1. Background
Cytomegalovirus (CMV) is a member of the herpesviradae family which also includes Epstein-Barr virus, herpes simplex virus, varicella-zoster virus, and herpes virus 6, 7, and 8 [1]. The virus is transmitted through close personal contact with body fluids, including blood, urine and saliva, also cytomegalovirus infection can occur in immunocompetent individuals, but it most frequently occurs in immunocompromised patients such as recipients of organ transplants, patients undergoing hemodialysis, patients receiving immunosuppressive drugs, and patients with acquired immune deficiency syndrome [2]. Cytomegalovirus infection is ubiquitous in developed nations, with laboratory evidence of prior infection in 40% - 70% of the general adult population [3, 4]. Inflammatory bowel disease (IBD) represents a group of idiopathic chronic inflammatory intestinal conditions. The two main disease categories the covers are Crohn’s disease (CD) and ulcerative colitis (UC) with both overlapping and distinct clinical and pathological features. In recent years, cases of IBD associated with cytomegalovirus infection have occasionally been reported [5, 6]. In these patients, cytomegalovirus has been recognized in colonoscopy biopsy specimens obtained during evaluation and management of inflammatory bowel disease or diagnosed after pathologic examination of colon. Some reports have also assumed a triggering role of CMV infection in the onset or the worsening of the IBD or even in the development of malignancy in the colon [7, 8]. However, prospective studies examining prevalence of CMV genome in patients with IBD in comparison with a control population are limited. CMV infection in IBD patients often makes clinical diagnosis and treatment complex. de Saussure et al. treated 3 CMV-positive IBD cases with antiviral therapy, and only 1 patient got remission [9]. Kandiel and Lashner used antiviral drugs for the treatment of CMV positive colitis, and achieved a remission rate of 67% - 100% [10].
2. Objectives
Give the importance of inflammatory bowel disease as the unknown etiology and detection of an infectious agent in these patients might have important implications in treatment and prevention, the present study to investigate the prevalence of CMV in patients with ulcerative colitis in comparison with healthy subjects by using PCR technique conducted.
3. Patients and Methods
3.1. Patients
In this analytical case-control study, informed consent was received from all patients admitted to the Endoscopy clinic of Toos and Firoozgar hospital in Tehran, Iran, between January 2013 and May 2013. In this study five patients with ulcerative colitis and thirty patients without malignancy as controls were selected. Sampling was performed by endoscopic biopsy operation. All collected tissues were kept frozen under -20ºC until analysis.
3.2. DNA Extraction
The DNA was extracted using the KiaSpin® Tissue kit (Kiagen CA, Iran) according to the manufacture’s instructions. In order to determine the concentration of the sample absorbance at a wavelength to 260 nm was performed by biophotometer system (Eppendorf, Germany). In addition, to determine the purity of the sample wavelength of 280/260 and 230/260 was also examined.
3.3. PCR
In order to determine the quality of the extracted DNA, PCR amplification of the gene for human β-globulin was carried out (Table 1) [11]. The mixture reaction PCR for a reaction volume of 20 µL containing 10 µL prime taq premix (2x) (Kiagen CA, Iran), 3 µL of sterile distilled water, 1 µL of forward and rivers primers (TAG Compenhagen, Denmark), and 5 µL of DNA template. The PCR reaction was carried out in accordance with the schedule of time and temperature. As first denaturation 95ºC for 5 minutes, then 35 cycles of 95ºC for 50 seconds, 55ºC for 45 seconds, 72ºC for 40 seconds and finally 72ºC for 5 minutes final elongation was performed.
In order to reproduce the CMV genome of samples was performed using specific primers (Table 1) [11]. The mixture reaction PCR for a reaction volume of 20 µL containing 10 µL prime taq premix (2x) (Kiagen CA, Iran), 3 µL of sterile distilled water, 1 µL of forward and rivers primers (TAG Compenhagen, Denmark), and 5 µL of DNA template. The PCR reaction was carried out in accordance with the schedule of time and temperature. As first denaturation 95ºC for 5 min, then 35 cycles of 95ºC for 50 seconds, 60ºC for 45 seconds, 72ºC for 40 seconds and finally 72ºC for 5 min final elongation was performed. Then 5 µL of the PCR product on a 1.5% agarose gel was taken.
3.4. Statistical Analysis
Statistical analysis were performed using the SPSS-20 (SPSS, Inc., Chicago, USA) software package. The relationship between the prevalence of CMV and occurrence of ulcerative colitis and also compared with control group tissue samples were analyzed using the t-test and χ2 test. Statistical significance was accepted at the 5 percent level.
| Primer | Sequence | Size, bp |
|---|---|---|
| 106 | ||
| F | 5’ TCCAACATCAACATCTTGGT 3’ | |
| R | 5’ TCCCCCAAATTCTAAGCAGA 3’ | |
| 167 | ||
| F | 5’ GTCACCAAGGCCACGACGTT 3’ | |
| R | 5’ TCTGCCAGGACATCTTTCTC 3’ |
4. Results
In patients with ulcerative colitis, CMV DNA was found in 80% of samples (4 of 5). CMV DNA was found in 30% of patients in the control group of non-malignant (9 of 30). Statistical analysis showed significant association between the prevalence of CMV and incidence ulcerative colitis in comparison with the control group (P = 0.03).
The results showed that the highest prevalence of CMV in patients with ulcerative colitis older than 55 years (60%) and in non-malignant control group in two age groups of 35-55 years (13.3%) and under 35 years (13.3%). In terms of gender, the highest prevalence of CMV in patients with ulcerative colitis in both of two gender women (40%) and men (40%), and in non-malignant control group women (16.6%) have been observed.
Statistical analysis showed no significant association between the prevalence of CMV, age group and gender, in patients with ulcerative colitis in comparison with control group.
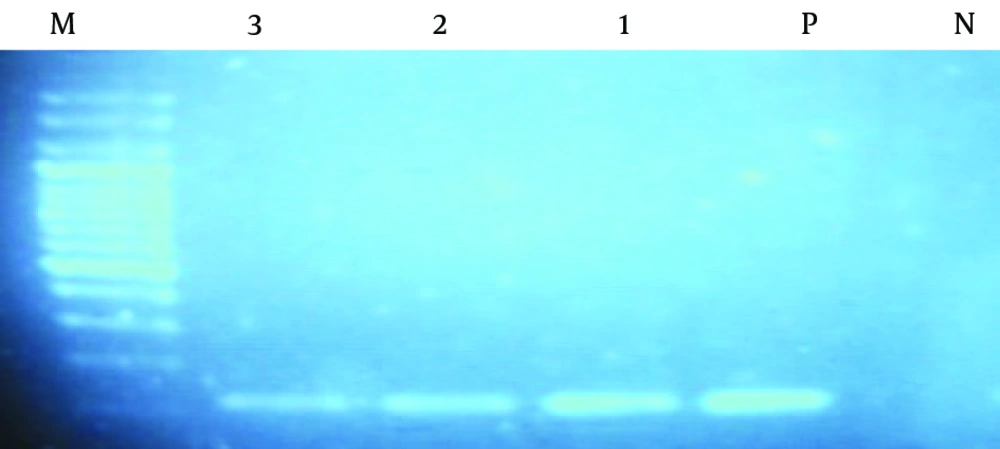
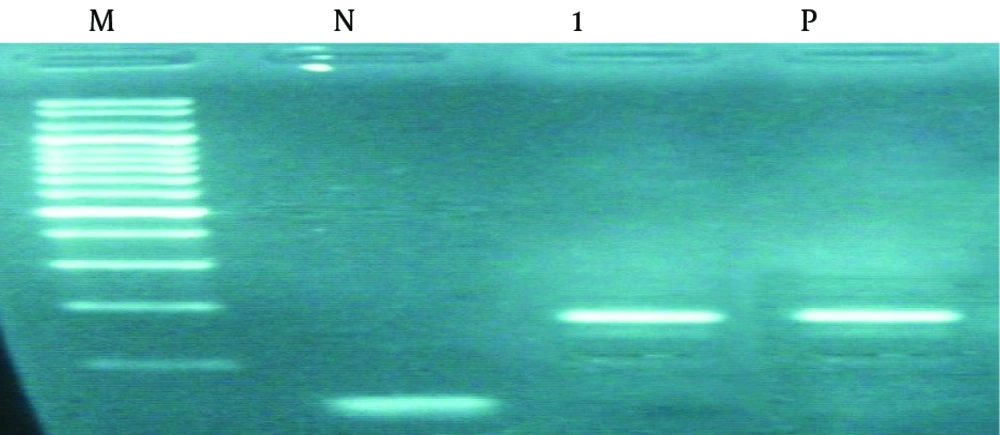
In all tissue samples 106 bp band that represents the amplification of human β-globulin gene observed (Figure 1). Due to the quality and reliability of DNA extracted, PCR analysis with CMV specific primers was performed; 167 bp bands that represent the replication is observed (Figure 2).
DNA extracted from tissue samples was amplified for β-globulin gene using primers described in methods.Amplification yielded a band of 106 bp. As positive control (P), human DNA from fresh tissue was used; as negative control (N), PCR master mix without DNA was used. Clinical samples, lanes 1 - 3. DNA molecular weight marker, M.
5. Discussion
In this study, we investigated ulcerative colitis and non-malignant tissues for the presence of CMV DNA by PCR method. Results showed that the prevalence of viral DNA in specimens of ulcerative colitis 80% and 30% in non-malignant control group.
Cytomegalovirus is an opportunistic pathogenic microorganism. During recent years, a clear association between complicated courses of ulcerative colitis and the presence of cytomegalovirus has been established. The exact pathogenic role of cytomegalovirus in these patients remains unclear despite a great number of published reports. Powell et al. [12] first reported the association of cytomegalovirus with ulcerative colitis in 1961. CMV infection in ulcerative colitis patients, especially in those who are immune-compromised by steroid therapy, can produce severe systemic disease and often leads to colectomy, but the coincidental diagnosis of UC and CMV colitis has also been reported [13-16]. However, the importance of CMV as an exacerbating factor of UC is neglected by many clinicians. PCR has emerged as the most sensitive laboratorial method for diagnosis of viral infection including that with CMV [15]. In the current study has shown the presence of CMV sequences in ulcerative colitis tissues and non-malignant by PCR method reflects the ability of the virus to infect of the different colon cells. These results suggested a possible causative association between CMV and ulcerative colitis. In the study by Dimitroulia et al. [4] in the intestinal tissue CMV genome was detected in 32.9% of the IBD patients and only in 2.4% of the controls, also a significant association was detected between CMV intestinal infection and either ulcerative colitis or Crohn’s disease, although the association was even stronger for patients with ulcerative colitis. Hommes et al. [14] evaluated the pathogenicity of cytomegalovirus in inflammatory bowel disease; their results showed CMV causes significant clinical morbidity in IBD patients. Kishore et al. [15] investigated infection with cytomegalovirus in patients with inflammatory bowel disease, sixty-three patients with IBD (both UC and CD) were selected, results showed CMV infection in patients with IBD may be common, this has definite clinical significance and therefore should not be ignored. Although our results confirmed the results of Dimitroulia et al. [4], Hommes et al. [14] and Kishore et al. [15] indicating that there is association between CMV infection and progression of inflammatory bowel disease. However, in other studies, no evidence of a direct association between inflammatory bowel disease and CMV infection was found [16, 17]. In the study by Yi et al. [16] on the prevalence and risk factors of cytomegalovirus infection in inflammatory bowel disease in Wuhan, central China, 226 IBD patients (189 ulcerative colitis and 37 patients with Crohn’s disease) were selected, CMV DNA was detected by nested PCR, their results showed no risk factor was found to be significantly correlated with CMV infection in risk factors analysis. Also, Leveque et al. [17] found no relationship between CMV viral load and disease severity in patients with active IBD.
In conclusion, our observations, suggest that UC patients have a predisposition to CMV infection as compared to healthy individuals, but the etiologic link between UC and CMV infection needs to be studied.