1. Background
Leishmaniasis is a parasitic infectious disease caused by Leishmania spp. (1). About 70,000 deaths are caused by leishmaniasis every year across the world. Besides, 350 million people are at risk of CL, and around 1.5 - 2 million new cases are reported in the globe annually (2). According to the WHO report, leishmaniasis is one of the six main diseases in tropical regions (3).
Leishmaniasis occurs in three main clinical forms: mucocutaneous leishmaniasis (MCL), visceral leishmaniosis (VL), and cutaneous leishmaniasis (CL) that is the most prevalent type (4). Cutaneous leishmaniasis is a vector-borne skin infection that is still one of the important health problems in the world, especially in tropical and subtropical countries (2, 5, 6). Its incidence is increasing worldwide, and it is considered as one of the most important neglected diseases (2). Cutaneous leishmaniasis causes skin lesions such as papules, nodules, or plaques with a period of six to 12 months (7). Although the disease is self-limited, it leaves scars on the skin, causing mental and psychological complications for the patients (8). Cutaneous leishmaniasis is caused mainly by Leishmania major and Leishmania tropica, which are causative agents for zoonotic cutaneous leishmaniosis (ZCL) and anthroponotic cutaneous leishmaniosis (ACL), respectively (9). Over 90% of CL cases occur in seven countries, including Brazil, Saudi Arabia, Algeria, Afghanistan, Syria, Peru, and Iran (10-14).
Iran is one of the most common endemic diseases for CL. The prevalence of the disease has been reported from 1.8 to 37.9 in different parts of Iran, and 56,546 CL patients were identified in this country from 2011 to 2013 (5, 15). Mashhad is the second-most populous city in Iran and one of the important endemic areas of CL in the country (16-18).
2. Objective
This study aimed to evaluate the status of CL during four years (2015 - 2018) in Mashhad City, Iran.
3. Methods
A retrospective cross-sectional study was conducted to determine the epidemiological status of CL from 2015 to 2018 in Mashhad City. Mashhad is the capital of Khorasan-e-Razavi Province, which is located in the northeastern of Iran. The information of 5,241 confirmed patients who had been referred to five health centers was recorded. We obtained the total population covered by each healthcare center in Mashhad City, so we could calculate the prevalence of CL. Cutaneous leishmaniasis had been diagnosed by lesion sampling, stained smear, and microscopic methods. Data including age, sex, nationality, place of residence, number, and site of wounds on the body were collected and analyzed.
Data were analyzed by SPSS 16 software. The chi-square and Fisher exact tests were conducted at the significance level of less than 0.05 to examine the statistical differences between subgroups of patients.
4. Results
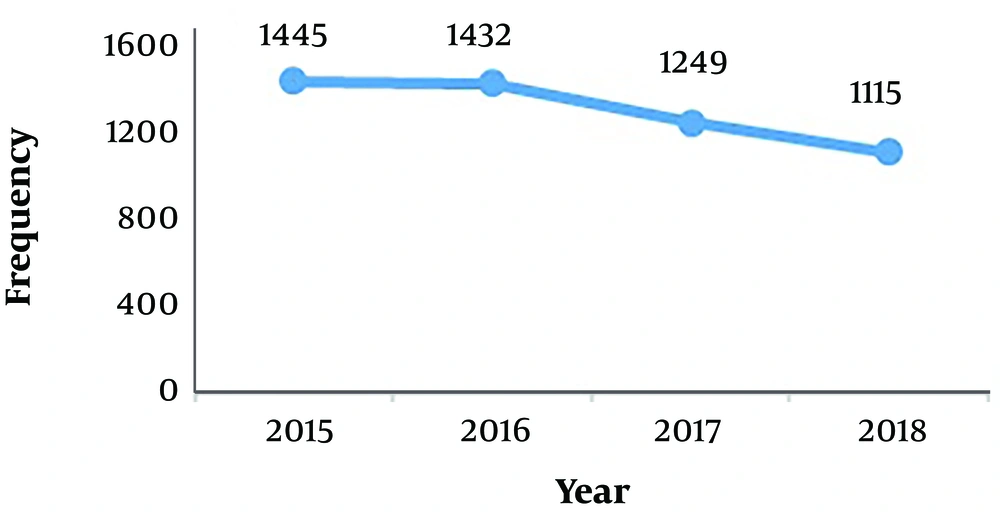
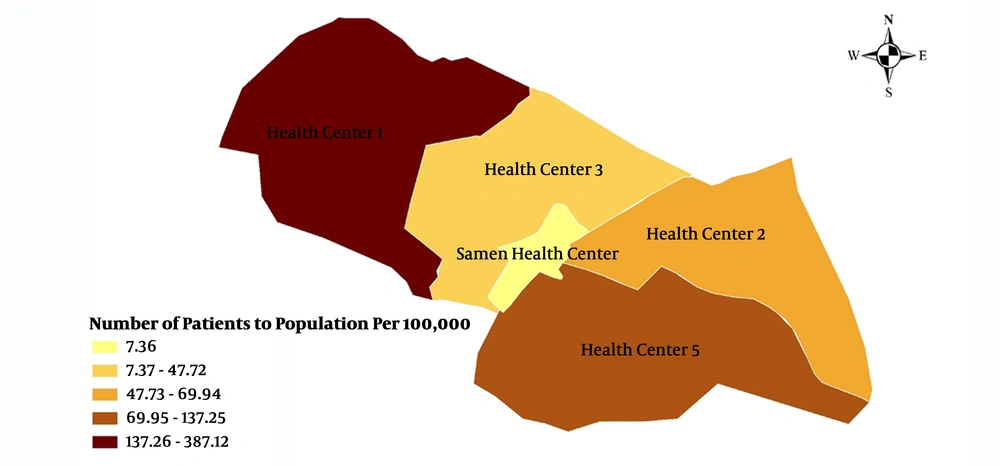
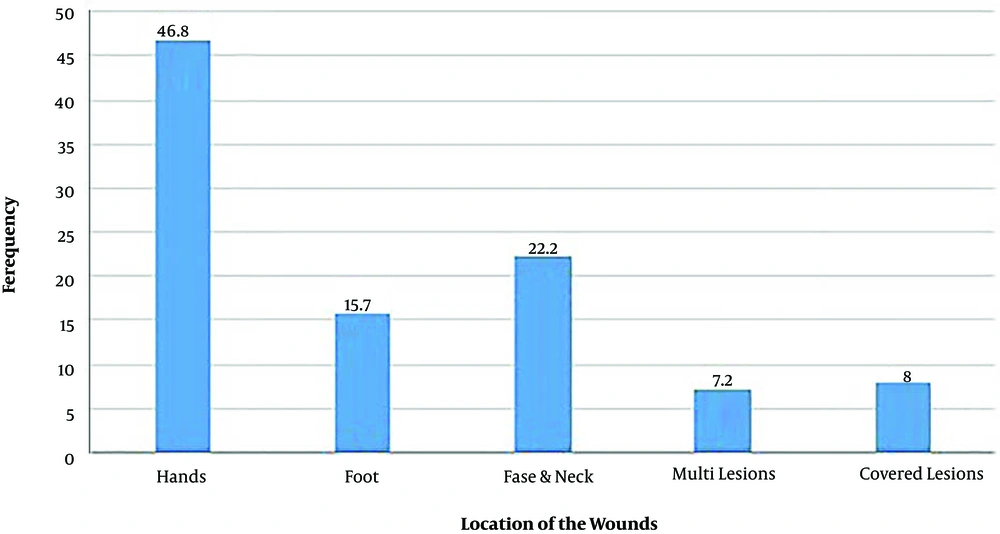
The highest prevalence rate of CL was 27.6% (n = 1445 patients), observed in 2015, and the lowest prevalence rate was 21.3% (n = 1115) in 2018 (Figure 1). The 1 - 9 year age group showed the highest incidence (21%). The distribution in different age groups (29.29 ± 20.14 years) is shown in Table 1. Totally, 2,617 (49.9%) and 2,624 (50.1%) out of 5,241 CL patients were males and females, respectively (P = 0.2) (Table 2). Besides, 1,273 (24.3%) of the patients lived in rural districts, and 3,968 (75.7%) lived in urban areas (Table 3). Leishmaniasis was more prevalent in the southwest of Mashhad than in the rest of the area (Figure 2). There were 265 (5.05%) Afghan and four (0.07%) Pakistani patients from 2015 to 2018 (Table 3). Most of the patients had one lesion on their body, and only 8% of them had multi lesions. The most frequent lesion sites were hands (47%), followed by the head and neck with a frequency of 22.2% (Figure 3). In addition, only 7.2% of the lesions were in the covered parts of the body.
| Age Group, y | Male | Female | Total |
|---|---|---|---|
| < 1 | 6 (0.2) | 8 (0.3) | 14 (0.3) |
| 1 - 9 | 570 (21.8) | 558 (21.3) | 1128 (21.5) |
| 10 - 19 | 526 (20.1) | 391 (14.9) | 917 (17.5) |
| 20 - 29 | 446 (17) | 393 (15) | 839 (16) |
| 30 - 39 | 378 (14.4) | 410 (15.6) | 788 (15) |
| 40 - 49 | 299 (11.5) | 317 (12.1) | 616 (11.8) |
| 50 - 59 | 194 (7.4) | 283 (10.8) | 477 (9.2) |
| 60 - 69 | 128 (4.8) | 157 (6) | 285 (5.4) |
| 70 - 79 | 49 (1.8) | 79 (3) | 128 (2.4) |
| > 80 | 21 (0.8) | 28 (1) | 49 (0.9) |
| Total | 2617 (100) | 2624 (100) | 5241 (100) |
aValues are expressed as No. (%).
| Year | |||||
|---|---|---|---|---|---|
| Sex | 2015 | 2016 | 2017 | 2018 | Total |
| Male | 729 (27.9) | 718 (27.4) | 599 (22.9) | 571 (21.8) | 2617 (49.9) |
| Female | 716 (27.3) | 714 (27.2) | 650 (24.8) | 544 (20.7) | 2624 (50.1) |
| Total | 1445 (27.6) | 1432 (27.3) | 1249 (23.8) | 1115 (21.3) | 5241 (100) |
aValues are expressed as No. (%).
| Variable | Male (%) | Female (%) | Total |
|---|---|---|---|
| Location | |||
| Urban | 1999 (76.4) | 1969 (75) | 3968 (75.7) |
| Rural | 618 (23.6) | 655 (25) | 1273 (24.3) |
| Nationality | |||
| Iranian | 2473 (94.5) | 2498 (95.2) | 4971(94.8) |
| Afghan | 141 (5.4) | 124 (4.7) | 265(5.05) |
| Iraqi | 1(0.01) | 0 (0) | 1(0.01) |
| Pakistani | 2 (0.1) | 2 (0.1) | 4(0.07) |
5. Discussion
Cutaneous leishmaniasis is one of the main health problems, especially in tropical and subtropical countries (2, 5). An increasing incidence of leishmaniasis has been reported in more than 98 countries in recent years (19). Despite extensive national and international efforts, on top of investments, the new foci of CL are also emerging in Iran (20).
During 2015 - 2018, 5,241 patients were diagnosed with CL in five healthcare centers in Mashhad City. The results of this study indicated that the highest frequency and the lowest frequency of CL were observed in 2015 and 2018, respectively. In recent years, we have been facing a declining trend in CL due to the implementation of control programs, including the collection of construction wastes by municipalities, installing screens on windows by health centers in endemic regions, house spraying for sand fly control, and using personal protective equipment. From 1992 to 2013, the lowest prevalence of the disease was observed in 1996 (993 patients) in this region. In 2002 and 2009, the area was in an epidemic status of about 6,000 patients each year. There were 10,533 patients recorded during four years (2010 to 2013) in Mashhad (21). Overall, the number of CL patients was decreasing according to this study in recent four years (5,241 patients from 2015 to 2018). According to another study by Norouzinezhad et al. (2016), from 2011 to 2013 in Iran, Khorasan-e-Razavi (n = 13,383), Fars (n = 13,359), and Isfahan (n = 8,786) had the highest frequency of CL, respectively. Also, the lowest prevalence was observed in Mazandaran (n = 150), Markazi/Alborz (n = 115), and West Azerbaijan (n = 90) provinces in the same years (15).
Although an insignificant correlation was observed between the place of residence and the prevalence of CL, most of the patients were from urban areas (75.7%). It seems that essential control strategies are necessary to reduce the incidence of the disease in these areas. The southwest of Mashhad had the highest number of patients, which was significantly higher than in other places (P = 0.021). This region is near a mountainous area, near to Torghabeh and Shandiz counties, which are endemic foci for CL (22). According to the obtained results, 265 Afghan and four Pakistani patients had CL during the four years of study in all health centers of Mashhad. Mashhad is known as a religious city with many pilgrimages because of the Holy Shrine of Imam Reza.
The most common sites of CL lesions were the exposed parts of the body, such as hands and faces (P < 0.001), similar to other studies (23). As a result, most lesions were seen in the unprotected parts of the body, like in other studies (24, 25). In addition, the analysis of the distribution of the wound site on the body revealed that most CL lesions were in the upper limbs of the body. The majority of the lesions on the hands and face characterize the anthroponotic form of CL, which is caused by L. tropica (9). In recent studies, L. tropica has been the dominant Leishmania species in molecular diagnostic methods in Mashhad (26). The mean prevalence of CL was decreasing in the past four years in the northeast of Iran as an important endemic region in the country.