1. Background
There are controversies regarding the diagnosis of lupus nephritis because its clinical manifestations and severity are different from one patient to another. Without accurate monitoring, lupus nephritis can lead to end-stage renal disease (ESRD). Therefore, it is necessary to find a non-invasive method for the diagnosis and monitoring of lupus nephritis. Serum creatinine levels, urine protein, and urine sediments level (RBC cast) can be used to evaluate the response to the treatment. In addition, the size of the autoantibodies is useful to detect lupus nephritis and disease activity monitoring (1-5). As the severity of lupus nephritis is associated with its clinical manifestations and histopathology, biopsy and histopathology can be considered as the gold standard for its diagnosis. A biopsy is an invasive method with complications such as bleeding, intravenous artery fistula, and infection. Although it provides useful clinical and laboratory findings, its repetition is difficult and is not accessible at all healthcare centers (3-7).
According to the currently available evidence, the use of clinical and laboratory findings can be considered as the gold standard for early diagnosis of lupus nephritis, which is a non-invasive, low cost, and easy to use method (5-7). Our literature review revealed that few quantitative biopsy-related criteria have been compared in terms of the degree of kidney involvement. There are also other important criteria, such as clinical and laboratory criteria, that their association with renal involvement in biopsy have not been studied.
2. Objectives
In this study, in addition to a wider comparison of clinical and laboratory symptoms with the degree of kidney involvement, the diagnostic value of laboratory and clinical findings of patients with lupus nephritis based on the findings of the biopsy was investigated.
3. Methods
Following a retrospective design, patients with lupus who were candidates for renal biopsy and undergoing kidney biopsy were studied. A total of 57 patients were referred to the nephrology Department of the Imam Khomeini Hospital. The biopsy of 26 cases (out of 57) was excluded due to various reasons, mainly because of patients’ dissatisfaction and medical considerations. Out of 31 eligible biopsies, one was diagnosed with diabetic nephropathy. Finally, a total of 30 cases were investigated.
Data on clinical findings (including blood pressure, limb edema) and laboratory hemorrhage (Cr, ESR, CRP, BUN, C3, C4, CH50, Anti-ds DNA, and hematuria) were collected. Finally, the diagnostic value of clinical and laboratory findings was evaluated according to the pathology staging of samples. Bun, Cr, c3, c4, and CRP were measured by Hitachi.917, and Anti ds-DNA was measured by the chemiluminescence method. Hematuria was evaluated using the tetramethylbenzidine dipstick and microscopic method. Biopsy was performed using a frozen section, and H&E was applied for the staging of nephritis.
3.1. Data Analysis
Data analysis was administered using SPSS. Descriptive statistics such as frequency, percent, tables, and bar diagrams were used to describe the findings. Quantitative variables are displayed using mean (and standard deviation) and quartiles. The Kolmogorov-Smirnov test was applied to test for a normal distribution. Based on the biopsy results, there was no report of mild kidney involvement (i.e., stages 1 and 2). Patients were divided into two groups of severe and end-stage. Fisher’s exact test was used to compare study groups. Also, independent samples t-test and Levene’s test were used to evaluate variances of quantitative variables. Error bars were also used to compare the quantitative variables of study groups.
4. Results
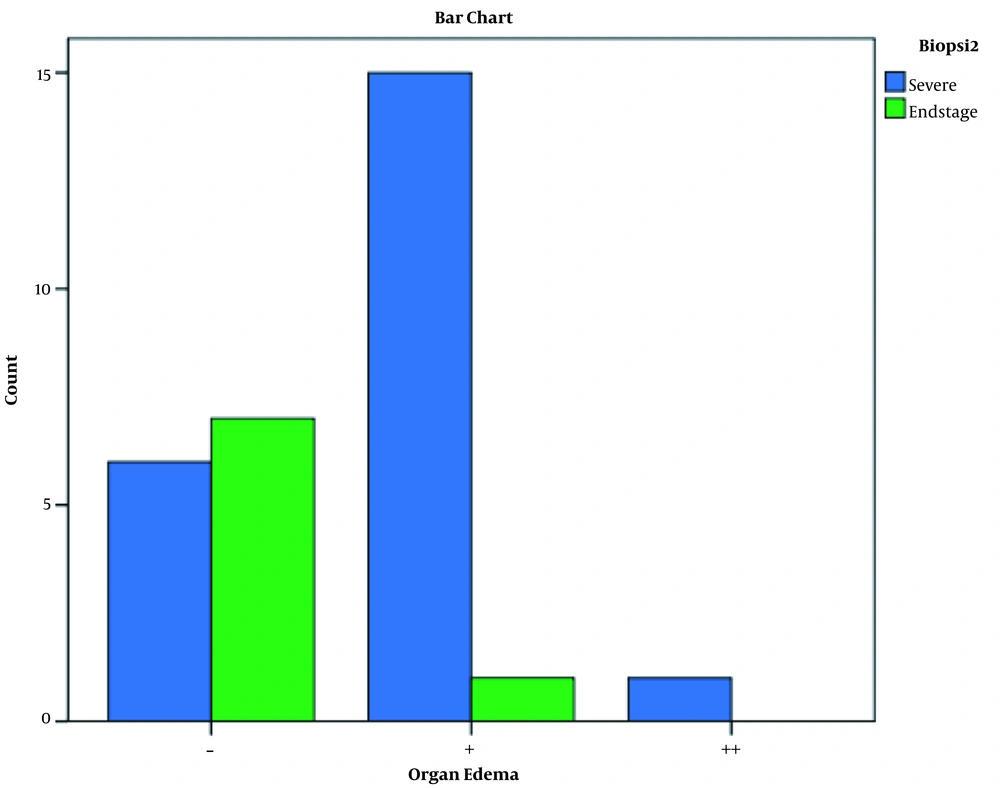
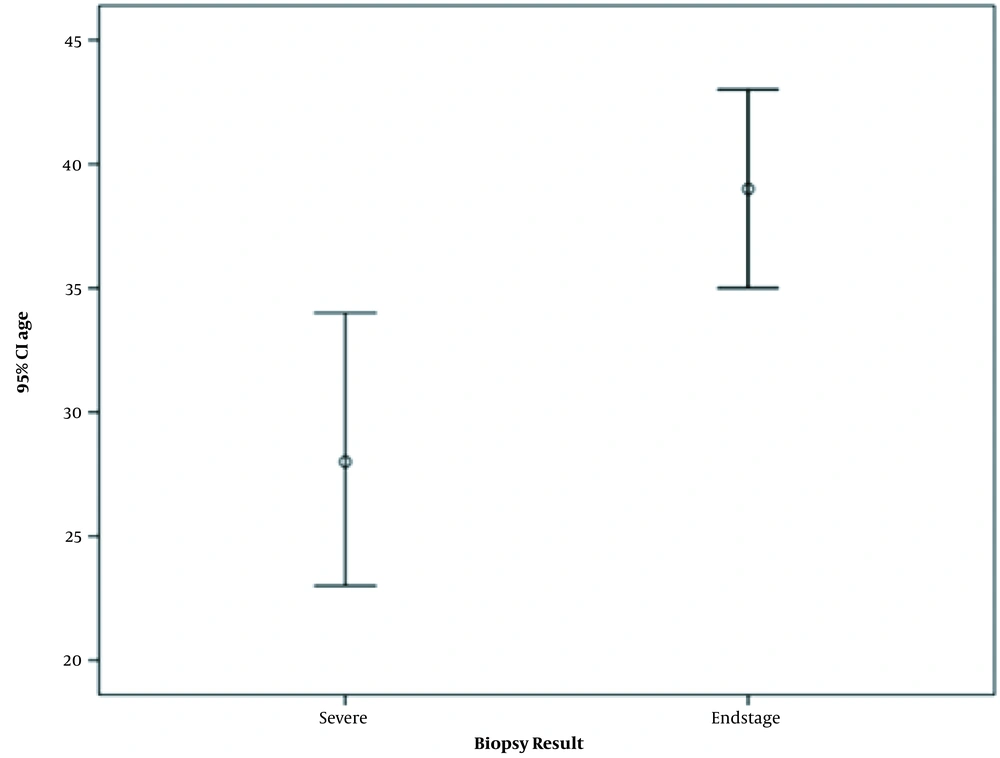
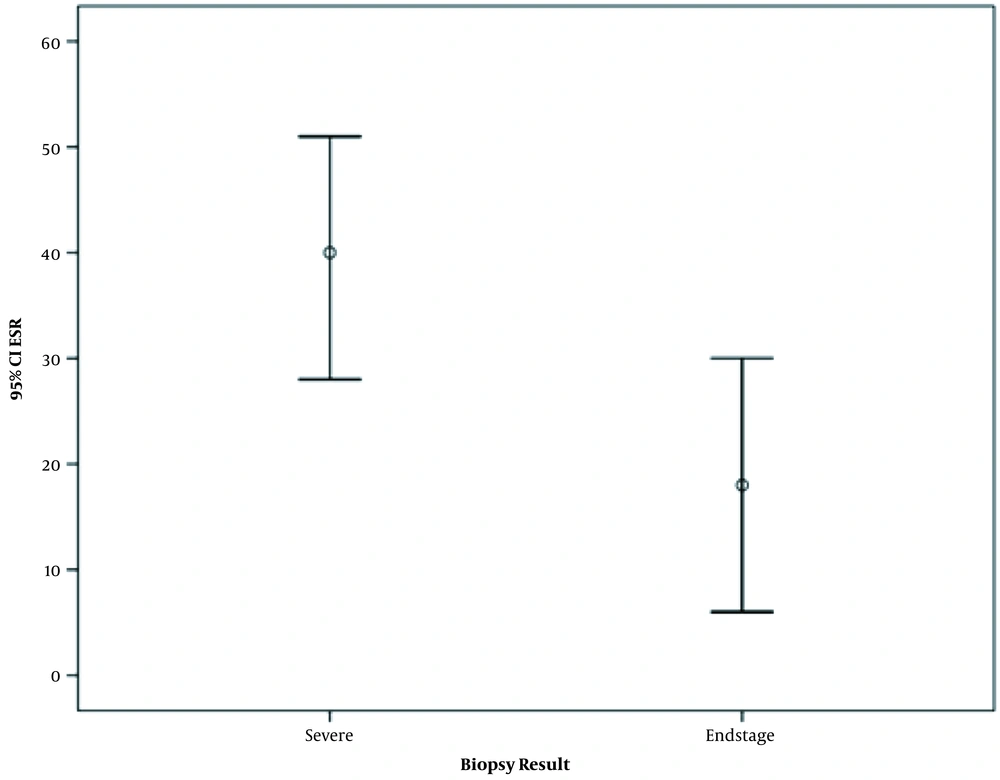
In this study, a total of 57 patients were referred to the Nephrology Department of the Imam Khomeini Hospital. The biopsy of 26 cases (out of 57) was excluded due to various reasons, mainly because of patients’ dissatisfaction and medical considerations. One (out of 31) biopsy was diagnosed with diabetic nephropathy. Eventually, the biopsy of 30 patients was investigated. Five cases had a biopsy of grade 3 and FSGN, 8 had grade 3 - 4, 9 had grade 4, 8 had grades of 4 - 5, 5 and 5 - 6 (Table 1). Based on the results of the biopsy, there was no report of mild kidney involvement (i.e., stages 1 and 2). Patients were divided into two groups of severe (grades 3, 3 - 4 and 4) and end-stage (grades 4 - 5, 5 and 5 - 6) (Tables 2 and 3). According to the findings, the significant items included age, limb edema, and ESR. In the severe group, patients were younger but had higher ESR and limb edema. But in the end-stage group, the opposite was seen (that is, patients were older, had lower ESR, and extremity of edema was lower. Proteinuria, complement, and anti-ds DNA were not significantly different between the two groups. Variables of age, limb edema, and ESR had a significant association with biopsy results (P < 0.05) (Figure 1-3).
| Grading | No. (%) |
|---|---|
| 3 class | 3 (10.0) |
| 4 class | 9 (30.0) |
| 5 class | 6 (20.0) |
| FSGN | 2 (6.7) |
| 3-4 class | 8 (26.7) |
| 4-5 class | 1 (3.3) |
| 5-6 class | 1 (3.3) |
| Total | 30 (100.0) |
Grading of the Biopsy Results for 30 Patients
| Variables | Biopsy Groups | Total | P-Value | |
|---|---|---|---|---|
| Severe | End Stage | |||
| Sex | 1.0 | |||
| Female | 21 (95.5) | 8 (100.0) | 29 (96.7) | |
| Male | 1 (4.5) | 0 (0.0) | 1 (3.3) | |
| Organ edema | * | |||
| - | 6 (27.3) | 7 (87.5) | 13 (43.3) | |
| + | 15 (68.2) | 1 (12.5) | 16 (53.3) | |
| ++ | 1 (4.5) | 0 (0.0) | 1 (3.3) | |
| Hemachori | * | |||
| - | 4 (18.2) | 2 (25.0) | 6 (20.0) | |
| + | 16 (72.7) | 6 (75.0) | 22 (73.3) | |
| ++ | 2 (9.1) | 0 (0.0) | 2 (6.7) | |
| Lechositori | 0.698 | |||
| - | 9 (40.9) | 4 (50.0) | 13 (43.3) | |
| + | 13 (59.1) | 4 (50.0) | 17 (56.7) | |
| CH50 | 0.419 | |||
| Decrease | 10 (45.5) | 2 (25.0) | 12 (40.0) | |
| Normal | 12 (54.5) | 6 (75.0) | 18 (60.0) | |
| C3 | 0.112 | |||
| Decrease | 19 (90.5) | 5 (62.5) | 24 (82.8) | |
| Normal | 2 (9.5) | 3 (37.5) | 5 (17.2) | |
| C4 | 0.112 | |||
| Decrease | 19 (90.5) | 5 (62.5) | 24 (82.8) | |
| Normal | 2 (9.5) | 3 (37.5) | 5 (17.2) | |
| Total | 21 (100.0) | 8 (100.0) | 29 (100.0) | |
| Variables | Biopsy Group | Frequency | Mean ± SD | P-Value |
|---|---|---|---|---|
| Age | Severe | 22 | 28.91 ± 12.486 | 0.031 |
| End stage | 8 | 39.25 ± 4.652 | ||
| Start of entanglement, y | Severe | 21 | 4.381 ± 4.5219 | 0.527 |
| End stage | 8 | 5.750 ± 6.5846 | ||
| Proteinuria rate | Severe | 22 | 2521.59 ± 1937.988 | 0.913 |
| End stage | 8 | 2604.25 ± 1343.661 | ||
| Creatinine | Severe | 22 | 1.364 ± 0.7000 | 0.410 |
| End stage | 8 | 1.138 ± 0.4984 | ||
| Systolic BP | Severe | 22 | 138.18 ± 18.162 | 0.456 |
| End stage | 8 | 132.50 ± 18.323 | ||
| Diastolic BP | Severe | 22 | 85.00 ± 9.636 | 0.770 |
| End stage | 8 | 86.25 ± 11.877 | ||
| ESR | Severe | 22 | 40.18 ± 25.828 | 0.034 |
| End stage | 8 | 18.62 ± 13.938 | ||
| CRP | Severe | 22 | 15.39 ± 17.630 | 0.495 |
| End stage | 8 | 10.62 ± 13.384 | ||
| Anti-ds DNA | Severe | 21 | 389.14 ± 261.296 | 0.554 |
| End stage | 8 | 326.25 ± 226.838 | ||
| Hemoglobin | Severe | 22 | 9.550 ± 2.5686 | 0.326 |
| End stage | 8 | 10.550 ± 1.9109 | ||
| WBC, thousand | Severe | 8 | 10.250 ± 4.4320 | 0.663 |
| End stage | 5 | 11.400 ± 4.6152 | ||
| PLt | Severe | 22 | 202.95 ± 70.886 | 0.935 |
| End stage | 8 | 205.38 ± 70.940 | 0.031 |
Comparison of the Grading of the Biopsy Results in 30 Patients According to Quantitative Variables
5. Discussion
Several studies reported a correlation between the findings of the laboratory and the degree of renal involvement in patients with lupus. However, the degree of renal involvement cannot be determined only according to the laboratory criteria. Plawecki et al. (1) investigated the association between lupus nephritis and c1q anti-ficolin-3, anti-ds DNA-antibodies, and complement reduction in patients with abnormal lupus nephritis and other forms of involvement (such as internal organs). They also reported declined levels of active proliferative and creatinine, anti-ds DNA, and Anti-C1q (1).
In a similar study, Zivkovic et al. (2) investigate the positive or negative predictive value of anti-ds DNA -ANA- and anti-c1q for lupus nephritis, which was considered to be a positive predictor of lupus nephritis and potentially helpful in predicting lupus nephritis. Zabaleta-Lanz et al. (3) compared 42 patients with non-asymptomatic renal insufficiency (SLN) and 49 untreated patients with renal failure lupus erytoureasis (OLN). They reported that ANA-anti-ds DNA-Antigen and C4 serum were not significantly different between the study groups. However, serum C3 and CH50 were significantly different (3). In a study on 48 patients with lupus nephritis (who 72% had grades 1 and 2 and 17% in grades 3 to 4 of renal damage according to the results of the biopsy), Ishizaki et al. (4) reported that those with higher grades had a considerably lower level of C3-and CH50. As the level of Anti-sm was significantly higher, it was considered as the predictor of silent lupus nephritis (4). de leeuw et al. (5) intended to measure anti-ds DNA by the ELISA method and reported that 95% of participants were positive for lupus nephritis. In a study on patients referred to a hospital in South India from 2009 to 2014, Devadass et al. (6) investigated patients with SLE with clinical evidence of lupus nephritis. They mentioned grades 3 and 4 as the most common involvements. In addition, the authors found that a higher proportion of ANA and Anti ds positive DNA accompanied with a higher frequency of arthritis at presentation (6). In a study by Farah et al. In 2019 similar to our study in 79 patients with lupus nephritis based on clinical and laboratory findings, in renal biopsy patients, biopsy results showed the highest degree of involvement in stages 4, 3, and 5. On the other hand, renal failure rate and Anti ds DNA level were significantly correlated with grade 4 kidney involvement (7).
In the present study, 30 cases were examined, out of which 5 had a biopsy result of grade 3 and FSGN, 8 had grade of 3 - 4, 9 had grade 4, and 6 had a grade 5 biopsy. The associations between age, limb edema, ESR, and biopsy results were statistically significant. Akbarian et al. (8) investigated the association between isolated hematuria and the results of the biopsy in patients with lupus. In addition, 21.25% of patients had grade 2, 63.15% were of grade 3, and 3 had grade 4 of kidney involvement (8). In our study, the results showed that almost all patients selected for biopsy were correctly identified based on clinical and laboratory findings. The degree of renal involvement in these patients ranged from grade 3 to 5, which indicates the need for prompt treatment. These results confirm the association between clinical and laboratory findings and the degree of renal involvement in biopsy and indicate that the more clinical and laboratory criteria used in patient selection, especially in the first three years of lupus disease, the results will be more reliable.
These results are particularly relevant in healthcare centers where biopsy is not possible, or patients are not satisfied with the biopsy. On the other hand, preparation of biopsy results is usually time-consuming, and patients with lupus kidney disease often require urgent treatment; hence, it seems necessary for physicians to make more reliable clinical and laboratory findings to initiate treatment. The use of clinical and laboratory findings can be highly helpful, mainly due to easy, non-invasive access as well as early preparation of results to determine the severity of the disease in the shortest time.