1. Background
The Body mass index (BMI), as was introduced in 1842 by Adolphus Quetelet [1], employs a relatively simple formula to describe body condition. For the past 30 years, it has been used as an indicator of body condition and regarded as a measurement of overall obesity in adolescents [1-4]. Another indicator for evaluating body condition is the waist-to-hip ratio (WHR), which represents both the subcutaneous and intra-abdominal adipose tissues [5, 6]. The WHR can be adjusted by gender but the interpretation of the BMI remains the same regardless of gender, age, and ethnicity [7]. In some studies, both the WHR and BMI are shown as valid indicators of obesity, and there are studies which suggest the opposite [4, 8-10]. Both are inexpensive, quick, and developed on the basis of data obtained from people whose origin is either North America or Europe, suggesting that they may not be appropriate for other ethnic groups [11-13].
In Asia, Deurenberg [14] and Huxley [15] estimated the WHR cutoff points of 0.90 for men and 0.80 for women. However, in Obesity in Asia Study [16], the estimated values were 0.92 for men and 0.84 for women. Lin et al. studied 55,563 Taiwanese and reported the WHR cutoff points of 0.85 for men and 0.76 for women [17]. The BMI and WHR indices are reported in Iranian studies. For example, Gharipour [18] reported the WHR cutoff points of 0.88 and 0.93, and the BMI scores of 28.50 and 26.00 for females and males, respectively. Hajian et al. [19] reported the WHR of 0.86 and 0.85, and the BMI of 25.30 and 25.40 for females and males, respectively. Esmaillzadeh found that the WHR was better in detecting obesity than was the BMI [20]. On the other hand, Ejtahed et al. [21] analyzed the data from 133 Iranians and concluded that the BMI is better than is the WHR in diagnosing excess adiposity. Estimating the percentage of body fat (PBF) is a new method for detecting obesity. The world health organization (WHO) defines the gold standards for obesity as the PBF > 25% in men and > 35% in women [22]. The PBF is measured by differences methods such as magnetic resonance imaging (MRI), X-ray, and bioelectrical impedance analysis (BIA) [23]. The BIA is an affordable, non-invasive method [24]. The comparison between the BIA and X-ray has shown that it is accurate in assessing body composition [25-28].
2. Objectives
The primary purpose of this study was to examine the agreement between the BMI and WHR classifications in diagnosing obesity among adult Iranians by using cutoff points of WHO gold standards. The secondary purpose was to estimate suitable cutoff points for BMI and WHR for various sex and age-groups.
3. Methods
The study was cross-sectional in nature. The permission to conduct it was obtained from the vice chancellor for research and technology at Hormozgan University of Medical Sciences. The prevalence of obesity in Iranian adult population is 21.5% [29], which was used to estimate that the minimum sample size was 6,483 at the 0.01 level of significance. The data collection took place between 2009 and 2014 in a health and diet therapy center in Bandar Abbas, Iran. There were 23,300 individuals who voluntarily agreed to participate in the study. All signed the required consent forms. The data collection and the implementation of the BIA were explained to all participants by the members of the research team. Those who were not at least 20 years old, had pacemakers, were pregnant, and had been hospitalized three months prior to data collection were excluded from the study. There were 19,366 adults (13,691 females, 5,675 males) who met the inclusion criteria. Although there were many more females than males in the study, it must be noted that the BMI does not take into consideration gender differences and that the WHR indices were calculated for different genders separately.
The BIA was performed, using the body composition analysis device - Plusavis 333 (JAWON medical company). This device uses the frequency ranging from 50 kHz to 250 kHz and utilizes the latest technology to measure body composition, using direct segmental multi-frequency. The device can be used to measure the BMI, WHR, PBF, total body fat, proteins, minerals, soft lean mass, fat free mass, muscle quantity, lean body mass, total body water, total energy expenditure, basal metabolic rate, fat-trunk, and muscle-trunk. The whole body impedance was measured by using the standard positions of outer and inner electrodes on the right hand and foot (8 electrodes) [30]. The measurements were done by professional technicians. Body height in centimeter (cm) was measured to the nearest 0.5 cm by stadiometer. The BMI was calculated by dividing weight in kilogram (kg) by squared height (cm) and used to form four groups: 1, underweight (under 18.50); 2, normal weight (18.50 to 24.99); 3, overweight (25.00 to 29.99), and; 4, obese (30.00 and higher) [31]. The WHR was classified for men as < 0.90 (normal), 0.90 - 0.99 (overweight), and ≥ 1 (obese); for women < 0.80 (normal), 0.80 - 0.84 (0verweight), and ≥ 0.85 (obese) [32]. We used the WHO gold standards to evaluate the accuracy of the BMI and WHR in detecting obesity. The cutoff points of the gold standards were used to identify the obese persons. To do so, we divided all subjects into either non-obese or obese based on the BMI and WHR. Three age-groups were formed: 20 - 39, 40 - 59, and greater than 59 years old. The statistical package for the social sciences (SPSS) was used for the purpose of data analysis. Contingency tabulations were used to calculate sensitivity, specificity, positive predictive power (PPV), and negative predictive power (NPV). Group comparisons employed t-test for independent samples. Additionally, receiver-operating characteristic (ROC) curves [33], Fisher’s r-to-z transformation, linear regression, and Hanely formula [34] (for comparing ROC curves) were employed. The level of significance was set, a priori, at 0.01.
4. Results
A profile of subjects is shown in Table 1. Gender differences on the basis of the BMI and fat free mass (FFM) were not statistically significant, suggesting that these two parameters do not differentiate between females and males. On the other hand, the WHR, height, weight, and soft lean mass (SLM) were less and the PBF and total fat (TF) were more in females compared to males and the differences were statistically significant. On the basis of the gold standards, the BMI, and the WHR, 52.1%, 35.8%, and 34.8% of the study participants were obese respectively.
| Subjects | N | Mean | SD | P |
|---|---|---|---|---|
| Age | < 0.01 | |||
| Female | 13691 | 34.17 | 10.40 | |
| Male | 5675 | 34.81 | 10.74 | |
| Height | < 0.01 | |||
| Female | 13691 | 159.73 | 5.90 | |
| Male | 5675 | 173.99 | 6.65 | |
| Weight | < 0.01 | |||
| Female | 13691 | 71.46 | 17.00 | |
| Male | 5675 | 84.64 | 20.92 | |
| BMI | 0.29 | |||
| Female | 13691 | 28.01 | 6.49 | |
| Male | 5675 | 27.90 | 6.48 | |
| PBF | < 0.01 | |||
| Female | 13691 | 33.56 | 7.70 | |
| Male | 5675 | 24.32 | 8.343 | |
| WHR | < 0.01 | |||
| Female | 13691 | 0.84 | 0.08 | |
| Male | 5675 | 0.88 | 0.10 | |
| FFM | 0.27 | |||
| Female | 13691 | 9.07 | 9.08 | |
| Male | 5675 | 9.2 | 10.4 | |
| TF | < 0.01 | |||
| Female | 13691 | 25.10 | 10.31 | |
| Male | 5675 | 21.94 | 11.33 | |
| SLM | < 0.01 | |||
| Female | 13691 | 42.32 | 6.38 | |
| Male | 5675 | 57.84 | 9.96 |
Abbreviations: BMI, body mass index; PBF, percent body fat; WHR, waist-to-hip ratio; FFM, fat free mass; TF, total fat; SLM, soft lean mass.
4.1. WHR in Males
There were 679 males (12% of all) who were classified as obese. Sensitivity and the NPV were 21.6% and 50.7%, respectively. On the basis of this classification, nearly 78% of obese subjects had been wrongly classified as non-obese.
4.2. WHR in Males by AGE-Group
The WHR was ineffective in detecting obesity among males between 20 and 39 years old. The sensitivity and NPV in this group were 10.9% and 49.8%, respectively. The sensitivity ranged from 10.9% to 70.1% among males. Results showed that increase in age was associated with increase in detecting obesity in males. Specificity and PPV for all age-groups were 100%. The suitable cutoff point for the 20 - 39 age-groups was 0.85, 0.93 for the 40 - 59 age-groups, and 0.96 for males older than 59 years.
4.3. BMI in Males
There were 1,969 males (34.7% of all males) who were classified as obese. Sensitivity and PPV were 57.5% and 64%, respectively. Results showed that 42.5% of obese males had been wrongly classified as non-obese.
4.4. BMI in Males by Age-Group
The BMI was effective in detecting obesity among males ranging in age from 20 to 39 years. The sensitivity and NPV were 61.7% and 68.5%, respectively. For all males, sensitivity ranged from 46.7% to 61.7%. Results showed that increase in age was associated with decrease in detecting obesity in males. More than half of the obese males were wrongly classified as non-obese after the age of 39 years. The suitable cutoff points for the 20 - 39, 40 - 59, and greater than 59 years age-groups were 27.4, 27.5, and 26.4, respectively.
4.5. WHR in Females
There were 6,063 females (44.3% of all females) who were classified as obese. The measures of sensitivity, specificity, PPV, and NPV were high. Only 15.8% of obese females were wrongly classified as non-obese.
4.6. WHR in Females by Age-Group
The WHR was effective in detecting obesity in older than 39 years females. Increase in age was associated with increase in detecting obesity in females. The suitable cutoff points were 0.82, 0.85, and 0.86 for the 20 - 39, 40 - 59, and greater than 59 years’ age-groups.
4.7. BMI in Females
There were 4,963 females (36.3% of all females) who were classified as obese. Sensitivity and NPV were 68.8% and 75.1%, respectively. By this method, 31.2% of obese females were wrongly classified as non-obese. The BMI was effective in detecting obesity among females. Increase in age was associated with decrease in sensitivity and NPV.
4.8. BMI in Females by Age-Group
The BMI was effective in detecting obesity in females between the ages of 20 and 39 years in which sensitivity and NPV were 69.5% and 80%, respectively. Among those older than 59 years, sensitivity and NPV were 66% and 52.5%, respectively. In this age-group, the BMI was not useful in distinguishing between female and male subjects. The suitable cutoff points for the 20 - 39, 40 - 59, and greater than 59 years age-groups were 27.8, 28.0, and 26.9, respectively (Table 2).
| Age-Group | Non-Obese, N | Obese, N | Sensitivity, % | Specificity, % | PPV, No. (%) | NPV, No. (%) | ||
|---|---|---|---|---|---|---|---|---|
| BMI: Total Male (M) | 3706 | 1969 | 57.5 | 93.6 | 1807 | (91.8) | 2372 | (64) |
| BMI: 20-39 (M) | 2626 | 1437 | 61.7 | 94.3 | 1329 | (92.5) | 1800 | (68.5) |
| BMI: 40-59 (M) | 963 | 476 | 48.7 | 91.4 | 428 | (89.9) | 512 | (53.2) |
| BMI: > 59 (M) | 117 | 56 | 46.7 | 90.9 | 50 | (89.3) | 60 | (51.3) |
| WHR: Total Male (M) | 4996 | 679 | 21.6 | 100.0 | 679 | (100.0) | 2534 | (50.7) |
| WHR: 20-39 (M) | 3829 | 234 | 10.9 | 100.0 | 234 | (100.0) | 1908 | (49.8) |
| WHR: 40-59 (M) | 1069 | 370 | 42.1 | 100.0 | 370 | (100.0) | 560 | (52.4) |
| WHR: > 59 (M) | 98 | 75 | 70.1 | 100.0 | 75 | (100.0) | 66 | (67.3) |
| BMI: Total Female (F) | 8728 | 4963 | 68.8 | 97.3 | 4782 | (96.4) | 6557 | (75.1) |
| BMI: 20-39 (F) | 6809 | 3218 | 69.5 | 98 | 3106 | (96.5) | 5448 | (80) |
| BMI: 40-59 (F) | 1778 | 1612 | 67.5 | 94 | 1546 | (95.9) | 1035 | (58.2) |
| BMI: > 59 (F) | 141 | 133 | 66 | 96.1 | 130 | (97.7) | 74 | (52.5) |
| WHR: Total Female (F) | 7628 | 6063 | 84.2 | 96.9 | 5853 | (96.5) | 6528 | (85.6) |
| WHR: 20-39 (F) | 6648 | 3379 | 75.6 | 100.0 | 3379 | (100) | 5560 | (83.6) |
| WHR: 40-59 (F) | 938 | 2452 | 99.5 | 84.1 | 2277 | (92.9) | 926 | (98.7) |
| WHR: > 59 (F) | 42 | 232 | 100 | 54.4 | 197 | (84.9) | 42 | (100) |
Abbreviation: BMI, body mass index; WHR, waist-to-hip ratio.
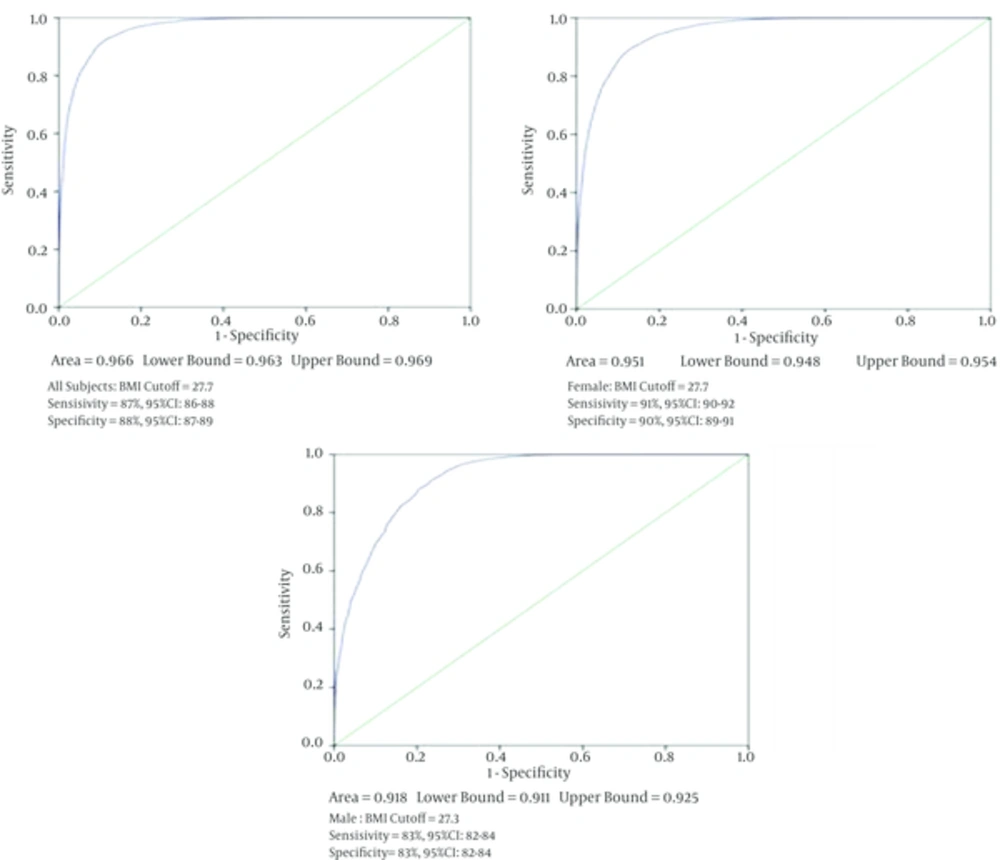
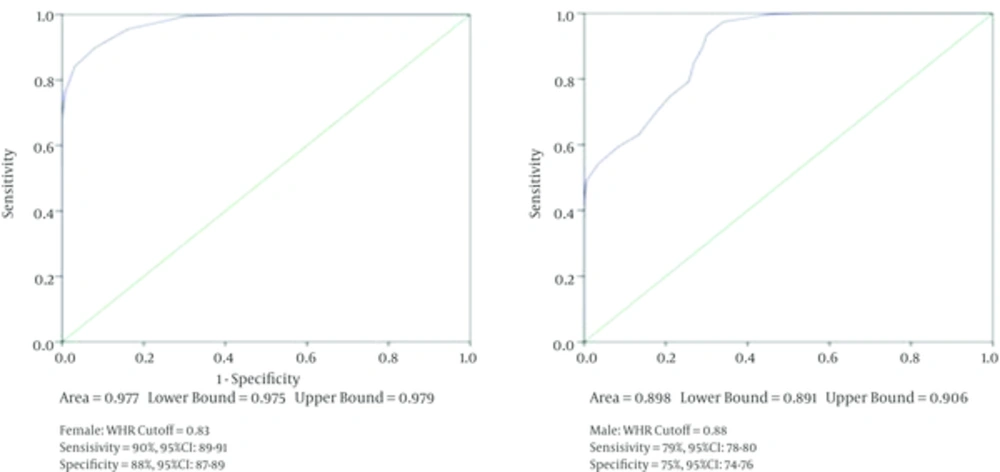
4.9. ROC Curves Analysis
The ROC curve analysis showed that a suitable BMI cutoff point for detecting obesity was 27.7 in all subjects, 27.7 in females, and 27.3 in males. Additionally, on the basis of the WHR, the suitable cutoff points were 0.83 and 0.88 for females and males, respectively. Results are depicted in Figures 1 and 2.
4.10. Correlational Analyses
A detailed correlational analysis was performed. Fisher’s r-to-z transformation was used to examine the statistical significance of the differences between magnitudes of the simple associations.
Simple correlations between the PBF on one hand and the BMI and WHR on the other hand are summarized in Table 3. In relation to the BMI, the largest correlation coefficients belonged to the 20 - 39 age-group, which was significantly higher than the other age-groups (P < 0.01). In all age-groups, the associations were significantly higher among the females compared to the males (P < 0.01). In relation to the WHR, the magnitude of the associations was higher and accounted for larger amount of the explained variation in the PBF than the ones obtained for the BMI (P < 0.01). Simple correlations between the TF on one hand and the BMI and WHR on the other hand showed that the magnitude of all associations was high, ranging from 0.86 to 0.98. The BMI showed stronger associations with the TF than did the WHR and all differences were statistically significant (P < 0.01). Simple correlations between the SLM on one hand and the BMI and WHR showed that the range of the associations between the BMI and SLM was from 0.71 to 0.84 while it was from 0.24 to 0.72 for the WHR. The most pronounced trend was a decrease in the magnitude of the association as age increased. Results are summarized in Table 3.
| Age- Group | BMI and PBF | WHR and PBF | BMI and TF | WHR and TF | BMI and SLM | WHR and SLM |
|---|---|---|---|---|---|---|
| Female | ||||||
| 20 - 39 | 0.92 | 0.97 | 0.98 | 0.94 | 0.84 | 0.72 |
| 40 - 59 | 0.86 | 0.97 | 0.96 | 0.89 | 0.75 | 0.45 |
| > 59 | 0.86 | 0.98 | 0.95 | 0.88 | 0.71 | 0.38 |
| Male | ||||||
| 20 - 39 | 0.88 | 0.96 | 0.97 | 0.90 | 0.82 | 0.54 |
| 40 - 59 | 0.74 | 0.97 | 0.92 | 0.86 | 0.75 | 0.24 |
| > 59 | 0.76 | 0.98 | 0.93 | 0.91 | 0.74 | 0.27 |
Abbreviations: BMI, body mass index; WHR, waist-to-hip ratio; PBF, percentage of body fat; TF, Total fat; SLM, soft lean mass.
5. Discussion
The aim of the study was to determine suitable BMI and WHR cutoff points for detecting obesity among adult Iranians. Based on this study, a suitable cutoff point for BMI is 27.7, which is smaller than the WHO’s 30. By the BMI classification, 42% and 32% of the obese males and females, respectively, were classified as non-obese. After the age of 39 years, this classification missed half of the obese men and one third of the obese women. Romero et al. reported that the BMI missed more than half of the obese subjects. These findings indicate that the BMI has limited diagnosis performance in detecting obesity, especially in men and elderly. We suggest 26.4 and 26.9 as cutoff points for detecting obesity in elderly males and females, respectively.
The suitable WHR cutoff point for Iranian males is 0.88, which is less than the suggested cutoff point of 0.95 for males in American [35], ≥ 1 for European males 32, and Arabian studies such as Al-Lawati et al. [36] (0.91) and Mansour et al. [37] (0.92). However, it is fairly close to the ones reported in Eastern Asian studies, for example, Lin et al. [38] (0.85 - 0.88) and Ko et al. [39] (0.88). The suitable WHR cutoff point for Iranian females is 0.83, which is more than the ones recommended for Americans (0.80), less than Omanis (0.91), and Iraqis (0.91) but similar to those reported for Europeans (≥ 0.85) and Eastern Asians (0.84). The WHR is limited in diagnosing obesity in young males but is powerful in distinguishing between non-obese and obese females. For example, it correctly classified more than 99.5% of obese females after the age of 39 years.
Gharipour et al. reported 0.95 as the suitable WHR cutoff point for elderly Iranian males. On the basis of our data, our estimate of the index is 0.96. These findings suggest that the WHR cutoff point to detect obesity among elderly males in Iran is less than the one for the Europeans (≥ 1). In males with age less than 60, the BMI is more effectiveness than is the WHR in classifying non-obese and obese subjects.
The sensitivity, specificity, NPV, and PPV, based on the WHR, were high among females, attesting to usefulness of the WHR in detecting obesity in females with the exception of those older than 59 years in which half were wrongly classified of being obese. The WHR’s specificity for men in all age groups was 100%, indicating that it could correctly classify obese males. Both the BMI and WHR were highly correlated with the TF and PBF. In the WHR, increase in age was associated with increase in sensitivity, NPV, and SLM, regardless of gender. In the BMI, increase in age in males and females was associated with decrease in the NPV and SLM. These results suggest that strong correlations are not necessarily indicators of proper diagnostic performance, for which there is some support in the literature [40].
The BMI correctly classified 30% - 36% and 28% - 58% of overweight men and women, respectively. Peltz et al. concluded that the discrepancies between the BMI and PBF were due to the BMI’s limitations [41]. There are criticisms associated with the BMI [42], including its frequent misclassification [43], high rate of false negatives, and that it cannot be in a standard form.
In spite of the large sample, it should be noted that the study’s participants were recruited from south Iran and did not represent the country’s population. We recommend the replication of the study in other regions of Iran, which could enhance the generalizability of the results.
We conclude that 1, the WHR is limited in detecting obesity in men under 60 years old; and 2, the BMI faces limitations in distinguishing between overweight and obese men and women. Additionally, we report that both the WHR and BMI underestimate the number of subjects who meet the criteria for obesity. It seems that the WHR is suitable for distinguishing between obese and overweight females, and that as age increases, the WHR is better than is the BMI in classifying both males and females.
Age, gender, and race for BMI, and age and race for WHR and Gold Standard have not been considered in formulation of these classifications. It is essential to find a standard method for assessing with confidence body conditions based on sex and age groups, [44, 45].