1. Background
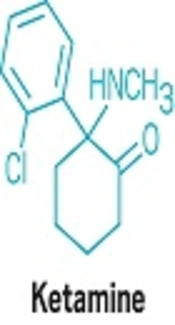
Ketamine is a derivative of phencyclidine and an intravenous anesthetic drug, which was used clinically for the first time in 1965. This drug is different from most other intravenous anesthetic agents in terms of causing significant analgesia (1). However, its use is limited due to complications, such as nausea and vomiting, psychiatric side effects, increased secretion, elevated heart rate (HR), and blood pressure (2). Propofol is another drug used for sedation. Propofol (2,6-diisopropylphenol/DIPP) is an alkylphenol with hypnotic properties. It is probably the most common anesthetic medication used for induction of anesthesia. In addition, propofol is a selective drug for maintenance of anesthesia and sedation in the operating room and intensive care unit. Propofol, more than any other anesthetic drug, leads to vasodilatation and dramatically reduces arterial blood pressure. Moreover, it significantly inhibits normal pressure reflex response. Propofol slightly increases the HR, and this enhances hypotensive effect of the drug. Severe bradycardia and asystole can be complications in healthy adults (1).
In the recent years, numerous studies have been performed on the drug combination of ketamine and propofol (ketofol). Ketamine due to the increase in blood pressure improves hemodynamic changes of propofol and its sedative effect causes a reduction in the dose of propofol in combination. On the other hand, propofol has antiemetic effects and reduces the psychiatric side effects of ketamine through the strong sedative effect. As a result, this combination seems to be ideal in sedation (3-14).
Aydogan et al. investigated the recovery time and hemodynamic effects of combination of ketamine and propofol compared to propofol alone in patients undergoing endoscopy. The researchers claimed that the combination of propofol and ketamine lead to shorter recovery time and better hemodynamic stability (7).
Shah et al. compared ketofol and ketamine in children aged between 2 and 17 years and showed that recovery time was shorter and nausea and vomiting were lower in the ketofol group (15).
Also, Singh et al. studied ketofol mixed at 4:1 ratio compared with propofol alone in children aged between three and eight years old. The results showed that the effect of using ketofol in sedation during spinal anesthesia is more effective than propofol alone and the risk of respiratory depression is also less in the ketofol group (16).
All studies have used the combination of propofol and ketamine (within a syringe) as a new drug called ketofol. Sometimes concurrent use of two injectable drugs in unit syringe or in an intravenous infusion solution results in sedimentation, gas production, changes in pH or change in the color of the solution (17). Although there are investigations on the therapeutic effects of ketofol, yet the complications of combined drugs have not been examined in any of the studies. In combining the two drugs, the possibility of drug interactions should be consistently considered though they are not visible in appearance and with naked eyes. The present study was designed to investigate the effect of ketofol compared with ketamine plus propofol on hemodynamic status of patients undergoing transurethral lithotripsy (TUL) to avoid combining the two drugs when there is no difference in the therapeutic and hemodynamic effects of injecting this drug combination.
2. Methods
This quasi-experimental study was carried out during year 2015 on patients undergoing TUL at the operating room of Moradi Hospital, Iran.
Inclusion criteria were patient satisfaction, age of between 15 and 45 years, ASA physical status class 1 or 2, no history of cardiovascular disease, thyroid disease, epilepsy, seizures and hepatitis, no history of allergy to eggs and soy, and no history of airway problems. Exclusion criteria included difficulties in airway management, difficult intubation, history of taking narcotics, alcohol and painkillers, and emergency TUL surgery.
The sample size was calculated as 20 people for each group through the formula of the mean difference between the two independent communities and taking in account α = 0.5% and β = 0.20% (13). The patients entered in the study were assigned randomly (using 20 sealed envelopes with the mark of A = ketofol and 20 sealed envelopes with the mark of B = ketamine plus propofol) to one of the two groups. Intravenous access was done for the patients in the surgery ward. On admission to the operating room and after placement on a bed, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), HR, and oxygen saturation of arterial blood (O2Sat) were primarily recorded for the patients via SAZGAN model monitoring system (made in Iran). Overall, 5 mL/kg of ringer solution was infused before anesthesia and 2 µg/kg of fentanyl was administered as premedication of anesthesia. In the patients of the ketofol group, mixture of 1 mg/kg of propofol and 1 mg/kg of ketamine were drawn in a single syringe and were then injected. In the patients of ketamine plus propofol group, 1 mg/kg of propofol and 1 mg/kg of ketamine were drawn in a separate syringe and were injected consecutively (1, 14). The syringes were marked with A and B symbols. In both groups, 0.5 mg/kg of atracurium was used as muscle relaxant, and one anesthesiologist performed the endotracheal intubation. During the surgery, N2O 50% and O2 50% with isoflurane of MAC = 1% were used for maintenance of anesthesia. Then, a third anesthesia technician, who was unaware of the used drugs (double-blind study: The person who injected the medicine, the person who intubated, and the person who wrote vital signs did not know what medicine were injected) recorded SBP, DBP, MAP, HR and O2Sat for the patients at 1, 5, 10 and 15 minutes after endotracheal intubation (7). The obtained data were analyzed using SPSS V. 16 software and statistical tests, including mean, frequency, Independent t-test, and Chi-square, and P < 0.05 was considered significant.
The statistical test of Kolmogorov-Smirnov was used for evaluation of the normality of data (P > 0.05).
3. Results
The mean age of participants was 37.34 ± 8.33 years and the age group of 31 to 45 years accounted for the highest percentage. A total of 20 patients were included, the ketofol group had four females (20%) and the ketamine plus propofol group had six females (30%). Chi-square test showed that this difference was not significant between the two groups (P = 0.87).
In the ketofol group, the maximum frequency was related to the age group of 31 to 45 years (90%); and in the ketamine plus propofol group, the highest frequency was observed in the same age group (65%). Independent t-test revealed that this difference was not significant between the two groups (P = 0.71).
Table 1 shows mean ± SD of SBP of the patients at different times of surgery in the ketofol and ketamine plus propofol groups.
| Ketamine Plus Propofol Group, mmHg | Ketofol Group, mmHg | P Valuea | |
|---|---|---|---|
| Pre operative | 147.95 ± 23.42 | 135.05 ± 13.33 | 0.39 |
| First minute | 123.80 ± 23.04 | 125.90 ± 19.62 | 0.75 |
| Fifth minute | 135.55 ± 29.46 | 124.60 ± 18.65 | 0.16 |
| Tenth minute | 120.80 ± 28.20 | 115.40 ± 16.65 | 0.46 |
| Fifteenth minute | 116.00 ± 20.48 | 114.20 ± 13.15 | 0.74 |
| P valueb | 0.001c | 0.000c |
a Independent t-tests.
b Repeated measures.
c P < 0.05.
As shown in the table, the difference of the mean SBP of the patients at different times was significant, but no significant difference was observed between the two groups. In Table 2, mean ± SD of DBP of the patients at different times of surgery in the ketofol and ketamine plus propofol groups was investigated and statistical analysis showed no significant difference.
| Ketamine Plus Propofol Groupa, mmHg | Ketofol Groupa, mmHg | P Valueb | |
|---|---|---|---|
| Pre operative | 86.20 ± 12.21 | 84.95 ± 9.42 | 0.71 |
| First minute | 74.95 ± 14.78 | 79.30 ± 14.13 | 0.34 |
| Five minutes | 77.25 ± 25.11 | 79.05 ± 13.08 | 0.77 |
| Ten minutes | 86.75 ± 22.80 | 71.85 ± 16.57 | 0.62 |
| Fifteen minutes | 68.10 ± 22.04 | 70.20 ± 11.84 | 0.71 |
| One-way ANOVA | 0.035c | 0.004c |
aValues are expressed as mean ± SD.
bIndependent t-tests.
cP < 0.05.
According to the results of Table 2, the difference in mean DBP in patients at different times was significant, yet no significant difference was observed between the two groups. Table 3 compares the mean ± SD of MAP criteria at different time points of surgery in the ketofol and ketamine plus propofol groups, indicating no significant difference between the two groups.
| Ketamine Plus Propofol Groupa, mmHg | Ketofol Groupa, mmHg | P Valueb | |
|---|---|---|---|
| Pre operative | 90.52 ± 11.43 | 90.37 ± 11.00 | 0.17 |
| First minute | 89.65 ± 16.85 | 91.75 ± 17.08 | 0.69 |
| Five minutes | 96.60 ± 28.72 | 89.50 ± 13.17 | 0.32 |
| Ten minutes | 86.40 ± 24.64 | 85.08 ± 16.83 | 0.84 |
| Fifteen minutes | 83.10 ± 21.23 | 84.40 ± 11.88 | 0.81 |
| One-way ANOVA | 0.009c | 0.004c |
aValues are expressed as mean ± SD.
bIndependent t-tests.
cP < 0.05.
Mean arterial blood pressure changes were significant in both groups at different times, yet there was no significant difference between the two groups in this regard. Table 4 demonstrates the comparison of the mean ± SD of HR at different time points of surgery in the ketofol and ketamine plus propofol groups. There was no significant difference between the two groups.
aValues are expressed as mean ± SD.
bIndependent t-tests.
cP < 0.05.
Table 5 shows the mean ± SD of arterial blood oxygen-saturated hemoglobin (O2Sat) at different time points of surgery in the ketofol and ketamine plus propofol groups. The statistical test did not show a significant difference.
aValues are expressed as mean ± SD.
bIndependent t-tests.
cP < 0.05.
Mean oxygen saturation changes were significant in the ketofol and ketamine plus propofol groups at different time points, yet there was no significant difference between the two groups.
4. Discussion
The current research was conducted to examine the effects of ketofol compared with the effect of ketamine plus propofol on hemodynamic status of patients undergoing TUL.
In studies conducted so far, ketofol combination with other sedatives, such as midazolam, propofol or narcotics has always been compared with each other. The combination of ketofol in a syringe and ketamine plus propofol in separate syringes has not been examined in any study. Therefore, the current study attempted to compare the findings of this study using the most relevant articles and their results.
The findings demonstrated that the mean age of participants was 37.34 ± 8.33 years and the age group of 31 to 45 years accounted for the highest percentage, in line with studies by Andolfatto and Willman and Aydogan et al. (6, 7). According to the scientific evidence, kidney stone symptoms usually appear after the age of 30 years, and this justifies a higher frequency of samples studied in this age range in the current study (18).
A total of 40 patients, males constituting 75% of patients (n = 30), were recruited. This result is consistent with studies by Andolfatto and Willman and Aydogan et al. (6, 7), and could be due to smoking and poor diet in males than females. Scientific findings also suggest that, the incidence of kidney stones in males is four times higher than females (18).
The mean difference of SBP of the patients in the study was not significant in both groups, consistent with the study of Dal et al. in 2014. In this study, 60 patients for endobronchial aspiration were divided to two ketamine-midazolam and ketofol groups and then SBP was measured at different time points during surgery. At the end, the results reveal that difference in SBP was not significant between the two groups (13). They attributed the lack of significant difference between the two groups to the fact that the propofol has sedative effects on the cardiovascular system hemodynamic status of the patients, and can neutralize the effects of ketamine.
Also, in 2013, Aydogan et al. studied the recovery time and hemodynamic effects of ketamine and propofol combination compared with propofol alone in 100 patients undergoing endoscopy. For this purpose, they measured vital signs, such as SBP at different time points. At the end, it was said that the SBP difference was not significant in the two groups; this finding is in line with the results of the current study (7). The lack of significant difference in the two groups was probably because ketamine leads to an increase in blood pressure in both treatment groups. On the other hand, propofol keeps blood pressure in the normal range, because of blood pressure lowering effects.
The present study showed that, the mean DBP was not significantly different between the two groups. This result is consistent with the studies of Aydogan et al. and Dal et al. (7, 13). The lack of differences between the two groups is probably due to the short interval between injections of ketamine and propofol in the ketofol and ketamine plus propofol groups and ketamine being injected immediately after propofol. As a result, ketamine and propofol improve hemodynamic fluctuations of each other.
The other finding of the present study was that the MAP of the patients was not significant in both groups, confirming the studies of Dal et al. (13) and Aydogan et al. (7), since the MAP is calculated according to systolic and diastolic pressures. It is natural that the MAP has no significant difference between the two groups. In the present research, the mean HR and O2Sat level of the patients showed no significant differences between the two groups. This finding is confirmed by studies of Dal et al. and Aydogan et al. Because in both groups the patients were intubated and had controlled ventilation, the two groups had no difference in the O2Sat level.
4.1. Study Limitations
The authors found no studies that reported findings inconsistent with the results of the present study.
4.2. Conclusion
The present study was a new research to compare the drug combination. It was found that the two groups had no significant differences in hemodynamic status. As a result, there is no need to combine the two ketamine and propofol drugs to build a new compound called ketofol to avoid possible complications and interactions of ketamine and propofol drugs.