1. Introduction
Thymoma is accounting for most of anterior mediastinal mass in adults. Paraneoplastic syndromes with autoimmune basis are frequently founded in patients with thymoma. Very rarely there are multiple simultaneous paraneoplastic syndromes in one patient with thymoma. Thymoma with an adult-onset immunodeficiency is called Good’s syndrome. According to a systematic review by Kelesidis and Yang [1], pure red cell aplasia (PRCA) is occurring in 34.8% of cases with Good’s syndrome. Cases of diffuse panbronchiolitis (DPB) associated with “Good syndrome” or thymoma alone has also been reported [2]. Thymoma is also reported as a complication of DPB [3]. Despite frequently reported of paraneoplastic syndromes in concomitant with thymoma, here is a unique case of thymoma with multiple rare comorbodities and complications.
2. Case Presentation
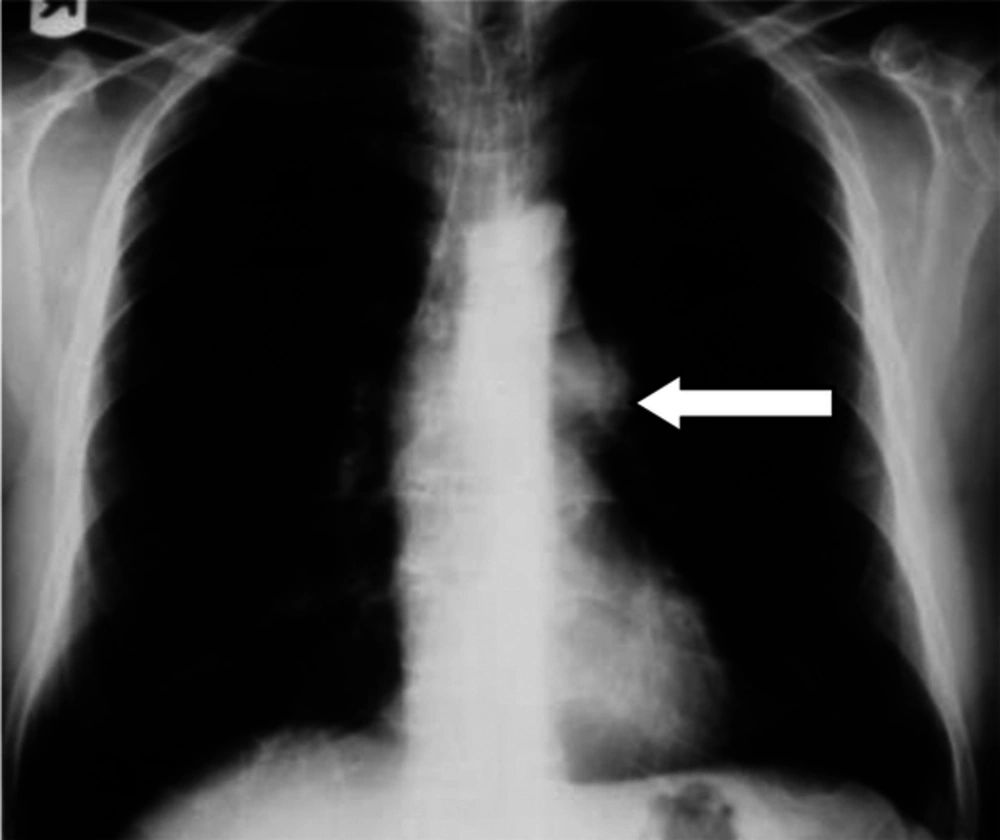
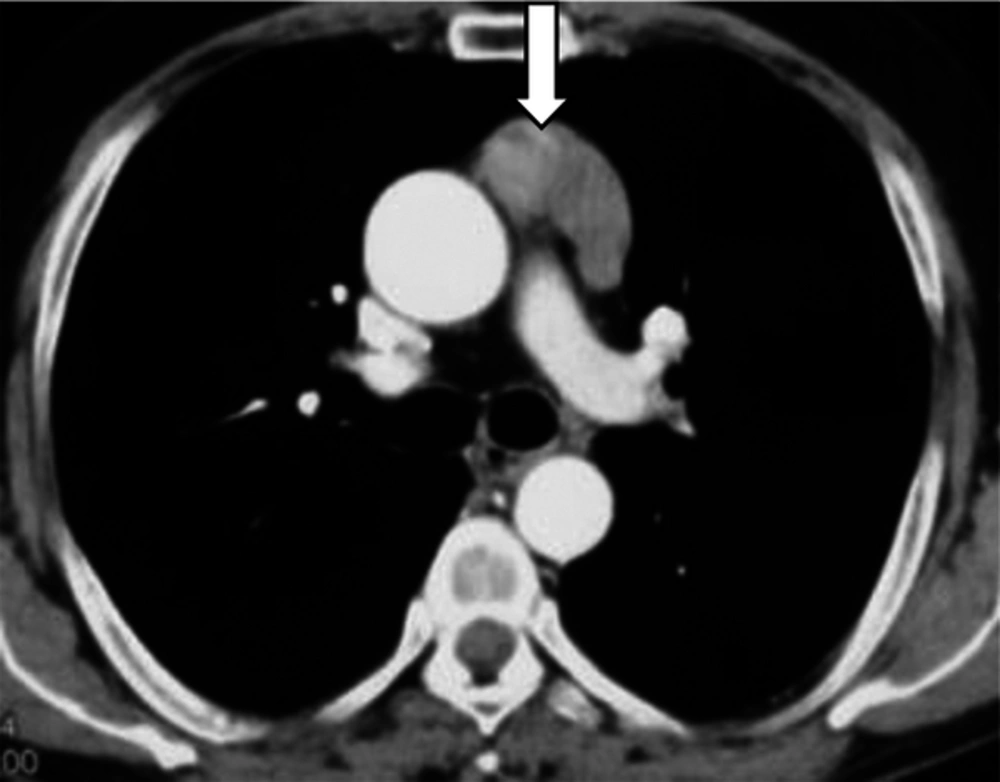
A 62-year-old non-smoker man with diagnosis of ulcerative colitis taken placed on prednisone and sulfasalazine 3 years ago. After 8 months of treatment, symptoms subsided and the patient stopped taking the drug without consulting the physician. Then, he had experienced recurrent attacks of respiratory sign and symptoms. Chest X-ray (CXR) and thoracic computed tomography (CT) scan determined an anterior mediastinal mass compatible with thymoma (Figures 1 and 2).
Lung high-resolution computed tomography (HRCT) showed ground glass images, nodules and bronchiectasis. Pathologist’s report on transbronchial biopsy was lymphoplasma cell inflammation. Ziehl-Neelsen staining on smear of bronchoalveolar lavage was negative. Laboratory findings included urea, creatinine, urine analysis, cytoplasmic anti-neutrophil cytoplasmic antibodies (C-ANCA), perinuclear anti-neutrophil cytoplasmic antibodies (P-ANCA) and rheumatoid factor (RF) test were not remarkable, but antinuclear antibody (ANA) test showed an increased up to 25 U/μL (positive test > 18). ESR and LDH was elevated top to 75 and 544 U/L respectively. Immune electrophoresis revealed IgG = 644 (Normal: 800 - 2,100 mg/dL), IgM = 23 (Normal: 50 - 320 mg/dL), IgA = 55.6 (Normal: 100 - 470 mg/dL) and IgE = 1 IU/mL. HIV testing was negative. Because of productive cough, ciprofloxacin and erythromycin was started. The patient’s condition improved. Ciprofloxacin was discontinued and erythromycin reduced to 400 mg/day and continued. Influenza and pneumococcal vaccination was carried out. Six months after starting erythromycin, sudden drop in hemoglobin occurred (Hb = 5.5 g/dL, reticulocyte count = 1.8%). Erythromycin was discontinued. Red cell hypoplasia made on study of bone marrow biopsy. Recurrent blood transfusion was performed. However rapid drop in hemoglobin recurred after each transfusion.
Surgical resection of anterior mediastinal mass was labeled as encapsulated thymoma type AB. Anemia did not improve four months lapsed from surgery. Prednisolon (50 mg/day) and cyclosporine (100 mg/day) were started. One month later the patient developed sever pneumonia, leukopenia (WBC = 1300/μL), hypoxia and respiratory acidosis. Treatment with vancomycin, clindamycin and imipenem was started. The patient was intubated and ventilation with low tidal volume strategy started. Blood culture was positive for streptococcal pneumonia susceptible to vancomycin.
Condition of patient was more complicated by atrial fibrillation, hypotension, azotemia, hyperglycemia and thrombocytopenia and lead to cardiac arrest and death.
3. Discussion
As a complication of ulcerative colitis, thymoma has not been reported till now. However there are reports about synchronization of ulcerative colitis with thymoma and improvement or remission after thymoma resection [4]. The second major problem was respiratory symptoms and hypogammaglobulinemia. Considering high antinuclear antibody (ANA) titer, bronchiectasis, ground glass opacity and nodule on lung HRCT and good response of respiratory symptoms to erythromycin, lead us to diagnosis of DPB syndrome. Anti-inflammatory properties of low-dose erythromycin have shown therapeutic effects in DPB [5]. Coexistence of thymoma and hypogammaglobulinemia is called Good's syndrome. DPB is reported with Good syndrome [2].
Thymoma has been also reported as a complication of DPB [2, 3].
Severe anemia was the third major complication. In view of the potential side effects of erythromycin, the Medline search provide just one case report of erythromycin induced anemia in a 84 old man with congestive heart failure (CHF) who was concomitant on therapy with furosemide [6]. With regard of red cell aplasia on bone marrow biopsy, hypogammaglobulinemia and thymoma; anemia can be explained in relation to Good’s syndrome [1]. In the latest episode, the patient was suffering from pneumococcal pneumonia and sepsis. Hypoimmunoglobulinemia and drug induced immunosuppression predisposed the patient to infection.
Only a few cases of hypoplastic neutropenia or amegakaryocytic thrombocytopenia were reported in patients with thymoma [7, 8]. It was assumed that thrombocytopenia and neutropenia were more fitted by sepsis and cyclosporine induced bone marrow suppression in the present case. The patient had no history of diabetes or family history of diabetes. Hyperglycemia during hospitalization, may be caused by sepsis related stress and corticosteroids use during hospitalization. Now it cannot be linked to thymoma. Concomitant of multiple paraneoplastic syndromes in single patient with thymoma as introduced here is very rare.