1. Background
Mother’s death during pregnancy or up to 42 days after the labor is defined as maternal mortality excluding the death caused by accidents [1]. Maternal mortality indicates the situation of women in a society, access to the required cares, quality and efficacy of the cares, capacity of caring system in response to a mother’s needs and finally level of socioeconomic status of the society [2]. Most of maternal deaths which occur almost instantly after the delivery are associated with heavy bleeding [3]. The causes of maternal death are not similar in different studies but in Iran the most common causes are the following: bleeding, hypertension, infection, hard labor [4, 5].
Many of mothers having complications of the delivery are transferred to ICU. Some of these mothers unfortunately die. Dissimilar manners are used to diagnose their severity of the complication and estimate the patient’s death probability [6]. One of these approaches is called APACHE II scoring system which is very practical and highly recommended worldwide [7, 8].
Acute physiology and chronic health evaluation is another severity of disease classification. It is applied within 24 hours of admission of a patient to an intensive care unit. Higher scores correspond to more severe disease and higher risk of death [9].
In the beginning, APACHE scoring system was so complex and confusing, until Knaus et al. made some modifications and then APACHE II was born that included 12 parameters, despite introducing many newer systems APACHE II stands between the most practical systems ever designed [8-10].
APACHE II has three components:
1- Acute physiologic signs including: rectal core temperature, respiratory rate, pulse rate, serum creatinine level, serum potassium level, mean arterial pressure, oxygenation level concerning receiving oxygen level and alveolar-arterial oxygen gradient, hematocrit level, white blood cell count, serum bicarbonate level, GCS level, and arterial blood pH.
2- Patient’s age
3- A positive history of previous chronic illness including elective or emergent surgical procedure [11-13].
It has to be mentioned that the most severe sign and highest lab results are recorded during first 24 hours and considered in the scoring system. According to APACHE.II scoring system, the scores of 0 - 15, 16 - 19, 20 - 30, and higher than 30, are associated with related death probability, respectively: 10%, 15%, 35% and over 75% [11, 14, 15].
According to the importance of the subject, this study was designed and accomplished to analyze the association of relationship between ICU admission criteria and end results of caring of obstetrics/gynecologic patients hospitalized in Imam Ali hospital in Zahedan city on 2015.
2. Methods
Ethical approval was provided by ethical committee of Imam Ali hospital, Zahedan city, Iran. In this study, 86 OB/GYN patients hospitalized in ICU of Imam Ali hospital of Zahedan University of medical sciences were studied through studying their files. APACHE II score was quantified after considering the associated parameters during first 24 hours of the hospitalization.
Data was gathered through a questionnaire which was designed based on APACHE II scoring system. Patient’s final fate, duration of hospitalization, necessity of ventilation, the time spent on ventilator and their relationship with APACHE II scoring system were studied. At the end, the data was used by SPPS ver.20 software and the different aspects of the data were compared to each other via t-test and Chi-square.
3. Results
Average age of cases was 27.3+/-5.3 years. Average APACHE.II score was 11.3+/-4.7. Risk of death in 75 cases was 10%, in case of nine patients it was 15%, for one patient that was 35% and one patient had more than 75% risk of death, morality rate was 2.3% (Table 1).
Mean APACHE.II score for the deceased was 32+/-4.2 and in case of the living ones it was 10.8+/-3.5. Because of low mortality rate, Mann-Whitney U test was applied. Results revealed a meaningful relationship between APACHE.II criteria and mortality rate (P = 0.001) (Table 2).
| Variable | Abundance | Apache.Ii Score | P Value |
|---|---|---|---|
| Mortality of patients | |||
| Deceased | 2 | 32+/-4.2 | 0.001 |
| Alive | 85 | 10.8+/-3.5 | |
| Ventilator requirement | |||
| Requried | 25 | 14.7+/-6.1 | 0.001 |
| Not required | 61 | 9.9+/-3.1 |
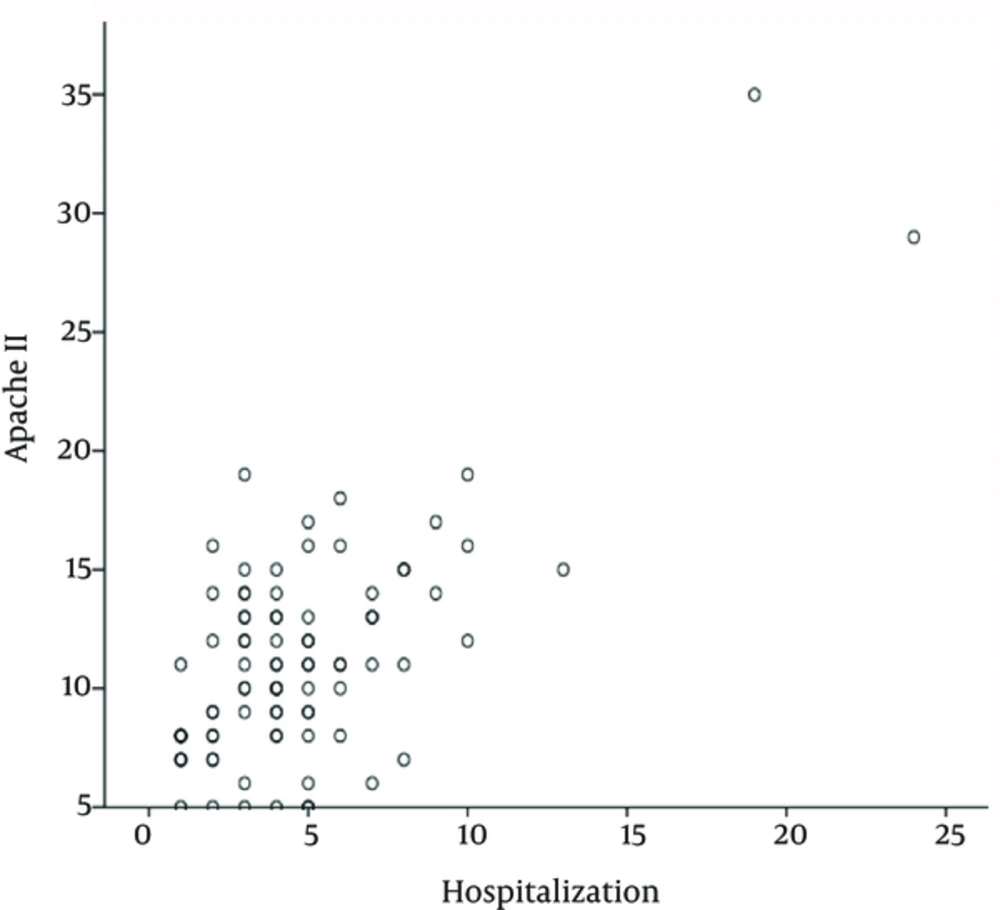
The relationship between APACHE II scoring system and the duration of hospitalization were studied, then the Pearson score was 0.693 which indicated a meaningful relationship (P = 09.00).
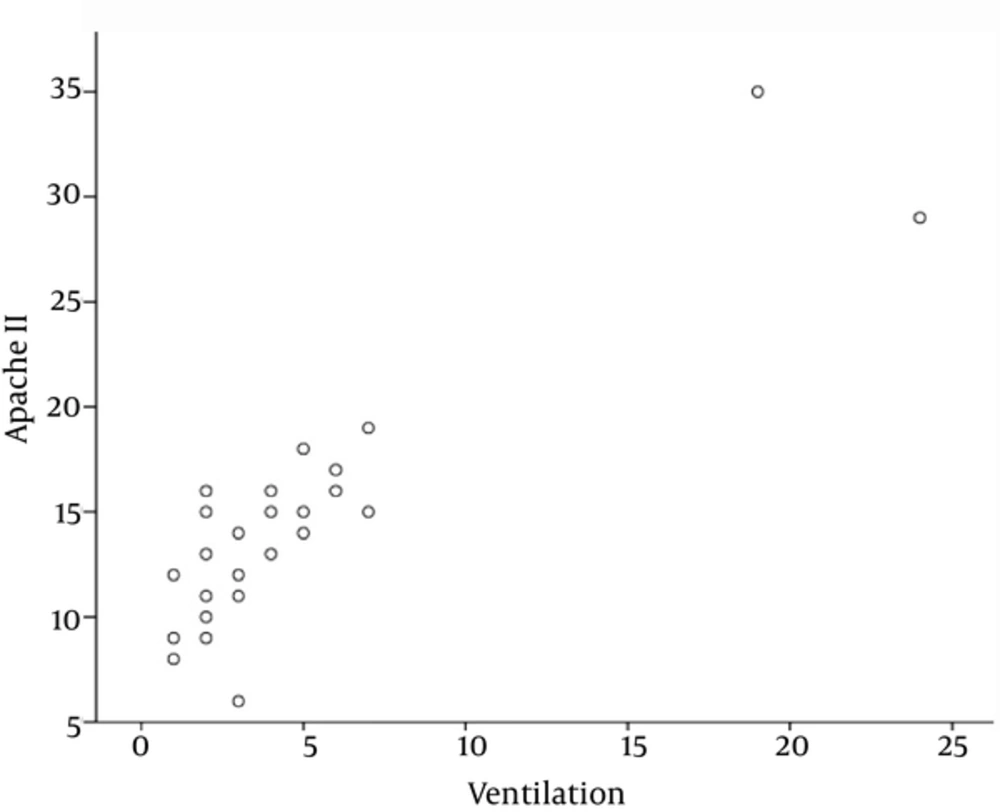
APACHE II score in case of patients in need of ventilation was 14.7+/-6.1, and for those who did not require ventilation it was 9.9+/-3.1, which reveals a meaningful relationship between the scoring system and the need for ventilation (P = 0.00).
Then the relationship between APACHE II scoring system and time spent on the ventilator was studied, the results were the following: Pearson score was 0.888, P value = 0.00, according to the findings mentioned above there is a statistically meaningful relationship between APACHE II scoring system and the time spent on ventilation.
4. Discussion
The study revealed that the mean APACHE II score was 11.3 and the risk of death was associated with more than 87% of patients was less than 10% , only two patients had a high risk of death, which eventually died.
APACHE II score associated with the deceased, requirement of ventilator, longer hospitalization duration, and longer time spent on ventilator was higher meaningfully.
Pollock et al. studied 33 women hospitalized in ICU in Australia on 2011, the mean APACHE II score was 12.6 which had a meaningful statistical association with risk of death and severity of disease comparing to women hospitalized in the OB/GYN ward [16].
Wang et al. studied 101 women hospitalized in ICU in China on 2013, according to APACHE II scores, 12.9% of women were severely ill but only 2.3% of the cases studied in our research were severely ill with high risk of death. Average of duration of hospitalization in Wang et al. study was 7.5+/-3.6 days comparing to the4.7+/-3.6 days of our study is considerably more. Comparing these two studies indicates that the higher APACHE.II score the higher the duration of hospitalization [6].
Lin et al. studied 207 ICU patients on 2011. There was a high incidence of severely ill women with high APACHE II scores. Shortening of the time elapsed from initiation of acute and critical condition to start point of the hospitalization leaded to increment of the remission probability and decline of the hospitalization duration [17].
Zhang et al. compared the end results of APACHE II system and other disease-severity classifications the study revealed that APACHE II is a very practical approach and classification which helps a lot [18]. Amini et al. compared the ability of APACHE II modified APACHE II and TRISS to evaluate and assess the death risk of ICU patients with head trauma on 2010. The results demonstrated that all three of them are able to estimate the death risk equally [19]. Musavi et al. studied trauma cases hospitalized in ICU, according to their results 6 of 75 patients with APACHE II score under 15 died comparing to 12 deaths associated with 20 cases with APACHE II scores between 20 and 30, their study concludes that applying APACHE II scoring system to trauma cases hospitalized in ICU is reasonable and of course patients with high score has to be taken more seriously [20].