1. Background
Pain is a common complication after all surgeries and pain management has an imperative role. Adverse side effects through non-adequate pain management, such as atelectasis, ventilation-perfusion mismatch, hypoxia, hypercapnia, systemic hypertension, tachycardia, myocardial ischemia, dysrhythmia, hyperglycemia, deep vein thrombosis, and platelet aggregation, has been reported in several studies (1-5). Moreover, mismanagement of pain through surgery could lead to chronic pain after surgery (6).
Postoperative pain is usually managed both pharmacologically and non-pharmacologically, each with their own advantages and drawbacks. Opioids and NSAIDS are common drugs administered for post-operative pain, however, they all have the probability of gastrointestinal, renal, and respiratory complications (5). Given the mentioned factors, it seems crucial to find better means to alleviate post-operative pain management with minimal side effects.
A feasible field to attenuate postoperative pain is intraoperative hemodynamic parameters. The association between mean arterial pressure and reduced perception of pain in human and animal models have been studied (7).
Intraoperative hypertension and hypotension have been reported in relationship to post-operative pain and other morbidities (8-11). Although permissive hypotension has long been introduced for decreasing the risk of intra-operative bleeding, it might increase post-operative pain12. Furthermore, central and peripheral hyperalgesia through traumatic injury and surgical damage could provoke post-operative pain (6).
This study was conducted to elucidate the effect of intraoperative hypertension on post-operative pain in patients undergoing hysterectomy and to examine the baseline and relative intraoperative blood pressure changes in order to manage postoperative pain management.
2. Methods
The study was approved by the Ethics Committee of Iran University of Medical Sciences (Approval No. = 94/D/105/1387). Informed consent was obtained from all participants. The information of the patients remained confidential. The trial was conducted during January to April 2017 at Firoozgar Hospital, a university affiliated hospital, Tehran, Iran. It had also been registered at Iranian Registry of Clinical Trials site (IRCT No.: IRCT2015112916151N4).
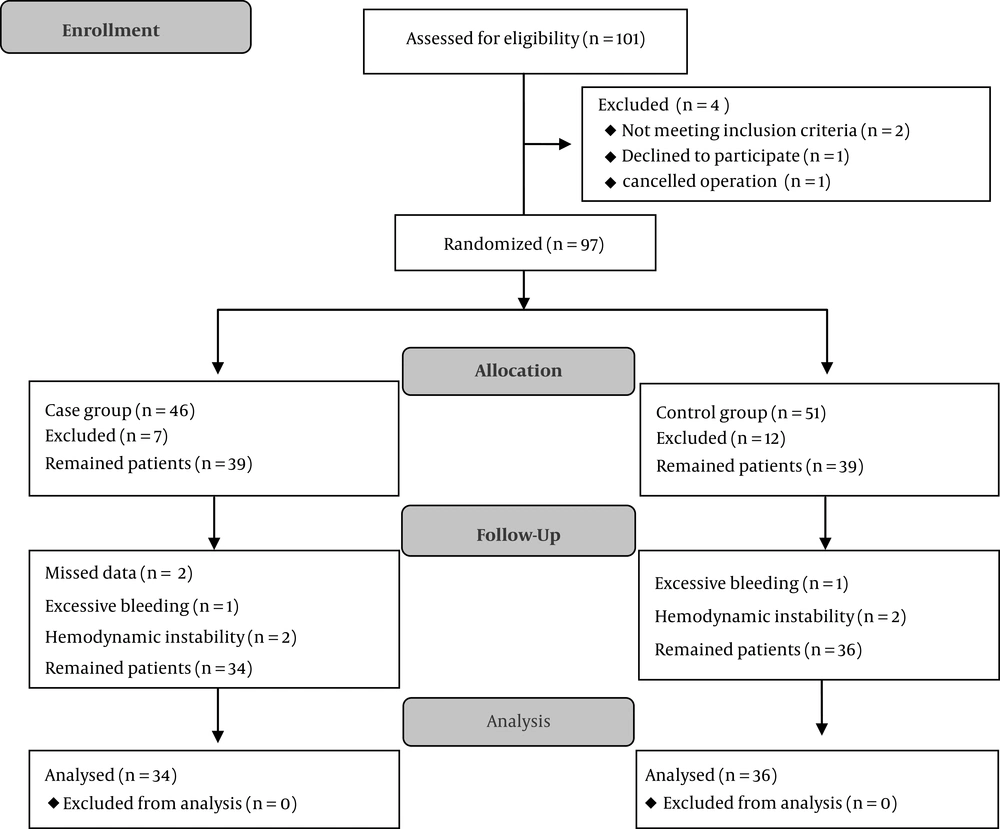
In this randomized controlled clinical trial, 78 patients, candidate for hysterectomy with past medical history of hypertension were simply randomized to two groups (Figure 1) by the date of surgery (odd or even days) and 70 were analyzed.
Based on a previous study (12) and considering Power = 90% and α = 0.05, sample size was calculated equal to 36 in each group (by online calculator available from the University of British Colombia, Vancouver, BC, Canada).
Inclusion criteria were presence of hypertension, female gender consuming antihypertensive drugs, age of between 40 and 60 years with stage 1 (SBP = 140 to 159mmhg, DBP = 90 to 99 mmHg) or stage 2 (SBP ≥ 160 mmHg and DBP = 100 to 110 mmHg) of hypertension on the day of surgery. Patients with analgesic drug consumption (opioids and non-opioids) in the past week before surgery, chronic pain, known cerebrovascular and cardiac disease, major intraoperative bleeding, vasoactive drug usage, and those with permissive hypertension causing disturbance in the surgical field (surgeon complaint about bleeding and unclear surgical field) were excluded from the study.
After volume loading with 5 mL/kg normal saline, standard monitoring and pre-oxygenation with 100% oxygen was administered to all participants. The depth of anesthesia was monitored with BIS and was maintained between 40 and 60 during the operation. Fentanyl 3 mcg/kg, midazolam 0.25 µg/kg, etomidate 0.2 mg/kg, and cisatracurium 0.2 mg/kg were administered for induction. Sufentanil 1 μ/kg/h, propofol 100 to 150 μ/kg/h, and cisatracurium 2 μ/kg/min were infused as maintenance. Group A were patients with hypertension in stage one to two, who were operated on odd week days and their blood pressure were maintained in the range of stage 1 with the dose adjustment of the maintaining anesthetic drugs. If the blood pressure declined to lesser than stage 1, in group A patients, it was supposed to decrease to 20% to 30% in previous infusion dose of propofol and keep the BP in specified range and BIS < 60, otherwise in failure to keep these conditions, the case was excluded. Group B were patients with hypertensive stage one to two, which were operated during even days and their blood pressure were maintained in the normal range (SBP ≤ 120, DBP ≤ 80) by increasing propofol dose and administration of TNG infusion during the surgery with the consideration of mean arterial pressure (MAP) not dropping more than 25% of baseline. Infusion of sufentanil and cisatracurium was discontinued after 30 minutes and propofol was held 10 minutes before the end of the surgery and at the end of the surgery, 1 g of paracetamol was administered to all patients.
Demographic data (age, weight, and concomitant disease), preoperative and intra operative data (hemoglobin, hematocrit, blood pressure, heart rate, operating time, and blood loss) and recovery data, including blood pressure, heart rate, and pain score at “two, four, six, 12, and 24 hours” using VAS (after surgery), and pain relief medicine requirements after 24 hours were recorded for all patients. The patients and the anesthesia resident, who were in charge of assessment of postoperative pain were blind during the study.
In participants with VAS score > 3, 0.5 mg/kg pethidine was injected, intravenously. It could be repeated after 20 minutes at the patients’ request and in cases with VAS score > 3. If the total doses of pethidine were more than 100 mg and in refractory pain, 0.1 mg/kg morphine sulfate was infused slowly.
Statistical analysis was performed with Statistical Package for Social Sciences (SPSS) version 22.0 (SPSS Inc., Chicago, IL, USA). Mann-Whitney U-test and pair t-test served to compare differences in non-parametric and numerical data, respectively. Repeated-measure analysis of variance test was also used for analysis of data during the surgery. P values of < 0.05 were considered statistically significant.
3. Results
Demographic and intraoperative data are shown in Table 1. No differences were found in age, gender, and anesthesia history between subjects (P > 0.05).
| Data | Group A | Group B | P Value |
|---|---|---|---|
| Age, y | 46.83 ± 6.61 | 49.16 ± 10.11 | 0.14 |
| Weight, kg | 78.11 ± 14.51 | 72.88 ± 13.73 | 0.92 |
| Concurrent disease | 0.35 | ||
| DM | 10 (29.4) | 4 (11.1) | |
| Thyroid disease | 2 (5.9) | 6 (16.7) | |
| CAD | 0 (0) | 2 (5.9) | |
| MR | 2 (5.9) | 0 (0) | |
| Fatty liver | 2 (5.9) | 0 (0) | |
| Asthma | 2 (5.9) | 0 (0) | |
| W/O | 16 (47.1) | 24 (57.1) |
Abbreviations: CAD, coronary artery disease; DM, diabetes mellitus; MR, mitral regurgitation, WO, without.
aValues are expressed as mean ± SD or No. (%).
Systolic blood pressure before surgery did not show any significant differences between the groups (P > 0.05). However, systolic and diastolic blood pressures were significantly lower in group B intraoperatively (P < 0.001 and P = 0.014, respectively). Moreover, both intraoperative bleeding and hematocrit levels (before and after surgery) showed no significant difference between groups. Also, BIS levels remained with no differences during the operation, Table 2.
| Group A | Group B | P Value | |
|---|---|---|---|
| Hematocrit, mg/dL | |||
| Before surgery | 36.65 ± 3.68 | 36.19 ± 6.97 | 0.82 |
| After surgery | 33.77 ± 3.23 | 32.99 ± 3.15 | 0.51 |
| Intraoperative Bleeding, mL | 408.33 ± 266.37 | 301.17 ± 144.99 | 0.30 |
aValues are expressed as mean ± SD.
Comparing VAS and need for pain relief drugs in both groups, no significant differences were found at “two, four, six, 12, and 24 hours” after surgery. However, a significant reduction of pain was observed in the hypertensive group from the 2th to 24th hour after surgery (P < 0.001), Table 3.
| Group A | Group B | P Value | |
|---|---|---|---|
| Pain scores (VAS) at:, h | |||
| 2nd | 4.55 ± 2.68 | 5.29 ± 2.54 | 0.40 |
| 4th | 5.72 ± 2.53 | 4.94 ± 2.35 | 0.41 |
| 6th | 5.27 ± 2.42 | 4.82 ± 2.21 | 0.75 |
| 12th | 4.44 ± 2.63 | 4.41 ± 2.45 | 0.16 |
| 24th | 2.55 ± 2.12 | 3.82 ± 4.75 | 0.63 |
| P value | 0.01 | 0.559 | |
| Pethidine consumption, mg | 40.38 ± 25.33 | 45.08 ± 18.22 | 0.59 |
| Morphine consumption, mg | 0.77 ± 0.73 | 0.82 ± 0.59 | 0.93 |
Abbreviation: VAS, visual analogue scale.
aValues are expressed as mean ± SD.
4. Discussion
The results of this study showed no significant differences between mean pain scores after abdominal hysterectomy between normal and high intraoperative blood pressure in patients with history of hypertension. Also, there were no significant differences between groups regarding post-operative opioids requirements. Repeated measure variance showed no significant difference between parameters studied at different times in this research and patients had similar severity of pain after surgery and analgesic requirements, according to statistics tests.
Postoperative pain is a common complication, which could be an unpleasant experience for patients (1). Implementation of intraoperative pain management leads to decreased use of postoperative drugs administered (13). On the other hand, many patients have accepted some levels of postoperative pain. Therefore, proper pain management renders acceptable insight and better service to the patients.
No exact and intact mechanism could be offered for anti-pain effect of hypertension. Vasopressin has been proved to have anti-pain properties in the spinal cord (6). Researches have shown that the normotensive group had higher VAS and more opioids administration (13). Phenylephrine can control pain by stimulation and release of vasopressin in the central nervous system. Increased blood pressure results in baroreceptor activity, which increases the pain threshold (12).
Previous studies indicated that both pain threshold and endurance are higher in the hypertensive group compared to the normotensive group (14). Also, it was shown that pain sensitivity had no relationship with past family history of hypertension. Hence, the higher rate of BP is more likely to decrease the sensitivity to pain than the genetic potential; high blood pressure may cause a decrease in pain sensation by leading and conducting the activities of endogenous opiates and stimulating the baroreceptor system (14). In another research, thermal stimulation on three points in volar foramen level and thermal pain threshold were measured. A significant relationship was shown between thermal pain threshold and increased blood pressure. They also clarified that beta-endorphins in the hypertensive group was surprisingly high, increasing the pain threshold in hypertensive patients (15). The baroreceptor reflex activity by stimulating mechanoreceptors and cranial nerves 9 and 10 stimulate which will decrease sympathetic and change the ability of stimulating the central nervous system.
Studies have shown the relationship between higher blood pressure before surgery and lower sensation to pain after surgery. Previous literature have found some effects of preoperative hypertension on postoperative pain (16), although the exact results related to all models are still a debate. Induced hypertension during surgery reduced postoperative analgesic requirements in one research (17). Deshaumes et al. found lower pain levels after oral surgery in patients with hypertension before the surgery (18). In another, hypoalgesia in people served as a valuable predictor of risk of hypertension in the future (19). A significant correlation between preoperative blood pressure and postoperative pain was observed in King et al.’s research (20).
Alteration in BP-pain sensitivity relationship in chronic pain due to dysfunction in pain regulatory systems has been proved by Bruehl et al.’s study (21). This finding and BP-pain correlation have been studied previously in another investigation by Maixner et al. and it was found that resting blood pressure could impair the central pain regulatory systems and change the patients’ sensitivity to noxious stimuli (22).
However, findings of Bruehl et al. and Maixner et al. and their colleagues are consistent with the current study and did not reveal any relationship between blood pressure and pain scores (21, 22). During year 2015, a similar study concluded no significant differences between pain scores at two, four, six, 12, and 24 hours after surgery in the controls (systolic blood pressure kept at 20% to 30% lower than baseline) and the hypertensive group (20% to 30% higher than baseline) (12). However, Luo et al. conversely concluded that one to six hours after abdominal hysterectomy, the controls had more pain scores than the hypertensive group. Despite this, similar to the current study, no significant differences were revealed at 12 and 24 hours after surgery (16). There are reported relationships between pre and postoperative hypertension and decline in pain scores. Also, intraoperative hypotension (MAP ≤ 50) has shown to effect postoperative morbidity and mortality.
Opioids requirements in hypertensive participants was lower compared to the normotensive counterparts, which was in agreement with previous studies, however, the current study had differing results (1, 17).
This discrepancy between the current study and other studies might be because of the design of the current study for the control and hypertensive group or the time pain score was measured after surgery. For example the difference between blood pressure in the current study before and after surgery is not tremendously different compared to other studies. Furthermore, the current researchers recorded pain scores two hours after surgery, whereas other studies calculated it immediately after surgery (16-18). Another conflict could be related to different time of pain assessment and the time of injection of pain killer drugs, thus, VAS in patients could be influenced by analgesics request by the patients and pain perception may have been recorded within a lower range.
The current study did not find any statistically significant differences between hemodynamic variables (systolic and diastolic blood pressure, heart rate and BIS) between groups before and during surgery. Furthermore, no difference was found between surgery duration, bleeding, extubation time, and the first necessity of pain relief drugs in groups. Delfino et al. (12) in their research on laparoscopic cholecystectomy found the same results as the current study.
Other studies used acute vasopressors and induced hypertension for their patients, which could have played a role in inducing mediators and pain control. However, in the current study, patients had chronic hypertension and vasopressors were not used. Also, time of hypertension could also have an effect in inducing pain, which was not considered and compared in the current study.
The current research had some limitations. Limitations of the current study include small study sample. Also, this study observed patients in stage 1 or 2 of hypertension, which restricted to determine the possibility of stronger relationship of other subtypes of hypertension with hypertensive hypoalgesia.
4.1. Conclusions
Finally, the current results showed no significant differences between pain score and opioid requirements at two, four, six, 12, and 24 hours after surgery in hypertensive patients compared to normotensive, during abdominal hysterectomy. Females undergoing hysterectomy with high MAP during surgery had no significant differences associated with pain scores and post-operative pain relief drugs requirements. Future studies should be conducted for best understanding of the role of intraoperative blood pressure and post-operative pain levels.