of abundant travelling and migration of the patients which could change the disease occurrence worldwide [2].